Translate this page into:
A Comparative Study between Autologous Noncultured Trypsinized Melanocytes–Keratinocytes Cell Suspension and Autologous Noncultured Nontrypsinized Epidermal Cells Grafting (Jodhpur Technique) in Stable Vitiligo
Address for correspondence: Dr. Dilip Kachhawa, Department of Skin and Venereal Diseases, Dr. SN Medical College, Shastri Nagar, Near Mathura Das Mathur Hospital, Jodhpur 342003, Rajasthan, India. E-mail: drdilipkachhawa@hotmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Noncultured epidermal cell suspension (NCES) and Jodhpur technique (JT) are two treatment options in vitiligo, in which the basic principle is the transfer of melanocytes from uninvolved skin to stable vitiligo patch in the form of either tissue graft or cellular graft.
Objectives:
The aim of this study was to evaluate effectiveness of two different treatment methods (NCES and JT) in stable vitiligo.
Materials and Methods:
This was a randomized comparative study, which included 45 patients with 153 stable vitiligo patches. Cases were randomly divided into two groups. Appropriate statistical analysis was done. A value of P < 0.05 was considered statistically significant.
Results:
Of 45 cases, female-to-male ratio was 1.36:1. Mean duration of disease and stability were found to be 10.44 ± 5.24 and 3.83 ± 2.31 years, respectively. Mean size of treated area for NCES and JT was 10.11 ± 10.31 and 10.13 ± 10.29 cm2, respectively. Earliest repigmentation was found at 3 weeks in NCES and 6 weeks in JT. At 6 weeks, repigmentation was better in NCES, whereas later JT showed better pigmentation. Follow-up was done at 8 days and 6, 10, 14, and 24 weeks. With respect to color match at 6 weeks, JT was found superior; however, at 24 weeks both showed similar efficacy. Mean reduction in daily life quality index was significantly decreased post-surgery.
Limitations:
This was a single-center, small sample size study.
Conclusion:
Melanocyte plus keratinocyte cell transfer is very effective in the treatment of stable vitiligo. On the basis of the results, JT may show significant contribution in vitiligo.
Keywords
Color match
JT (Jodhpur technique)
NCES (noncultured epidermal cell suspension)
repigmentaion
INTRODUCTION
Worldwide prevalence of vitiligo is approximately 1%, whereas in India it is approximately 3%–4% ranging from 0.46% to 8.8%.[12] Etiopathogenesis of vitiligo is multifactorial consisting of immunological, genetic, and environmental factors. Stability for more than 1-year duration is required for surgical treatment option.[34] The basic principal surgical method is the transfer of melanocytes from uninvolved skin to the stable vitiligo patch in the form of either tissue graft or cellular graft. Among these surgical options, this randomized study is planned to compare the outcome of two surgical modalities: one is autologous noncultured trypsinized melanocytes plus keratinocytes cell suspension (noncultured epidermal cells suspension; NCES) and the other is autologous noncultured nontrypsinized epidermal grafting (Jodhpur technique [JT]) in stable vitiligo patients in terms of extent of repigmentation, color matching of repigmented area, any perilesional white rim after transplantation, and any adverse events at both recipient and donor sites. This may be the first study in the literature that compares these two new cellular grafting techniques.
AIMS AND OBJECTIVES
To evaluate the efficacy of grafting techniques (NCES and JT) in the treatment of stable vitiligo patches.
To compare the effectiveness of two surgical methods (NCES and JT) using following parameters: (a) extent and pattern of repigmentation, (b) color matching of repigmented area, (c) adverse effects, and (d) patient satisfaction (daily life quality index [DLQI] questionnaire and patient global assessment).
To evaluate safety of two surgical methods (NCES and JT).
MATERIALS AND METHODS
This was a hospital-based interventional, randomized, comparative study conducted in Department of Dermatology, Venereology, and Leprosy, Dr. SN Medical College and Hospital, Jodhpur, Rajasthan, India. Approximately 45 patients with 153 stable vitiligo patches were included over a period of 1 year. It was patient-blinded study.
Written informed consent was taken from the patients, who were enrolled from the outdoor of Mathura Das Mathur Hospital after fulfilling the inclusion criteria. These were subjected to both vitiligo surgery (NCES and JT). Cases were randomly divided into two groups; Group I and Group II using randomization table. Group I comprised of 76 stable vitiligo patches, treated by noncultured trypsinized epidermal cell suspension (NCES) and Group II included 77 stable vitiligo patches, treated by Jodhpur technique (NCNTMKT/JT).
