Translate this page into:
A comparative study of 70% glycolic acid and 30% trichloroacetic acid peel in the treatment of facial atrophic acne scars: A split-face study
*Corresponding author: Pravesh Yadav, Department of Dermatology, Venereology and Leprosy, Dr. Baba Saheb Ambedkar Medical College and Hospital, New Delhi, India. rao.pravesh@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Manjhi M, Sagar V, Yadav P, Dabas G, Gupta A, Pratap P. A comparative study of 70% glycolic acid and 30% trichloroacetic acid peel in the treatment of facial atrophic acne scars: A split-face study. J Cutan Aesthet Surg. 2024;17:227-33. doi: 10.25259/jcas_117_23
Abstract
Objectives:
Medium-depth peels are dynamic tools when used as part of office procedures for the treatment of acne scars. Most of the available literature on chemical peels focuses on their role in skin rejuvenation and hyperpigmentation. There is a paucity of well-conducted studies that have compared peels in the treatment of acne scars in Asian patients.
Material and Methods:
The study aimed to compare the efficacy of 70% glycolic acid (GA) and 30% trichloroacetic acid (TCA) chemical peels in the treatment of facial atrophic acne scars. A longitudinal, right-left study was conducted to assess the effectiveness and side effects of 70% GA and 30% TCA in 30 patients with acne scars. A total of four peeling sessions were performed every 4 weeks. Evaluation of the response was done using Goodman and Baron’s quantitative global acne scarring grading system (GBASG), physician visual analog scale (VAS), and patient VAS at baseline and 4, 8, 12, and 16 weeks. Relevant statistical tests were employed to study the effectiveness of both TCA and GA peels.
Results:
Significant reduction was noted in mean GBASG scores on both sides at 8, 12, and 16 compared to baseline score (P = 0.000). Mean GBASG scores decreased from 12.67 ± 3.19 to 8.97 ± 2.73 on the 70% GA side while that on the 30% TCA side reduced from 13.20 ± 3.56 to 6.83 ± 2.60 (P = 0.003). The results were much better on the TCA peel side as compared to GA peel as per physician VAS (P = 0.000) and patient VAS (P = 0.000). Side effects such as post-inflammatory hyperpigmentation and acne were seen on both sides while dryness and crusting were more common on the TCA peel side.
Conclusion:
A 30% TCA peel is efficacious and well-tolerated for mild-to-moderate acne scars. About 70% GA peel is an effective alternative to TCA peel, especially for patients not tolerating TCA or requiring lesser downtime.
Keywords
Glycolic acid
Trichloroacetic acid
Chemical peel
Acne scars
INTRODUCTION
Acne is a self-limiting condition that often results in scarring and disfigurement. Acne scarring has been recorded in 14% of women and 11% of men.1 All grades of acne from papulopustular to nodulocystic can cause scarring and, therefore, warrant early treatment.2 Scarring may occur early in acne and is related to both its severity and delay before treatment.2 Acne scars can often be psychologically distressing and decrease a person’s self-esteem and confidence.3
Acne scars have been classified into atrophic and hypertrophic, based on the morphology. Atrophic post-acne scars have been classified by Jacob et al. into three basic types: Icepick scars, rolling scars, and boxcar scars.4 Various treatment modalities have been used in the treatment of post-acne scarring, with varying success rates. These include surgical techniques such as subcision, punch excision, chemical peeling, microdermabrasion, autologous fat transplant, dermal fillers, and laser resurfacing. However, there has been no standard treatment option for the treatment of acne scars. Chemical peels are widely used in the management of acne and acne scars, but the risk of hyperpigmentation can be a potential limiting factor in Asian skin.5
Medium-depth chemical peels cause controlled keratocoagulation through the epidermis and into the papillary dermis. These cause deeper regenerative changes that can target pathology both within the epidermis and the superficial dermis. Most of the available literature on chemical peels focuses on their role in skin rejuvenation and hyperpigmentation. Medium-depth peels have shown excellent clinical efficacy in the treatment of superficial acne scars. Both glycolic acid (GA) at 70% and trichloroacetic acid (TCA) at 30% act as medium-depth peels and have been used in the treatment of mild-to-moderate acne scars. However, there is a paucity of well-conducted studies comparing various peels in the treatment of acne scars in Asian patients. We conducted this study to compare the efficacy and safety of 70% GA and 30% TCA peels in the treatment of facial atrophic acne scars.
