Translate this page into:
A Clinical and Dermatoscopic Perspective of the Efficacy and Safety of Erbium: YAG Laser Ablation Versus 50% Trichloroacetic Acid for the Management of Xanthelasma Palpebrarum
Address for correspondence: Dr. Aakanksha Arora, 1159, First Floor, Sector 13, Karnal 132001, Haryana, India. E-mail: akarora357@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Xanthelasma palpebrarum (XP) is a benign cosmetic condition. Although the role of CO2 laser is well described, there are only a few studies on Erbium: YAG in XP. Similarly, trichloroacetic acid (TCA) is commonly used in XP. However, there are only a few studies comparing these modalities in the treatment of XP.
Aim:
To evaluate the effectiveness and safety of Erbium: YAG laser and 50% TCA in the treatment of XP with the role of dermoscope in the evaluation of lesions.
Materials and Methods:
A total of 20 subjects were randomly allocated into two groups: group A (TCA) and group B (laser). All patients were subcategorized into three grades viz. I (mild), II (moderate), and III (severe) using a self-devised scoring system.
Results:
About 25% and 70% of patients achieved complete clearance in groups A and B, respectively (P = 0.017). The rate of recurrence was 40% and 15% in groups A and B. Dyspigmentation and erythema were the most common side effects. Pretreatment dermoscopic evaluation of the lesion showed a network of brown streaks on a background of a yellowish structureless area and was used to assess the area and margins of the lesion where the adipose tissue was found during the procedure and serial assessment of the lesion.
Keywords
Dermoscope
Erbium: YAG
trichloroacetic acid
Xanthelasma palpebrarum
INTRODUCTION
Xanthelasma palpebrarum (XP) is a benign cosmetic condition characterized by yellowish papules and plaques in the periorbital area. Treatment options for XP documented in the literature include simple surgical excision, topical trichloroacetic acid (TCA) 50% and 70% application, laser therapy, cryotherapy, etc.[1] Lasers, including the carbon dioxide laser, the argon laser, the KTP laser, the Erbium: YAG laser, and the pulsed dye laser, have been used. However, each technique is associated with its own adverse effects, such as ectropion, scarring, post-inflammatory hypo or hyperpigmentation, infection, erythema, pain and healing defects, and a high recurrence rate.[2]
One of the treatment options available for XP is the ablative laser. The suggested mechanism of action involves cutaneous vessel coagulation and heat injury to the perivascular foam cells, which prevents the accumulation of lipids into tissue.[3] Carbon dioxide laser and Erbium: YAG laser are among the commonly used ablative lasers. Although the role of CO2 laser in XP is well described in the literature, there are only a few studies on Erbium: YAG in XP.[4] Similarly, TCA is commonly used in XP.[5] However, there are only a few studies comparing these modalities in the treatment of XP.[6]
Aim and objective
This study aims to evaluate the effectiveness and safety of Erbium: YAG laser and 50% TCA in the treatment of XP, along with the role of dermoscope in the evaluation of lesions.
MATERIALS AND METHODS
A formal ethical committee approval and informed consent from patients was taken. Inclusion criteria were Fitzpatrick skin types I–IV, more than 18 years of age, the presence of one or more XP lesions on single or multiple sites, and no history of concurrent or past treatment. Exclusion criteria were active pregnancy, Fitzpatrick skin types V–VI, oral or topical retinoid use, active skin infections at the site of lesion, bleeding disorders, history of keloid or hypertrophic scar formation, recurrent herpes simplex infection, connective tissue disease and those who were not willing or available for a follow-up period of at least 3 months. A total of 40 patients were included in the study. Biochemical investigations, including blood sugar and lipid profiles, were carried out for all patients. All the subjects were randomly allocated in two groups: group A (TCA) and group B (laser). All patients were subcategorized into three grades viz. I (mild), II (moderate), and III (severe) using a self-devised scoring system of the severity of XP based on a combined score of four parameters, namely number, size, depth, and laterality of lesions used by Goel et al.[7] [Tables 1 and 2]. Grading of response to treatment was assessed as complete response (100% clearance; appearance of normal skin), partial response (>50%–99% reduction), and inadequate or no response (<50% reduction). Dermoscopy was done before treatment, during follow-up visits, and post-treatment.