Inclusion criteria
The inclusion criteria of the study included the subjects with a clinical diagnosis of vitiligo that has been stable for a minimum of 1 year and not responding to medical treatment or residual patches of vitiligo vulgaris after medical therapy.
Exclusion criteria
The exclusion criteria of the study included the following:
Age less than 18 years and more than 40 years
Pregnancy and lactation
Patient with active spreading vitiligo
History of koebnerization
History of hypertrophic scars or keloidal tendency
Bleeding disorders
Patients with unrealistic expectation.
At the first visit, a proforma was filled noting the baseline characteristics, history, and examination findings. Patients were asked to fill DLQI questionnaire, which was designed by Dr. Finlay. We also carried out patient’s global assessment with the help of a patient satisfaction questionnaire including three questions: “grade the change in pigmentation in the transplanted area,” “are you satisfied with the treatment?,” and “do you find the treatment worthwhile?” Patients were asked to answer in terms of scoring from 0 to 10.
Technique of transplantation
Donor site was selected usually on noncosmetically important sites like the thighs, buttocks, or waist. Size of graft was approximately one-fourth to one-third of the recipient site.
In NCES, an ultrathin split thickness skin graft was taken with the help of a shaving blade and transferred to a container with normal saline. Dermabrasion was done until tiny pinpoint bleeding spots were seen (dermo-epidermal junction). Dermabrasion was extended 2 mm beyond margins to prevent halo phenomenon. Suspension was spread evenly on recipient area and extended 2 mm beyond it. The skin graft was transferred to trypsin-EDTA solution at 37°C for 45 min, then antitrypsinization was done. The separated epidermal parts were centrifuged for 6 min at 3000 rpm. This settled down pellets were transferred to recipient site.
In Jodhpur technique, hair was shaved off followed by painted by povidone-iodine and 2% lidocaine was infiltrated. Later antibiotic ointment (mupirocin) was applied. Dermabrasion was done with the help of dermabrader at slow rpm till pinpoint bleeding which meant the area appeared whitish (i.e., upper dermis) then paste-like material containing epidermal components (melanocytes and keratinocytes) was obtained with spatula and spread over the recipient site. Recipient site was prepared in the same manner as donor site except no harvesting of epidermal particles was done. Three-layer dressing (including collagen dressing) was done with antibiotic-soaked gauzes at both donor and receipt sites to prevent sticking of gauze to graft material.
The patient was asked to lie down for 30 min after the procedure and then allowed to go home. Suitable antibiotics and analgesics were prescribed. The dressing was removed after 7 and 14 days from the recipient site and donor site, respectively, and antibiotic ointment was applied for at least 2 weeks.
Follow-up was done at day 8, week 6, 10, 14, and 24, and repigmentation was assessed subjectively by digital photography. Psoralen plus UVA radiation therapy was given after 3 weeks in both groups.
Extent of repigmentation was assigned as poor, fair, good, and excellent for <50%, 50%–74%, 75%–89%, and 90%–100% repigmentation.
Repigmentation pattern was noted as “diffuse,” “perifollicular,” “dotted,” or “marginal.” Color matching of repigmented skin was categorized as “somewhat lighter than,” “same as,” or “somewhat darker than” normal skin.
No oral immunosuppressant was used before and after procedure.
Statistical analysis was performed with the plymouth routines in multivariate ecological research and statistical package for social sciences, Tril version 20.0 for Windows statistical software package (SPSS, Chicago, Illinois). The categorical data were presented as numbers (percent) and were compared among groups using Chi-square test. Groups were compared for demographic data, presented as mean and standard deviation and were compared using by Student’s t test. A value of P < 0.05 was considered statistically significant.
RESULTS
Forty-five patients with a total of 153 lesions with a clinical diagnosis of stable vitiligo were included in the study. Females outnumbered males with female-to-male ratio of 1.36:1. The youngest patient was 18 years old and the oldest one was 40 years.
Mean duration of disease in men was 10.37 ± 3.80 years and in women 10.50 ± 6.15 years with overall mean duration of disease was 10.44 ± 5.24 years. Likewise, the mean duration of stability of vitiligo for men and women was 4.03 ± 2.12 years and 3.69 ± 2.46, respectively.
Vitiligo vulgaris was the most common type ([46, 60.5%] [47, 61%]) followed by focal (17, 17) and segmental vitiligo (13, 13), in JT and NCES, respectively. No significant difference was observed between the groups based on type of vitiligo (P = 0.98).