MATERIAL AND METHODS
An open-label, prospective, interventional, left-right comparative, and split-face study was conducted at a tertiary care center in Delhi from December 2022 to June 2023 after obtaining permission from the Institutional Ethical Committee. The trial was registered with Clinical Trials Registry-India. Thirty patients aged more than 18 years with facial atrophic acne scars (Fitzpatrick skin types, IV-VI) were included in the study after obtaining informed written consent.
Patients who had active acne or had taken any topical treatment for acne scars in the past 1 month and oral treatment (including Isotretinoin) or any esthetic procedure (laser, platelet-rich plasma (PRP), and acne scar surgery) in the past 3 months were excluded from the study. Patients with active/recurrent herpes infection or a history of hypertrophic scarring/keloid were excluded from the study. Patients with hypersensitivity to aspirin, bleeding diathesis, human immunodeficiency virus/hepatitis B virus infection, and pregnant and lactating women were also excluded from the study.
Procedure
Clinical examination of post-acne scars was performed by a dermatologist with a magnifying lens, under good illumination, while the patient was sitting in an upright position. Grading of post-acne scars’ severity was performed using the qualitative and quantitative scarring grading system by Goodman and Baron [Table 1].6,7
| Grade | Type | No of lesions | ||
|---|---|---|---|---|
| 1–10 | 11–20 | >20 | ||
| A | Milder scarring – Macular erythematous, pigmented, mildly atrophic dish-like | 1 pts | 2 pts | 3 pts |
| B | Moderate scarring – moderately atrophic dish-like, punched-out small scars with, shallow bases but atrophic areas (<5 mm) | 2 pts | 4 pts | 6 pts |
| C | Severe scarring – punched out with deep but normal bases, punched out with deep but abnormal bases, linear or troughed dermal scarring, and deep and broad atrophic areas | 3 pts | 6 pts | 9 pts |
| D | Hyperplastic papular scars | 2 pts | 4 pts | 6 pts |
| E | Hyperplastic keloid or hypertrophic scars | Area <5 cm2–6 pts | Area 5–20 cm2–12 pts | Area >20 cm2–18 pts |
Pre-peel priming was advised in all patients using 0.025% tretinoin cream application at night and sunscreen sun protection factor (SPF 30) at daytime 2 weeks before the first peeling session. Patients were made to lie down in a reclining position. After cleaning and degreasing with acetone, 70% GA solution was applied on the right side of the face. Neutralization of GA solution was done after the first appearance of erythema. On the left side of the face, 30% TCA solution was applied till uniform frosting was seen, and then, the patient was instructed to wash the face. All patients were asked to avoid direct sun exposure, heat, and friction in the treated areas. They were instructed to apply sunscreen of SPF 30 regularly. The peeling was done at an interval of 4 weeks and a total of four sessions of chemical peeling were done.
Patient assessment
Serial digital photographs of each patient were taken at baseline, at each treatment session, and 1 month after the last treatment. Assessment of the efficacy of chemical peels was done using Goodman and Baron’s quantitative global acne scarring grading system (GBASG) [Table 1], physician visual analog scale, and patient satisfaction score (Patient Visual Analog Scale [VAS]). Goodman and Baron’s quantitative global acne scarring grading was done at baseline, at the 1st, 2nd, and 3rd monthly follow-up, and 1 month after treatment cessation (4th month) separately for both sides of the face. Physician’s VAS was done by a blinded dermatologist using digital photographs, wherein 0–25% was considered as mild improvement, 25–50% as moderate improvement, 50–75% as marked improvement, and 75–100% as excellent improvement. Patient VAS was done by the patient 1 month after the final session (4th follow-up) as per a similar quartile scale as Physician VAS. The primary outcome measure was as follows: 1. Comparison of mean acne scar grade on both sides of the face at the last (4th) follow-up. Secondary outcome measures were as follows:
Comparison of mean acne scar grade on both sides of the face at 1st, 2nd, and 3rd follow-up.
