Translate this page into:
A Case of Angiokeratoma Circumscriptum of the Tongue: Response with Carbon Dioxide and Pulsed Dye Laser
Address for correspondence: Dr. Hemanta Kumar Kar, Departments of Dermatology, STD and Leprosy, Dr. RML Hospital and PGIMER, Baba Kharak Singh Marg, New Delhi, India. E-mail: hkkar_2000@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Solitary angiokeratoma circumscriptum (AC) of the tongue is a rare entity. We present a case of solitary AC over the ventral surface of the tongue present for 3 years. The patient was treated with a combination of carbon dioxide (CO2) and pulsed dye laser (PDL). There was more than 75% improvement in the lesion after treating with alternate sessions of CO2 and PDL.
Keywords
Angiokeratoma circumscriptum
tongue
carbon dioxide laser
INTRODUCTION
Angiokeratoma is a rare, cutaneous vascular disorder that can occur under several clinically distinct conditions. It is characterized histologically by dermal vascular ectasia with overlying epidermal hyperkeratosis. Different types of angiokeratomas have been described. Although all these types differ clinically, they share similar histological features. Oral mucosal involvement is common in the systemic form, but rare if it is localized[12] Only mucosal type is uncommon and has been reported previously on few occasions.[2–5] We report a case of angiokeratoma circumscriptum (AC) of the tongue in a 12-year-old boy and its response to treatment with carbon dioxide (CO2) and pulsed dye laser (PDL).
CASE REPORT
A 12-year-old boy presented with multiple pink-to-red raised lesions over the ventral aspect of the tongue present for duration of 3 years. It started as a single raised lesion on the undersurface of the tongue which gradually increased in number and size and coalesced to form a plaque measuring approximately 3 cm. Some of the papules were also present over the lateral surface of the tongue. There was no preceding history of trauma. There was a history of bleeding from the lesion spontaneously, as well as on trauma. Approximately, there were 8–12 such episodes in a month. He denied any similar lesions elsewhere on the body.
On examination there were multiple, grouped, erythematous, shiny papules, some of which had a keratotic top, present over the ventral aspect of the anterior two-thirds of the tongue [Figure 1]. Some discrete to grouped papules were also present over the lateral edges of the tongue. They were mobile, firm and did not bleed on manipulation. Rest of the cutaneous and systemic examination was normal. All haematological and biochemical investigations were normal.

- Angiokeratoma circumscriptum on the ventral aspect of tongue; same patient with more than 75 % clearance after three alternating sessions of carbon dioxide laser and pulsed dye laser
A 2-mm biopsy of the representative tongue lesion revealed epidermal hyperkeratosis, acanthosis, papillomatosis with large dilated spaces lined by normal appearing endothelium filled with erythrocytes and organized thrombi [Figure 2]. These histological findings were consistent with diagnosis of angiokeratoma.
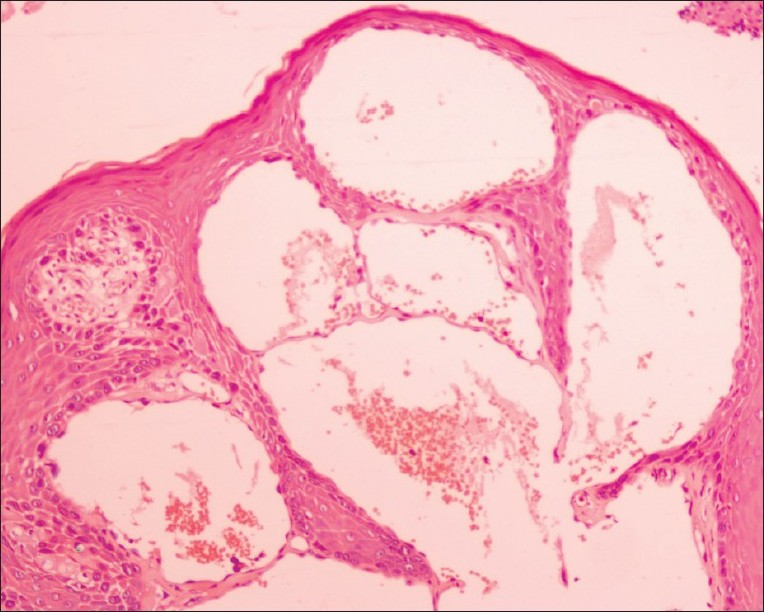
- Photomicrograph shows epidermal hyperkeratosis, acanthosis with vascular ectasia and erythrocytes in the dilated capillaries (haematoxylin and eosin, magnification, ×100)
The patient was started on a combination of CO2 and PDL. Two passes of CO2 laser (HM-30 CO2 Laser) were delivered over the lesion under local anaesthesia. A continuous wave with energy up to 5 J/cm2 to eliminate the hyperkeratotic and hypertrophic epidermis was used in the first pass. After this pass, the partially desiccated tissue was manually removed with a saline-soaked gauze, disclosing the superficial dermis with several haemorrhagic points. The second pass was delivered to achieve coagulation of the dermal vessels. Two weeks later, PDL (Q-switched Nd:YAG laser system with a separate hand piece of PDL; Medlite C6; USA) with five passes in each session was delivered to ablate the whole bulk of the lesion. Parameters used for 585 nm were maximum energy 8 J/cm2, 2 mm SS, 2 Hz RR and pulse width < 7 ns. Our PDL equipment has fixed parameters. A session of CO2 laser was followed by PDL after 2 weeks. This constituted one cycle. The next CO2 laser was repeated 2 weeks after PDL. Three such cycles were performed. Cap amoxycillin 500 mg three times daily and tab metronidazole 400 mg three times daily were administered for 1 week after every laser session. We noticed more than 75% reduction in the size of the lesion along with reduction in the bleeding episodes after treatment [Figure 1]. No adverse effect was observed. The patient was followed up for 4 months after treatment and no recurrence was found.