The mean size of treated area for NCES was 10.11 ± 10.31 cm2 and for JT 10.13 ± 10.29 cm2 (P = 0.818). All treated lesions were widely distributed all over the body (P = 0.891).
Ankle (26 patch), elbow (8 patches), foot (12 patches), finger (3 patches), and face (6 patches) are considered as difficult to treat sites. So we included vitiligo lesions present over both ordinary sites and difficult to treat sites.
Postoperative course
Earliest repigmentation was noted at 6 weeks of post-surgery. The donor site was also completely reepithelialized by the time of dressing removal, gradually pigmented.
According to Table 1, at 6 weeks results were better in NCES than in JT, which were comparable and found statistically significance (P ≤ 0.05). Later, over the period of time, JT showed better pigmentation than NCES, which were also statistically significant as p value for all 10, 14, and 24 weeks was <0.05.
| Extent of repigmentation | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Extent of repigmentation | 6 weeks FU | 10 weeks FU | 14 weeks FU | 24 weeks FU | ||||||||
| NCES | JT | Total | NCES | JT | Total | NCES | JT | Total | NCES | JT | Total | |
| No | 1 | 3 | 4 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 |
| Poor | 12 | 41 | 53 | 1 | 2 | 3 | 0 | 1 | 1 | 0 | 0 | 2 |
| Fair | 44 | 21 | 65 | 18 | 38 | 56 | 13 | 23 | 36 | 4 | 1 | 10 |
| Good | 16 | 12 | 28 | 43 | 31 | 74 | 26 | 31 | 57 | 19 | 7 | 42 |
| Excellent | 3 | 0 | 3 | 14 | 5 | 19 | 37 | 21 | 58 | 53 | 69 | 99 |
| P Value | <0.05 | <0.05 | <0.05 | <0.05 | ||||||||
| Color match with surrounding skin | ||||||||||||
| Color match with surrounding skin | 6 weeks FU | 10 weeks FU | 14 weeks FU | 24 weeks FU | ||||||||
| NCES | JT | Total | NCES | JT | Total | NCES | JT | Total | NCES | JT | Total | |