Comparison of VAS (Physician) at all (1st, 2nd, 3rd, and 4th) the follow-ups.
Comparison of VAS (Patient) at the last (4th) follow-up.
Statistical analysis
A Student’s t-test and paired t-test were conducted to determine whether there were statistically significant differences in mean scores for inter-group and intra-group comparisons, respectively. Proportions were compared using Chi-square or Fisher’s exact test, depending on their applicability. Analysis was conducted using the Statistical Package for the Social Sciences version 22.0. P < 0.05 was considered significant.
RESULTS
A total of 30 patients were enrolled in the study. There were 16 males and 14 females. Out of 30 patients, 13 (43.3%) patients were married. The mean age of the study patients was 26.2 ± 6.1 years (range: 18–38 years). The mean age of onset of acne was 12.7 ± 1.9 years. The mean duration of acne scar was 9.6 ± 4.7 years. Type 4 was the most common skin type (17 patients; 56.7%), followed by type 5 (8 patients; 26.7%) and type 3 (5 patients; 16.7%). Qualitative acne grading as per the Goodman and Baron Scale at baseline was similar in both groups. The mean GBASG score at baseline was 12.7 ± 3.2 and 13.2 ± 3.6 on the GA peel side and TCA peel side, respectively (P = 0.544). The scores on GA peel side decreased to 12.1 ± 3.4, 11.0 ± 3.7, 9.5 ± 3.2, and 8.9 ± 2.7 at 1st, 2nd, 3rd, and 4th follow-up, respectively. On the TCA peel side, the scores fell to 11.5 ± 3.8, 9.3 ± 2.9, 7.5 ± 2.7, and 6.8 ± 2.6 at 1st, 2nd, 3rd, and 4th follow-up, respectively [Table 2, Figures 1 and 2]. There was a significant fall in mean GBASG scores at 4th follow-up on both the TCA and GA sides as compared to the baseline score (P = 0.000). On comparing, the GA peel side with the TCA peel side, TCA fared much better at 3rd (9.5 ± 3.2 vs.7.5 ± 2.7; P = 0.010), and 4th followup (8.9 ± 2.7 vs. 6.8 ± 2.6; P = 0.003) [Table 2 and Figure 3].
| Mean acne scar scores | 70% glycolic acid (Mean±SD) (n=30) | 30% trichloroacetic acid (Mean±SD) (n=30) | P-value |
|---|---|---|---|
| Baseline | 12.67±3.198 | 13.20±3.566 | 0.544 (NS) |
| 1st follow-up | 12.10±3.387 | 11.50±3.821 | 0.522 (NS) |
| 2nd follow-up | 11.00±3.695 | 9.27±2.947 | 0.049 (S) |
| 3rd follow-up | 9.50±3.235 | 7.47±2.688 | 0.010 (S) |
| 4th follow-up | 8.97±2.735 | 6.83±2.601 | 0.003 (S) |
| Intra-group | 0.00 (S) | 0.00 (S) | |
| P-value |
SD: Standard deviation, NS: Not significant, S: Significant

- Patient 1: (a) Pre-peel and (b) post-peel photograph of glycolic acid peel side. (c) Pre-peel and (d) post-peel photograph of trichloroacetic acid peel side on the same patient at the last follow-up.