| Score for each parameter | No. of lesions | Average size (mm2) | Depth of lesion | Distribution |
|---|---|---|---|---|
| 1 | <3 | <6 | Flat | Unilateral |
| 2 | 3–5 | 6–10 | Raised | Bilateral |
| 3 | >5 | >10 |
| Groups | Severity | Group A (TCA) | Group B (laser) |
|---|---|---|---|
| 1 | Mild (4–5) | 6 | 5 |
| 2 | Moderate (6–7) | 8 | 9 |
| 3 | Severe (8–10) | 6 | 6 |
In group A, a cotton-tipped applicator was moistened with 50% TCA and applied to the lesion. The endpoint was solid frosting without pink background. Repeated sessions of TCA application were given at weekly intervals till cure was achieved or up to a maximum of six sessions. In group B, the treatment area was infiltrated with lignocaine 2% with 1:100,000 adrenaline, and the eyes were protected by ocular shells. The laser model quanta system Q Plus was used. Erbium: YAG laser with wavelength 2940 nm, short pulse, fluence ranging from 2.5 to 4 J/cm2, 3 Hz, multiple passes according to lesion size. The end point of treatment was determined either by the ablation of the lesion or by the appearance of pinpoint bleeding. Subsequent sessions of laser ablation were given at 14 days intervals till cure was achieved or to a maximum of three sessions.
RESULTS
Out of 40 patients, 19 patients were male, and 21 patients were female. The age ranged from 18 to 73 years. The mean age was 47 ± 11.4 years and 43 ± 12.8 years in groups A and B, respectively. Duration of lesion varied from 1 year to 5 years (mean 2.8 ± 1.2 years). Total cholesterol and low-density lipids (LDL) were markedly raised in 92.5% and 77.5% of patients, respectively [Table 3]. However, biochemical derangements did not have any significant effects on the outcome of treatment.[8]
| Group A (50% TCA) | Group B (Er YAG laser ablation) | |
|---|---|---|
| Age distribution in years | ||
| Range | 18–72 | 18–73 |
| Mean | 47 ± 11.4 years | 43 ± 12.8 years |
| Gender distribution | ||
| Male | 9 | 10 |
| Female | 11 | 10 |
| Duration in months | ||
| Mean | 3.1 ± 1.2 years | 2.9 ± 1.5 years |
| Biochemical investigations | ||
| T cholesterol | 244.66 ± 84.59 | 238.36 ± 79.19 |
| LDL | 109.28 ± 22.02 | 111.75 ± 21.16 |
There was no significant correlation between the lesion duration and the improvement rate of lesions in both groups (P > 0.05). Similarly, there was no significant correlation between the lesion duration and complications associated with both treatment modalities (P > 0.05).