| Dark | 31 | 13 | 44 | 21 | 10 | 31 | 13 | 4 | 17 | 2 | 3 | 5 |
| Light | 2 | 1 | 3 | 1 | 1 | 2 | 1 | 0 | 1 | 0 | 0 | 0 |
| Same | 43 | 63 | 106 | 54 | 66 | 120 | 62 | 73 | 135 | 74 | 74 | 148 |
| P Value | <0.05 | 0.07 | <0.05 | 0.66 | ||||||||
At weeks 24, in 74 lesions each in NCES (97%) and JT group (96%), the color of the repigmented area matched excellently with the normal surrounding skin [Table 1].
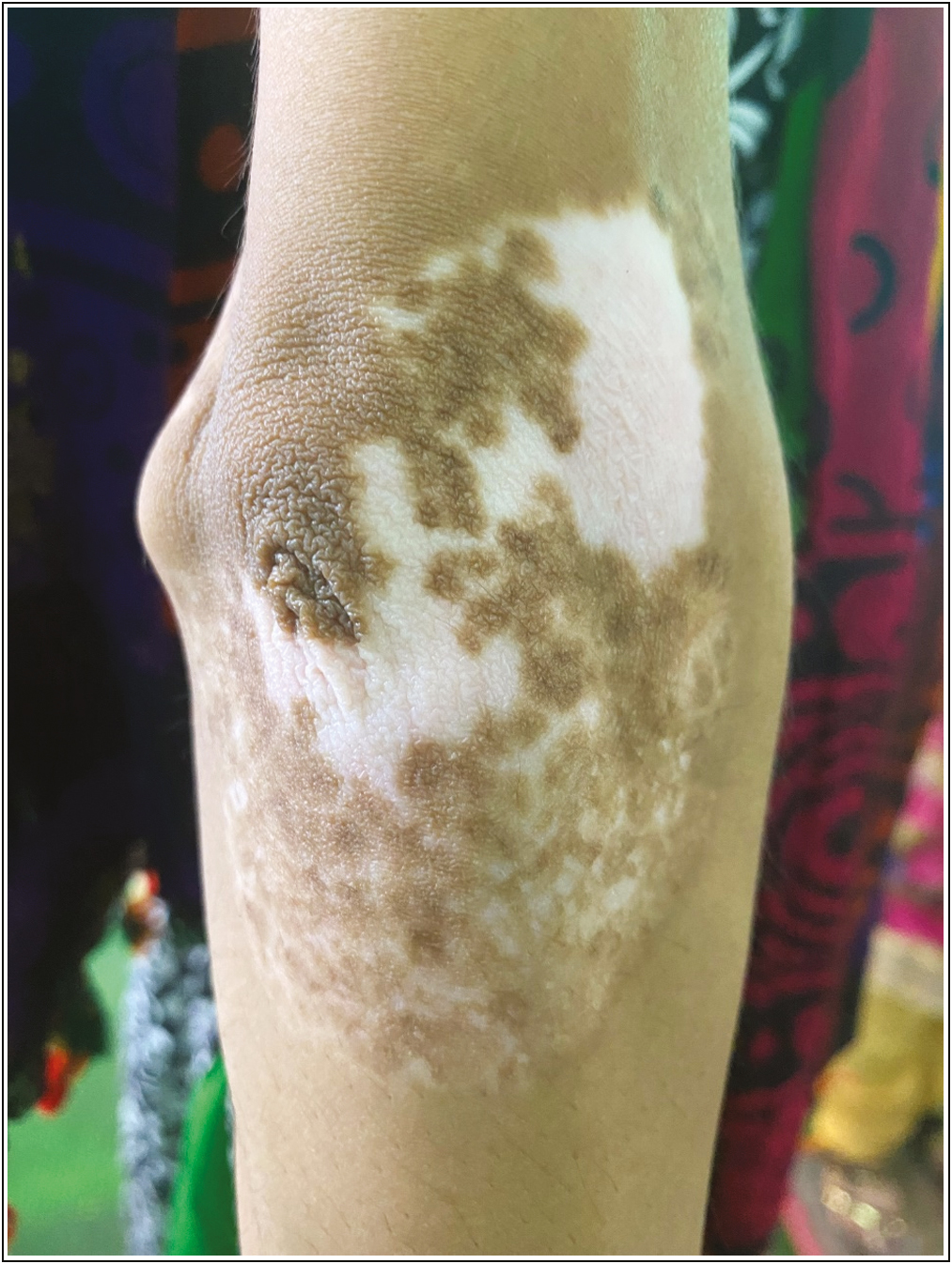
Diffuse repigmentation was the most common pattern of repigmentation observed in 106 (69%) of overall lesions ([57, 75%; NCES], [49, 64%; JT]). Perifollicular, marginal, and dotted repigmentation were observed in 6 (7%), 7 (9%), and 6 (7%) lesions in the NCES group and 8 (10%), 9 (11%), and 11 (14%) lesions in the JT group (P = 0.45) [Figures 1–5].

- Stable vitiligo patch on the right elbow and lower part of arm prepared for JT (preprocedure)

- Stable vitiligo patch on the right elbow and lower part of arm showed >75% repigmentation after JT at 16 weeks (post-procedure)

- Vitiligo patch showing paste-like material covering the site in JT (during procedure)

- Stable vitiligo patch on elbow of right arm preparing for NCES (preprocedure)
- Stable vitiligo patch showed >70% repigmentation after NCES at 16 weeks (post-procedure)
Daily Life Quality Index
DLQI reduced from a mean value of 12.89 ± 5.00 before surgery to 1.29 ± 1.16 after surgery. The mean reduction in DLQI was significantly greater in post-surgery cases (P ≤ 0.05).
Patient satisfaction
Patients in both groups were highly satisfied with the treatment outcomes. Mean values of Patient Satisfaction Questionnaire (PSQ)1, PSQ2, and PSQ3 were 8.59 ± 1.10, 8.68 ± 1.15, and 8.84 ± 1.21 after surgery. Overall PSQ-4 score was 138/153 (in 138 patches, patients wanted to choose this treatment again) (71/5; NCES, 67/10; JT).