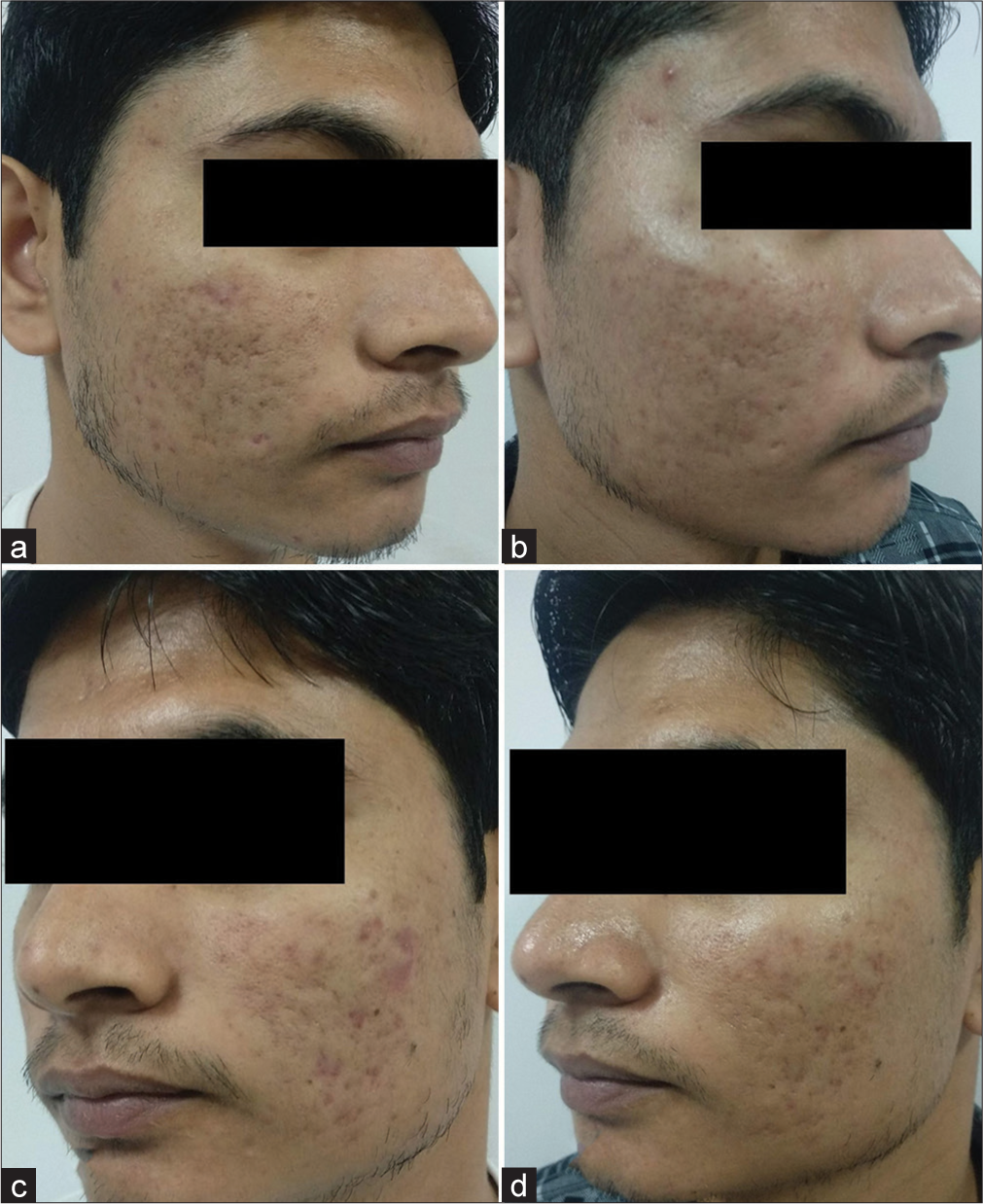
- Patient 2: (a) Pre-peel and (b) post-peel photograph of the glycolic acid peel side. (c) Pre-peel and (d) post-peel photograph of trichloroacetic acid peel side on the same patient at the last follow-up.