In group A, 5 of 20 (25%) patients achieved complete clearance, whereas 14 of 20 (70%) patients achieved complete clearance in group B. Overall, the difference was significant statistically (P = 0.017) between the two groups [Figure 1A].
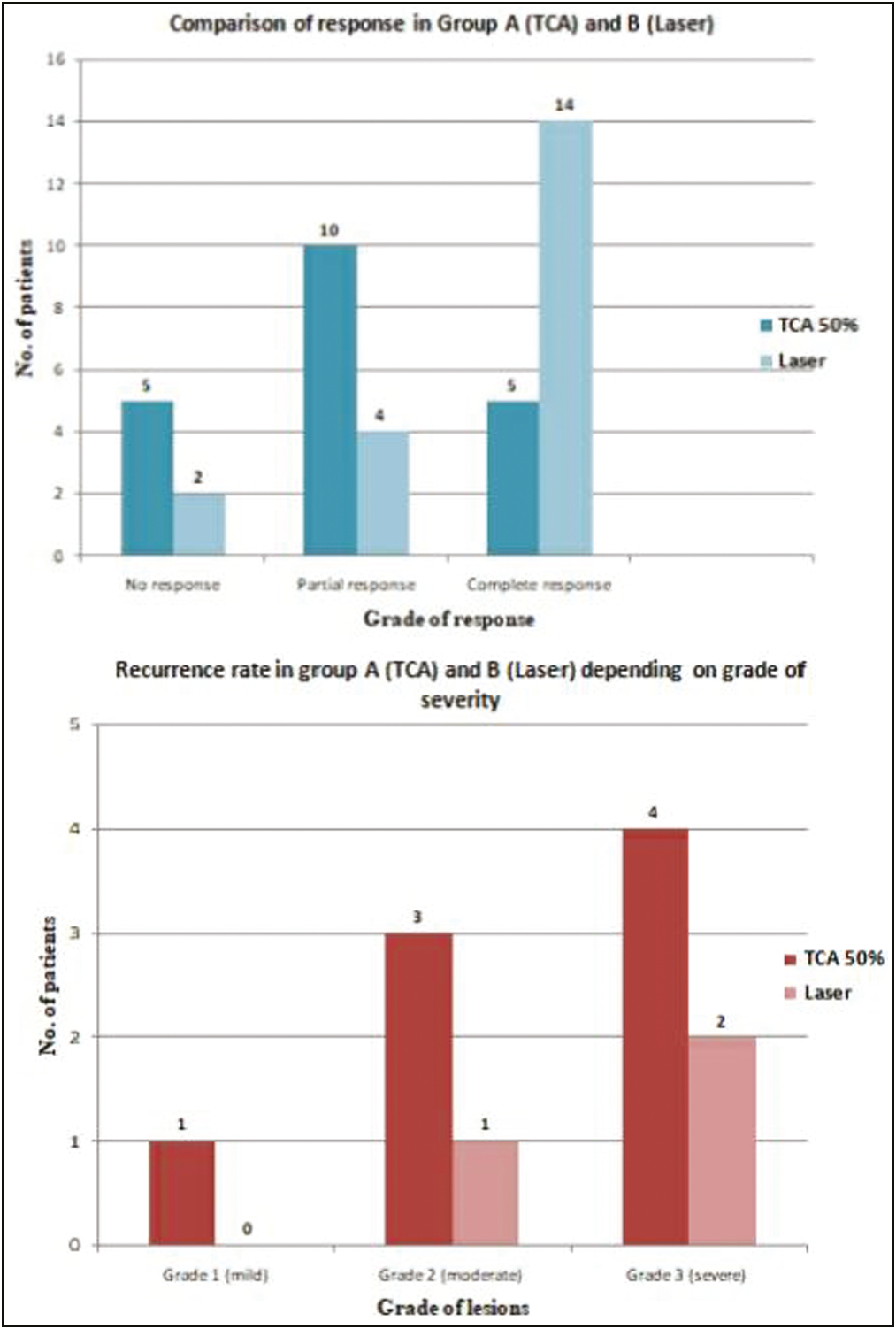
- (A) Graphical representation of a comparison of the response rate using erbium laser and TCA application; (B) comparison of the rate of recurrence in both the groups depending on the grade of severity
On subgroup analysis, the significant difference in cure rate was found for grade II (moderate) and III patients (severe), and not for patients in grade I (mild) when compared between group A (TCA) and group B (Erbium: YAG Laser) [Figure 2].

- Pre and posttreatment images of a patient with grade 3 lesion after treatment with Erbium yag laser showing complete clearance without any adverse effects
The rate of recurrence in the TCA group was 40%, while 15% in the laser group [Figure 1B]. The rate of recurrence varied with the severity of the lesion. In severe cases with an appreciable depth, laser treatment showed a better response and decreased the recurrence rate by deeper penetration.
The number of sessions was significantly lesser in the laser group (mean ± SD equal 1.35 ± 0.71) than in the TCA50% group (mean ± SD equal 2.65 ± 0.65).
Dyspigmention was the most common side effect with TCA application in 35% of cases [Figure 3]. Persistent erythema was the most common side effect noted with laser in 55% of cases. Scarring was more commonly observed in the laser group in 20% cases [Figure 4].

- Pre and posttreatment images of patients with grade 3 lesions after treatment with TCA 50% showing partial response and postinflammatory hyperpigmentation

- Pre and posttreatment images of a patient with grade 2 lesion showing scarring after treatment with Erbium yag laser
Pretreatment dermoscopic evaluation of the lesion showed a network of brown streaks on a background of a yellowish structureless area [Figure 5A]. The dermoscopy was also used to assess the area and margins of the lesion where the adipose tissue was found during the procedure and serial assessment of the lesion. It was possible to visualize a yellowish area on dermoscopy that corresponded to the site to be treated. Thus, dermoscopy allowed us to treat more objectively and minimize the possibility of inaesthetic damage. The serial assessment of lesions on follow-up visits helped to assess the presence of any remnants of adipose tissue in both groups [Figure 5B]. Resolving lesions showed a white structureless area with or without a yellowish rim and surrounding.