Adverse events
In both groups, no significant side effects were seen at the donor and recipient sites (P ≤ 0.05/0.54) [Tables 2 and 3].
| Complication (D) | NCES (D) | JT (D) | Total (D) | P Value (D) |
|---|---|---|---|---|
| No complication | 25 | 45 | 70 | <0.05 (significant) |
| Hyperpigmentation | 13 | 9 | 22 | |
| Hypopigmentation | 20 | 12 | 32 | |
| Scarring | 11 | 7 | 18 | |
| Milia | 7 | 4 | 11 |
D = donor
| Complication (D) | NCES (R) | JT (R) | Total (R) | P Value (R) |
|---|---|---|---|---|
| No complication | 47 | 56 | 103 | 0.54 (not significant) |
| Hyperpigmentation | 14 | 11 | 25 | |
| Perilesional halo | 9 | 4 | 13 | |
| Delayed repigmentation | 4 | 4 | 8 | |
| Milia | 2 | 2 | 0 |
R = recipient, D = donor
DISCUSSION
Both NCES and JT have an advantage that they permit treatment of affected skin manifold larger than the donor area. JT is a simpler and cheaper method requiring minimal infrastructure including instruments and chemicals.
However, this is the only study done between trypsinized and nontrypsinized cellular transplant methods in literature till date. Our study showed preponderance of females, which was probably the result of greater cosmetic awareness and social stigma of disease in females.
Njoo et al.[5] collected 39 studies, using various surgical methods in vitiligo. The highest success rates were achieved with split-thickness grafting (87% [95% CI, 82%–91%]) and epidermal blister grafting (87% [95% CI, 83%–90%]). The lowest success rate was reported with noncultured epidermal suspension method (31% [95% CI, 11%–59%]). Reason behind this outcome can be explained as patients in the noncultured epidermal suspension group were too little to draw a firm conclusion, and this was carried out in year 1998, when NCES method was still in its early stage of development.
As this is the first study of its kind, some Indian authors did tremendous work in the field of vitiligo surgeries. Gupta et al.[6] conducted a study in 143 patients related to epidermal blister grafting in vitiligo. Khunger et al.[7] described various tissue graft in vitiligo surgery.
Paul[8] conducted a study on epidermal cell suspension using retrospective analysis in 58 patients.
Olsson and Juhlin[9] conducted a study to investigate the responses in vitiligo to three surgical methods: autologous cultured melanocytes, ultrathin epidermal sheets, and basal cell layer suspension. In our study, we could get fair-good repigmentation at fingers with either of the method because these areas were not completely resistant to surgery.
According to the extent of repigmentation, we found excellent response in 70% lesions in the NCES group and 90% lesions in the JT group. So JT was found significantly superior to NCES in producing excellent repigmentation. However, a good extent of repigmentation was obtained approximate equally in both techniques.
We used very simplified method in vitiligo surgery in JT, described by Kachhawa et al.[10] Pandya et al.[11] reported an excellent response in 52.17% cases with noncultured epidermal suspension technique and in 50% with the melanocyte culture technique. In NCES, we followed the method of graft harvesting described by Behl using a sterile razor blade mounted on a straight artery forceps for taking ultrathin graft.
Gauthier and Surleve-Bazeille[12] had observed 70% repigmentation in 63.6% of the vitiligo patients treated by noncultured melanocyte transplantation. They had included only patients of focal and segmental vitiligo.
Van Geel et al.[13] utilizing the modified procedure reported 70% repigmentation in 62% of the 40 patients. It is important to note that in addition he used phototherapy (narrow band UVB or Psoralen plus UVA radiation), topical steroids, and calcipotriol in postoperative period for all patients.
Mulekar[14] in his study found that in the segmental and focal vitiligo group, 84% and 73% patients showed excellent pigmentation. He found that more than 50% of patients treated for difficult sites showed more than 65% repigmentation of the treated areas by noncultured epidermal suspension. According to Olsson and Juhlin,[9] a significant repigmentation was observed in 70% of patients.
While considering time taken for repigmentation, we found that ≥75% repigmentation was seen in 57% lesions in the NCES group and 40% lesions in the JT group at 10 weeks. This was an important difference between both cellular transfer techniques as described earlier. But at 14 and 24 weeks of follow-up, 83% and 95% out of 76 lesions, respectively, in the NCES group and 68% and 90% lesions out of 77 lesions, respectively, in the JT group reached ≥75% repigmentation.
Reason for faster repigmentation in NCES can be explained by the hypothesis suggested by Gauthier et al.[12] that in trypsinized graft, epidermal suspension has higher melanocyte concentration, and this help in faster early repigmentation. On the other hand, there was evenly spread of repigmentation achieved in early time because of the little resistance to pigment spread in epidermis.