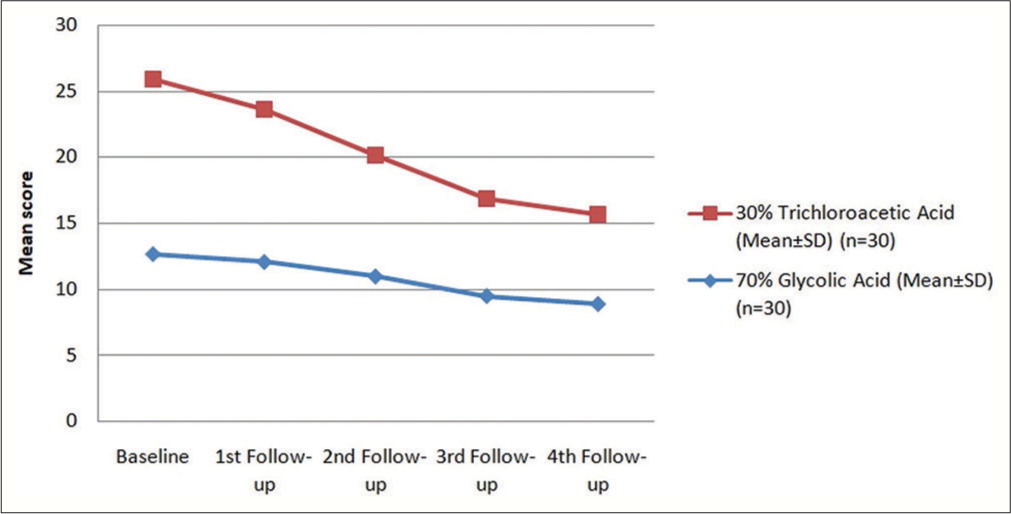
- Reduction in mean Goodman and Baron qualitative global scarring grading system (GBASG score) in the two groups, SD: Standard deviation.
The physician VAS grading was significantly better on the TCA peel side as compared to the GA peel side at each of the follow-ups [Table 3 and Figure 4]. At the last (4th) follow-up, 1 patient (3.3%) treated with 30% TCA showed excellent improvement, 15 patients (50%) had marked, and 14 patients (46.7%) had moderate improvement. Whereas, among patients treated with 70% GA, no patients had excellent improvement, only 2 patients (6.7%) had marked improvement, 21 (70%) had moderate improvement, and 7 (23.3%) had mild improvement according to physician VAS.
| Improvement as per physician VAS | Mild improvement (%) | Moderate improvement (%) | Marked improvement (%) | Excellent improvement (%) |
|---|---|---|---|---|
| 1st Follow–up | ||||
| 70% GA (n=30) | 28 (93.3) | 2 (6.7) | 0 (0) | 0 (0) |
| 30% TCA (n=30) | 21 (70.0) | 9 (30.0) | 0 (0) | 0 (0) |
| 2nd Follow-up | ||||
| 70% GA (n=30) | 19 (63.3) | 11 (36.7) | 0 (0) | 0 (0) |
| 30% TCA (n=30) | 6 (20.0) | 21 (70.0) | 3 (10.0) | 0 (0) |
| 3rd Follow-up | ||||
| 70% GA (n=30) | 14 (46.7) | 15 (50.0) | 1 (3.3) | 0 (0) |
| 30% TCA (n=30) | 0 (0) | 18 (60.0) | 12 (40.0) | 0 (0) |
| 4th Follow-up | ||||
| 70% GA (n=30) | 7 (23.3) | 21 (70.0) | 2 (6.7) | 0 (0) |
| 30% TCA (n=30) | 0 (0) | 14 (46.7) | 15 (50.0) | 1 (3.3) |
VAS: Visual analog scale, GA: Glycolic acid, TCA: Trichloroacetic acid
| Side effects | 70% glycolic acid (n=30) (%) | 30% trichloroacetic acid (n=30) (%) | P-value |
|---|---|---|---|
| Post-inflammatory hyperpigmentation | 2 (6.7) | 6 (20.0) | 0.129 (NS) |
| Acne | 6 (20.0) | 9 (30.0) | 0.371 (NS) |
| Dryness | 5 (16.7) | 12 (40.0) | 0.045 (S) |
| Crusting | 3 (10.0) | 20 (66.7) | 0.000 (S) |
NS: Not significant, S: Significant
The patient VAS scores were also significantly better on the TCA peel side as compared to the GA peel side at the last follow-up. (P = 0.000). Most patients reported mild-to-moderate improvement in acne scar with 70% GA peel while patients who underwent TCA peels reported moderate to marked improvement. Excellent improvement was noted in two patients with TCA peels as compared to none with GA peels [Figure 4].