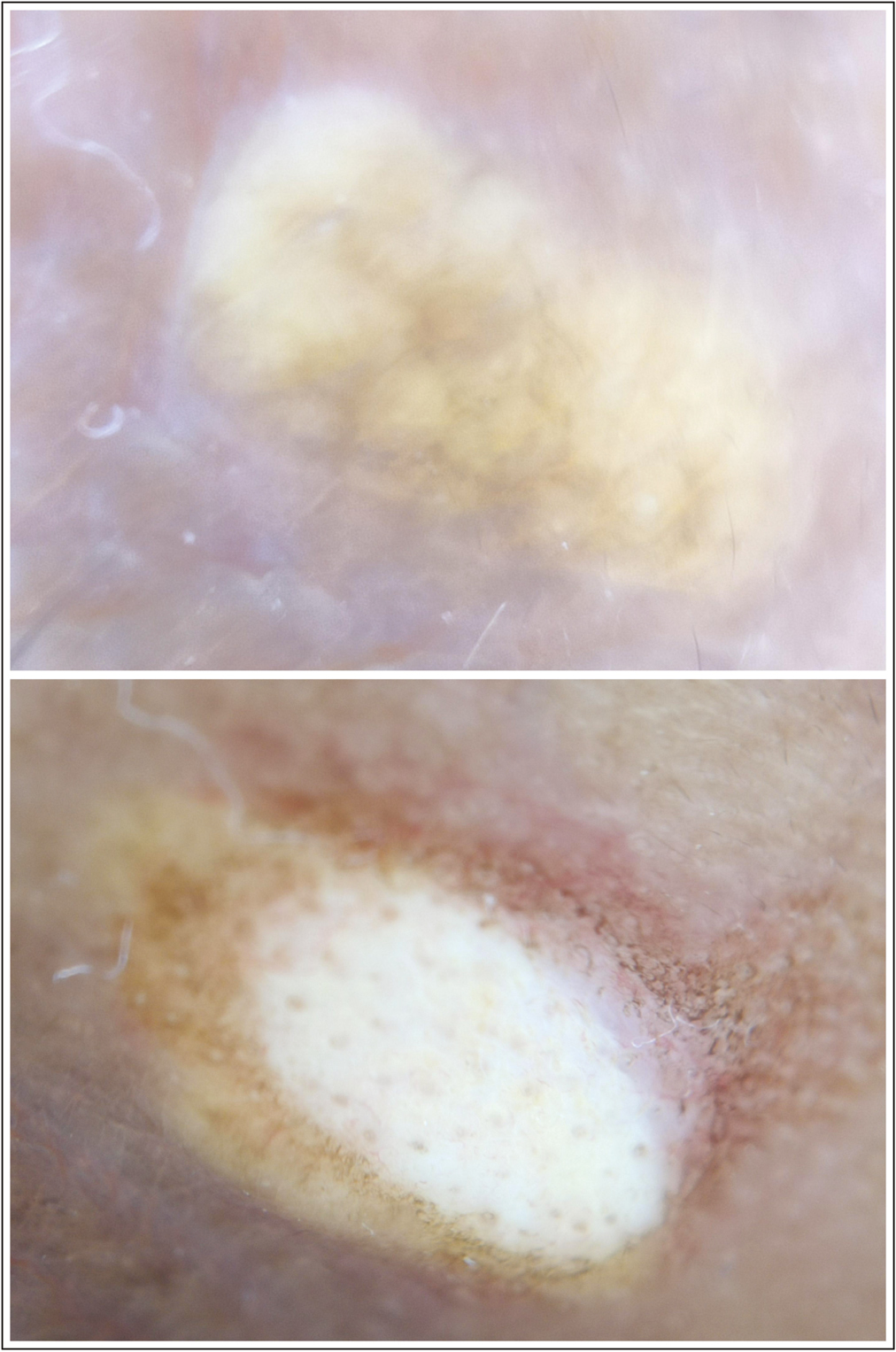
- (A) Dermoscopic image of xanthelasma palpebrarum before treatment showing the network of brown streaks on a background of the yellowish structureless area; (B) the dermoscopic image of a lesion at 2 weeks follow-up showing remnants of adipose tissue along the margins
DISCUSSION
XP is a common cosmetic problem. It results from the collection of xanthoma cells, which are lipid-rich histiocytes, invading the superficial dermis and brings about fibrosis and inflammation.[1] XP therapy is considered a purely aesthetic technique. There are many different treatment choices, but there is still disagreement over the best one in terms of effectiveness and adverse effects. The role of TCA and Erbium: YAG laser has already been described individually in the literature.[59] However, there is a scarcity of data on the comparative evaluation of these two modalities in XP.
In the present study, we compared Erbium: YAG laser against TCA 50% in XP therapy. At the end of our study, all xanthelasma lesions were efficiently removed by Erbium: YAG laser as compared to TCA 50% with statistically significant improvement in lesions. Our study also demonstrated that the number of sessions was significantly lesser for the laser group. The rate of recurrence was higher in the TCA group. In a study of Gungor et al.[6] of patients with xanthelasma, Erbium: YAG laser ablation and 70% TCA application were performed in different XP lesions of the same patient. They reported that 70% of TCA applications and Erbium: YAG laser ablation methods have similar effectiveness and complication rates.