In JT, the concentration of melanocytes in suspension is lower than in a trypsinized graft. So, the initial speed of repigmentation is slow. But, as the melanocytes repopulate at the recipient site evenly, the final outcome is better in terms of the extent of repigmentation. Keratinocytes are also transferred along with melanocytes in JT that help in the growth and survival of melanocytes.
The most commonly observed pattern of pigmentation in both groups was a diffuse pattern. This signifies that the repigmentation was due to transplanted melanocytes by NCES and JT. Perifollicular or marginal repigmentation is mainly induced by the melanocytes reserve in the hair follicle, which is stimulated by dermabrasion or phototherapy that was less in both groups.
Minor side effects were observed. Few patients exhibited postoperative hyperpigmentation at donor site which also vanished over time. Complications at donor site were statistically significant in both groups. At recipient site, hyperpigmentation and perilesional halo were more common in the NCES group while delayed repigmentation was equal in both groups.
We observed a significant reduction in DLQI after surgery. A similar improvement in DLQI score has been previously reported by Van Geel et al.[13] Reduction in DLQI was significantly decreased after surgery for both groups. PSQ score was also significantly higher after surgery. Early repigmentation noticed in NCES with color exactly matched with surrounding skin while in JT repigmentation started late and color matching slightly differed than NCES. Therefore, patients in the NCES group were significantly much more satisfied than those in the JT group.
Our study is the first of its kind in the literature to evaluate a new cellular transplantation technique (JT) in vitiligo to compare with a well-established cellular transplantation technique (NCES). Cellular transplantation techniques have been found to be sophisticated, costly, require laboratory, and somewhat difficult to be performed at the clinic. But we used a very cheaper technique of JT without any melanocyte culture media, any sophisticated, or costly apparatus.
We took into consideration patient satisfaction and improvement in DLQI, which are important parameters to consider in a psychologically disabling disease such as vitiligo especially since it has been reported that extent of repigmentation may not correlate directly with patient satisfaction and improvement in the quality of life.
Our study indicates that both NCES and JT are safe and effective techniques in terms of good and excellent repigmentation, color match but NCES is superior to JT in term of patient satisfaction and DLQI reduction.
However, a further molecular-level research is still needed to elaborate the factors impeding pigment spread in JT and the factors provided by keratinocytes for the growth and survival of melanocytes in JT.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The definition and assessment of vitiligo: A consensus report of the vitiligo European task force. Pigment Cell Res. 2007;20:27-35.
- [Google Scholar]
- Standard guidelines of care for vitiligo surgery. Indian J Dermatol Venereol Leprol. 2008;74:37-e45.
- [Google Scholar]
- Compendium of clinico-epidemiological features. Indian J Dermatol Venereol Leprol. 2007;73:149-56.
- [Google Scholar]
- A systematic review of autologous transplantation methods in vitiligo. Arch Dermatol. 1998;134:1543-9.
- [Google Scholar]
- Epidermal grafting in vitiligo: Influence of age, site of lesion, and type of disease on outcome. J Am Acad Dermatol. 2003;49:99-104.
- [Google Scholar]
- Tissue grafts in vitiligo surgery—Past, present, and future. Indian J Dermatol. 2009;54:150-8.
- [Google Scholar]
- Autologous non-cultured basal cell-enriched epidermal cell suspension transplantation in vitiligo: Indian experience. J Cutan Aesthet Surg. 2011;4:23-8.
- [Google Scholar]
- Long-term follow-up of leucoderma patients treated with transplants of autologous cultured melanocytes, ultrathin epidermal sheets and basal cell layer suspension. Br J Dermato. 2002;147:893-904.
- [Google Scholar]
- Keratinocyte-melanocyte graft technique followed by PUVA therapy for stable vitiligo. Indian J Dermatol Venerol Leprol. 2008;14:622-24.
- [Google Scholar]
- A study of autologous melanocyte transfer in treatment of stable vitiligo. Indian J Dermatol Venereol Leprol. 2005;71:393-7.
- [Google Scholar]
- Autologous grafting with noncultured melanocytes: A simplified method for treatment of depigmented lesions. J Am Acad Dermatol. 1992;26:191-4.
- [Google Scholar]
- Modified technique of autologous noncultured epidermal cell transplantation for repigmenting vitiligo: A pilot study. Dermatol Surg. 2001; 27:873-6.
- [Google Scholar]
- Long-term follow-up study of segmental and focal vitiligo treated by autologous, noncultured melanocyte-keratinocyte cell transplantation. Arch Dermatol. 2004;140:1211-5.
- [Google Scholar]