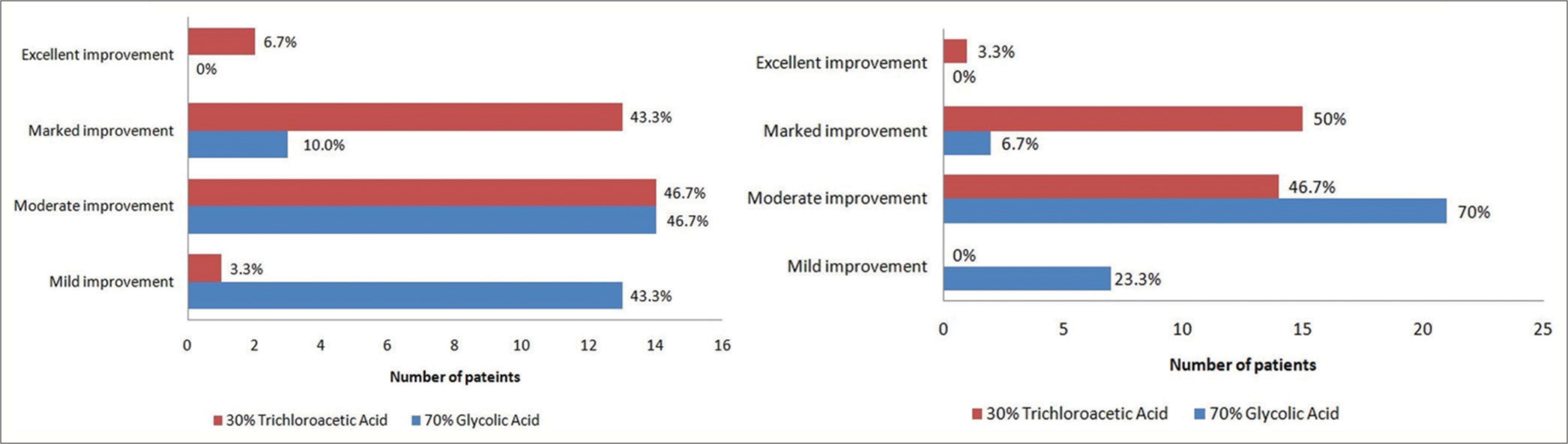
- Physician visual analog scale (VAS) and patient VAS at last (4th) follow-up.
Side effects from peels were noted in both treatment groups. All the side effects including post-inflammatory hyperpigmentation, acne, dryness, and crusting were noted more commonly on the TCA peel side; however, only dryness (P = 0.045) and crusting (P = 0.000) were found to be significantly higher [Table 4].