DISCUSSION
Angiokeratoma is a rare cutaneous vascular disorder of the papillary dermis characterized by vascular ectasia with overlying epidermal hyperkeratosis.[1]
Angiokeratomas can be divided into localized and systemic forms. The localized forms include the following: (i) solitary papular angiokeratoma that typically occurs on the lower extremities, (ii) localized angiokeratoma of the scrotum and vulva (Fordyce type), (iii) congenital form, AC naeviforme that presents as multiple hyperkeratotic papular and plaque-like lesions, usually unilaterally on the lower leg, foot, thigh, buttock or occasionally elsewhere and (iv) bilateral angiokeratomas that occur on the dorsa of the fingers and toes (Mibelli type). Generalized systemic form, angiokeratoma corporis diffusum, is usually associated with a metabolic disorder, the most common are Fabry's disease and fucosidosis.[16] Mucosal involvement, including the oral cavity, has been described both in systemic forms and as a component of localized ones. However, solitary angiokeratomas of the oral mucosa, not associated with lesions elsewhere, are rare and only few cases of isolated mucosal angiokeratomas have been reported.[2–5]
AC is a rare type of angiokeratoma characterized by aggregates of hyperkeratotic, erythematous to violaceous papules that may later become verrucous and may coalesce to form plaques. Females are commonly affected, with the male-to-female ratio being 1:3. AC may be either congenital or acquired. Lesions are usually present at birth, but in some cases may present in early childhood and adulthood.[2] Common sites are the lower extremities like leg, foot, thigh and buttock. Occasionally, they may be present elsewhere. AC may be associated with the Klippel–Trenaunay–Weber syndrome, Cobb's syndrome and other mixed vascular malformations.[7]
The pathogenesis of angiokeratoma is not clearly known. The primary event is vascular ectasia within the papillary dermis. Epidermal changes seem to be a secondary reaction. It has been speculated that the increased cell proliferation on the surface of vascular malformations and the close location of the vascular spaces with the epidermis in angiokeratoma could explain the reactive epidermal growth.[1] Pregnancy, trauma, chilblains, subcutaneous haematomas, high venous pressure and nevoid or vascular malformations are probable causative factors. Metabolic disturbance leading to weakness of the capillary wall and secondary ectasia is considered to be the primary cause for angiokeratoma corporis diffusum.[135] There was no systemic disease or local predisposing factors for the development of angiokeratomas at such an unusual site in our patient. AC of the tongue may be a distinct capillary vascular malformation.
AC may resemble a number of conditions like melanocytic nevus, malignant melanoma, verruca vulgaris, haemangioma, capillary aneurysm, Spitz nevus and pigmented basal cell carcinoma. Usually, these can be differentiated clinically, but at times a biopsy is required for diagnosis.[17] A thorough examination of the skin and mucous membranes must be performed to discard further lesions elsewhere and rule out an association with systemic diseases in widespread cases.[17]
On histology, AC has an exophytic profile, with numerous ectatic thin-walled vascular channels that expand the papillary dermis. The vascular spaces are partly or completely enclosed by elongated rete ridges, creating a basket-like or cup-shaped appearance. Thrombosis of the vessels is common and is responsible for mimicry of melanoma. The overlying epidermis encompasses the vascular spaces, often with a collarete, and displays variable degree of acanthosis and hyperkeratosis. The dermal connective tissue is generally not involved but may show a few siderophages.[17]
AC is an asymptomatic, benign, vascular malformation. Treatment is required when there is bleeding, discomfort or for cosmesis. Laser ablation or excision is the standard treatment. Laser ablation has been proven to be highly effective and may offer the best cosmetic outcome. Argon laser, Nd:YAG laser, intense pulse light, pulsed dye laser, etc., have been reported to effectively eliminate angiokeratoma, although there is a risk of scarring and hypopigmentation.[38] Also, several sessions are required with these non-ablative vascular laser systems because of the hyperkeratotic epidermal reaction in these lesions which results in a difficult access of the laser beam to target the superficial dermal vessels. The addition of ablative laser systems such as continuous wave argon or carbon dioxide laser results in better access because of the reduction in hyperkeratosis. We used a combination of carbon dioxide laser and pulsed dye laser in our case which led to more than 75% reduction in the size of the lesion after 3 months. In the follow-up period of 6 months, there was no recurrence.
A combination of the two lasers is an effective treatment option for mucosal angiokeratomas.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Oral and craniofacial findings in Fabry's disease: A report of 13 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:415-9.
- [Google Scholar]
- Vascular tumours. In: Elder D, Elenitsas R, Jaworsky C, Johnson B Jr, eds. Lever's histopathology of skin (8th ed). Philadelphia: Lippincott- Raven; 1997. p. :899.
- [Google Scholar]
- Solitary angiokeratoma of the tongue treated with diode laser. Lasers Med Sci. 2009;24:123-5.
- [Google Scholar]