In our study, we subclassified the patients based on the severity of their lesions into three grades. Grade 1 (mild) lesions were efficiently treated with both modalities. However, the Erbium: YAG laser showed better results in grade 2 (moderate) and grade 3 (severe) lesions.
With a wavelength of 2940 nm, the Erbium: YAG laser ablates just a few layers of skin with limited collateral thermal damage of peripheral tissue. Another mechanism implicated in xanthelasma laser surgery is the coagulation of the hyperpermeable vessels leading to damage of the perivascular foam cells and also prevents leakage of lipids into the tissue.[10] Additionally, it enables superior depth control and exact ablation of the tissue in delicate areas. It reduces therapy side effects because it is not extremely intrusive.[610] However, if the subcutaneous tissue is mistakenly damaged, there is a minor risk of scarring, and in a few instances, postoperative hyperpigmentation of the treated area has been reported. In the present study, 20% cases presented with scarring post-laser treatment. Disadvantages of Erbium: YAG laser includes high maintenance and expense of the equipment.[6]
The mechanism of action of TCA includes superficial coagulation of skin proteins leading to the destruction of the epidermis and upper papillary dermis.[11]
In the present study, there was a significant increase in post-therapy hyperpigmentation in 25% patients and hypopigmentation in 10% patients treated with TCA 50%. Nahas et al.[12] described the occurrence of hypopigmentation in TCA-treated patients as a complication of the deep cauterization damaging the melanin of the hair follicles.
The recurrence rate depends on the level of involvement of deeper layers and the extent of clean resection. Al-Kady et al.[13] reported a high recurrence rate in patients treated with TCA 50% as compared to CO2 laser because the depth of penetration cannot be adequately controlled with TCA. In our study, the recurrence rate was much more in the TCA group as compared to the laser.
Our study is the first of its kind to comment on the dermoscopic findings of XP and assess its role in management.
CONCLUSION
The results of this study show that Erbium: YAG laser ablation has more effectiveness and less complication rates, especially in thick and large lesions, and has a lower recurrence rate. However, TCA application is equally effective in the treatment of mild XP lesions. Dermoscopy can be used as an auxiliary tool in the treatment of xanthelasma by assessing the depth and extent of ablation. Recurrence is a major problem with all treatment approaches. Depth, size, and extent of the lesion are the key factors determining recurrence. Therefore, it is crucial to have a uniform grading system to compare different modalities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Xanthelasma palpebrarum: A review and current management principles. Plast Reconstr Surg. 2002;110:1310-4.
- [Google Scholar]
- Xanthelasma palpebrarum—A brief review. Clin Cosmet Investig Dermatol. 2017;11:1-5.
- [Google Scholar]
- The use of short and variable pulse Erbium: Yttrium-Aluminum-Garnet laser in dermatology and cosmetic surgery: Review. Turkiye Klinikleri J Dermatol. 2011;21:130-9.
- [Google Scholar]
- CO2 and erbium: YAG laser in eyelid surgery: A comparison. Ophtalmologe. 2000;97:835-41.
- [Google Scholar]
- Evaluation of three different strengths of trichloroacetic acid in xanthelasma palpebrarum. J Dermatol Treat. 2006;17:48-50.
- [Google Scholar]
- YAG laser ablation versus 70% trichloroacetıc acid application in the treatment of xanthelasma palpebrarum. J Dermatolog Treat. 2014;25:290-3.
- [Google Scholar]
- A prospective study comparing ultrapulse CO2 laser and trichloroacetic acid in the treatment of Xanthelasma palpebrarum. J Cosmet Dermatol. 2015;14:130-9.
- [Google Scholar]
- Xanthelasma palpebrarum—Clinical and biochemical profile in a tertiary care hospital of Delhi. Indian J Clin Biochem. 2007;22:151-3.
- [Google Scholar]
- Xanthelasma palpebrarum: Treatment with the erbium: YAG laser. Lasers Surg Med. 2001;29:260-4.
- [Google Scholar]
- Systematic review of laser therapy in xanthelasma palpebrarum. Int J Dermatol. 2017;56:e47-55.
- [Google Scholar]
- Assessment of efficacy and tolerability of different concentrations of trichloroacetic acid vs. carbon dioxide laser in treatment of xanthelasma palpebrarum. J Cosmet Dermatol. 2015;14:209-15.
- [Google Scholar]
- Treatment of eyelid xanthelasma with 70% trichloroacetic acid. Ophthal Plast Reconstr Surg. 2009;25:280-3.
- [Google Scholar]
- Fractional CO2 laser versus trichloroacetic acid 50% for xanthelasma palpebrarum therapy. J Cosmet Dermatol. 2021;20:763-8.
- [Google Scholar]