DISCUSSION
Chemical peels are an important part of today’s dermatology practice and are considered an adjunct therapy in treating all forms of acne and its sequelae. Medium-depth chemical peels including TCA and GA have previously been used for the treatment of acne scars, either alone or in combination with other therapies.8,9 TCA (30–50%) acts as a medium-depth peel and penetrates up to the papillary dermis.10 TCA causes denaturation of epidermal and dermal proteins, coagulative necrosis of epidermal cells, and destruction of dermal collagen.11,12 The clinical efficacy is seen due to reorganization in the dermal structure and increased collagen, glycosaminoglycans, and elastin in the dermis. GA peels are used at concentrations ranging from 20% to 70%.13,14 At a concentration of 70%, it acts as a medium-depth peel. GA acts as an exfoliative agent, causing desquamation of the skin by reducing corneocyte adhesion and keratinocyte plugging at the level of stratum granulosum.14,15 In addition, it also causes thickened epidermis and dermis with increased collagen and mucopolysaccharide synthesis, along with causing dispersion of melanin.15 Although no studies were comparing TCA with GA peel in acne scars, studies are available wherein these agents have been evaluated individually or in combination with other agents and compared with other peeling agents and found to be efficacious in acne scars.
Al-Waiz and Al-Sharqi have reported mild-to-moderate improvement in acne scars using a combination of Jessner’s solution followed by the application of 35% TCA.5 An open-label study evaluating the combination peel (20% TCA along with Jessner’s solution), a medium-depth peel for treatment of acne scars reported improvement in all except one patient who had mainly pitted scars and deep atrophic scars.16 They also noted that those with lighter skin complexion had lesser chances of developing hyperpigmentation. The authors also concluded that adding 20% TCA peel to Jessner’s solution would yield better results than the TCA alone.16 Puri compared the efficacy of a combination peel (20% TCA and Jessner’s solution) versus 20% TCA alone for the treatment of acne scars and found better outcomes in the combination group with lesser side effects.17
A study by Sharad evaluated the use of 35% GA peel as an adjuvant to microneedling in acne scars in Indian patients. They reported a significantly better improvement in the addition of GA peel indicating that GA peeling had an additive effect by promoting neocollagenesis.18 Another randomized controlled trial comparing 35% glycolic peel with microneedling versus microneedling alone revealed superior results in the combination group.19 Rana et al., in a study of 60 patients, also concluded that the addition of a still higher concentration of 70% GA peel to microneedling gives better scar improvement as compared to microneedling alone.20 In an open-label and non-randomized comparative study that evaluated 35% GA against 20% salicylic acid-10% mandelic combination peel, both peels produced equally significant improvement in the number of boxcar scars but had no significant effect on rolling scars and minimal effect on icepick scars.21 In a single-blind, placebo-controlled, and randomized comparative clinical study that evaluated the serial concentration of GA peels (20%, 35%, 50%, and 70%) versus 15% GA cream once or twice daily for 24 weeks, authors concluded that GA peeling is an effective modality for the treatment of atrophic acne scars.22
The lowest possible strengths at which they start acting as medium-depth peels, that is, GA peel at 70% and TCA at 30% concentration was chosen for this study. In our study, we found that both TCA and GA peels were efficacious in reducing acne scars and there was a significant fall in mean scores on both sides at each of the follow-ups as compared to the baseline score (P = 0.000). However, when comparing the two, TCA outscored GA peel in response. The mean scores on the TCA side continuously kept on improving faster as against the GA side at each follow-up, becoming significant at 2nd follow-up. As per Physician VAS and Patient VAS also, TCA peel gave better results as compared to GA peel.
Both the peels were well tolerated by the patients and the side effects were temporary and manageable by topical therapies. In our study, side effects such as post-inflammatory hyperpigmentation, acne, dryness, and crusting were noted more commonly on the TCA peel side. These were in concordance with previous studies on TCA peel where all these side effects are commonly observed.
CONCLUSION
About 30% of TCA peels are efficacious and well-tolerated for mild-to-moderate acne scars. About 70% GA peel is an effective alternative to TCA peel, especially for patients not tolerating TCA or requiring lesser downtime.
Authors’ Contributions
The contribution of the authors is as follows: Dr Mukesh Manjhi and Dr Pravesh Yadav-study conception and design, Dr Mukesh Manjhi, Dr Pravesh Yadav, Dr Vivek Sagar and Dr Aditi Gupta-data collection, analysis and interpretation of results, and Dr Garima Dabas and Dr Punit Pratap-manuscript preparation.
Ethical approval
The research was approved by the Institutional Ethical Committee F. No. 5(32)/2020/BSAH/DNB/PF/22610-11, dated 31.08.2022. The trial was registered with Clinical Trials Registry-India.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Management of post-acne scarring: What are the options for treatment? Am J Clin Dermatol. 2000;1:3-17.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical evaluation of acne scarring and its incidence. Clin Exp Dermatol. 1994;19:303-8.
- [CrossRef] [PubMed] [Google Scholar]
- Suicide in dermatological patients. Br J Dermatol. 1997;137:246-50.
- [CrossRef] [PubMed] [Google Scholar]
- Acne scarring: A classification system and review of treatment options. J Am Acad Dermatol. 2001;45:109-17.
- [CrossRef] [PubMed] [Google Scholar]
- Medium-depth chemical peels in the treatment of acne scars in dark-skinned individuals. Dermatol Surg. 2002;28:383-7.
- [CrossRef] [PubMed] [Google Scholar]
- Postacne scarring: A qualitative global scarring grading system. Dermatol Surg. 2006;32:1458-66.
- [CrossRef] [PubMed] [Google Scholar]
- Postacne scarring--a quantitative global scarring grading system. J Cosmet Dermatol. 2006;5:48-52.
- [CrossRef] [PubMed] [Google Scholar]
- Rejuvenation of the skin surface: Chemical peel and dermabrasion. Facial Plast Surg. 1996;12:125-33.
- [CrossRef] [PubMed] [Google Scholar]
- A practical approach to chemical peels: A review of fundamentals and step-by-step algorithmic protocol for treatment. J Clin Aesthet Dermatol. 2018;11:21-8.
- [Google Scholar]
- Variations and comparisons in medium-depth chemical peeling. J Dermatol Surg Oncol. 1989;15:953-63.
- [CrossRef] [PubMed] [Google Scholar]
- Focal treatment of acne scars with trichloroacetic acid: Chemical reconstruction of skin scars method. Dermatol Surg. 2002;28:1017-21.
- [CrossRef] [PubMed] [Google Scholar]
- Glycolic acid peel therapy-a current review. Clin Cosmet Investig Dermatol. 2013;6:281-8.
- [CrossRef] [PubMed] [Google Scholar]
- Chemical peeling in ethnic skin: An update. Br J Dermatol. 2013;169:82-90.
- [CrossRef] [PubMed] [Google Scholar]
- Superficial and medium-depth chemical peels. Clin Dermatol. 2008;26:209-18.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of modified Jessner's peel and 20% TCA versus 20% TCA peel alone for the treatment of acne scars. J Cutan Aesthet Surg. 2015;8:42-5.
- [CrossRef] [PubMed] [Google Scholar]
- Combination of micro needling and glycolic acid peels for the treatment of acne scars in dark skin. J Cosmet Dermatol. 2011;10:317-23.
- [CrossRef] [PubMed] [Google Scholar]
- Microneedling by dermapen and glycolic acid peel for the treatment of acne scars: Comparative study. J Cosmet Dermatol. 2019;18:107-14.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of microneedling with 70% glycolic acid peel vs microneedling alone in treatment of atrophic acne scars-A randomized controlled trial. J Cosmet Dermatol. 2017;16:454-9.
- [CrossRef] [PubMed] [Google Scholar]
- Glycolic acid peels versus salicylicmandelic acid peels in active acne vulgaris and postacne scarring and hyper pigmentation: A comparative study. Dermatol Surg. 2009;35:59-65.
- [CrossRef] [PubMed] [Google Scholar]
- Biweekly serial glycolic acid peels vs. Long-term daily use of topical low-strength glycolic acid in the treatment of atrophic acne scars. Int J Dermatol. 2000;39:789-94.
- [CrossRef] [PubMed] [Google Scholar]







