Translate this page into:
A Comparative Study of Effectiveness of Cryotherapy with Intralesional Triamcinolone Vs Fractional CO2 Laser with Topical Betamethasone for the Treatment of Keloids
Address for correspondence: Dr. Rajashekar T. S., Department of Dermatology, Sri Devaraj Urs Medical College, Tamaka, Kolar, Karnataka, India. E-mail: nishinagaria@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Introduction:
Keloids are hyperproliferative response of dermal connective tissue to trauma. Their management remains a challenge for practitioners as there is still no universally accepted treatment, leading to recurrences which are frustrating for patients and clinicians alike. Hence, it becomes essential to determine a modality with highest efficacy, least recurrence and produces good aesthetic results.
Objectives:
To compare the therapeutic effectiveness of combination of cryotherapy with intralesional corticosteroid and a combination of fractional CO2 laser followed by topical corticosteroids for treatment of keloids.
Materials and Methods:
This was a single centre, cross-sectional study consisting of 170 patients. Patients were randomly allocated in two groups, group one received a combination of cryotherapy with intralesional corticosteroid and group two was treated by laser ablation of keloid followed by topical corticosteroid application for four treatment sessions each after which they were evaluated for improvement.
Results:
There was remarkable difference in the treatment outcome of both the group, with group two showing more improvement (p value <0.001) and markedly fewer side effects. Patients in group two had less pain as compared to patients in group one, making them more compliant to treatment. Majority (31.8%) of patients belonged to 31–40 years of age group. The most common reason for treatment was for cosmetic concerns, seen in 70.6% of the patients.
Conclusion:
Both regimens showed excellent responses with minimum recurrence rates, indicating their high efficacy in management of keloids. However, regimen II was found to be aesthetically superior for the treatment of these exuberant scars.
Keywords
Combination therapy
cryotherapy
keloid
laser-assisted drug delivery
triamcinolone acetonide
INTRODUCTION
Keloids occur as a hyperproliferative response of dermal connective tissue to trauma. Wound healing is a complex biological process that involves various cell-to-cell and cell-to-matrix interactions in a complex environment of local and systemic stimuli. Over healed wounds, such as keloids, form when this healing process goes awry.
Keloids are irregular, hypertrophic lesions which most commonly occur in areas of high skin tension such as the chest region and extend beyond the original borders of the wound or inflammatory response. They may follow local skin trauma or inflammatory skin disorders like lacerations, tattoos, burns, injections, ear-piercing, vaccination, bites, acne, abscess or surgery. They are also known to occur spontaneously.
Besides posing as a cosmetic concern, causing social discomfort, psychological stress and embarrassment, these unsightly exuberant scars may also cause remarkable pain, pruritus, hyperesthesia and possibly affect joint movement. They seldom regress over time and have a major negative impact on one’s quality of life.
Keloids continue to be a problem for both patients and doctors. There is no universally approved treatment that results in permanent keloid scar ablation, despite the fact that different therapeutic procedures with treatment guidelines and recommendations have been published throughout the years.
Monotherapy have shown variable and transient results. Intralesional steroid (ILS), mainly triamcinolone acetonide, which is the first line of therapy has antimitotic effect inhibiting keratinocytes and fibroblast proliferation. It also stimulates fibroblast degeneration and reduce plasma protease inhibitors so that collagenase can degrade collagen. Cryotherapy achieves keloid destruction through direct cell anoxia due the formation of intracellular crystals, damage to the endothelial cell junctions and blood stasis, thereby producing microthrombi, vascular injury and ultimately tissue necrosis and sloughing. Fractional CO2 works by producing instant vaporization by heating target tissue to 1000C, is better used as an adjuvant.
Combination therapies like cryotherapy with ILS, however, have proved to produce better response rates with reduced incidence of recurrences.
This study was thereby undertaken to assess and compare the efficacy of two such combination therapies, namely the intralesional injection of triamcinolone with cryotherapy versus combination of Fractional CO2 with topical betamethasone, in achieving good cosmetic response.
This research looked at age, sex, location and family history in addition to the treatment features.
MATERIALS AND METHODS
This study was conducted in outpatient clinic of Dermatology, Venereology and Leprosy from December 2019 and May 2021 in patients with keloids. This was a hospital based randomized control interventional study consisting of 170 patients (85 in each group).
Method of data collection
Patients of either gender, above the age of 12 years, having single or multiple keloids of size not more than 10 cm in the largest diameter. Patients consenting for the study and willing for follow up were enrolled. Patients with infected keloids, co-existing inflammatory skin diseases, unrealistic expectations or with psychiatric illnesses, pre-existing bleeding disorders, renal diseases, hepatic disease, lactating/pregnant women, immunodeficient patients, diseases that react adversely to cold (Raynaud’s disease, cryoglobulinemia, cold urticaria) and with wound healing abnormalities were excluded.
The patients were randomly divided into two groups, which were administered two different treatment regimens. Before starting therapy, a full physical and systemic examination was performed, as well as any necessary fundamental investigations done. Serial photographs of the keloids were taken before the start of therapy and subsequent visits, during the course of treatment.
An informed consent was obtained from each patient after explaining the nature of the disease, course and prognosis. The institutional ethics committee granted permission to perform the study.
Group 1
At every session, following universal sterile precautions, the patient was given cryotherapy with liquid nitrogen until the appearance of a 1 mm halo of freeze, which will usually take around 10–20 seconds, at every session. Triamcinolone acetonide, 40 mg/1ml strength was given to the keloid after the second thaw. The volume differs among the patients due to the varying sizes of the keloids. We used 0.1ml per cm2, but did not exceed 1ml per lesion. The patient was given treatment once a month for 4 months, till lesions flattened or a maximum of 4 treatment sessions, whichever was sooner.
The drug was loaded in 1 cc syringe and injected under aseptic precautions with 26 Gauge needle. Multiple injections of 0.1 ml or >0.1ml were given regular intervals, and response was assessed by the Modified Manchester scar scale.
Group 2
Following universal sterile precautions, a topical anaesthetic cream (lignocaine 2.5% w/w + prilocaine 2.5% w/w) was applied on the lesion 1 hour before the procedure following which, one session of ablative fractional CO2 laser was given in each sitting. A topical corticosteroid (betamethasone cream) was applied over the keloid after laser treatment. Patient was also advised to use topical betamethasone cream twice a day, starting on the day of procedure till the end of the treatment. The patient was given treatment once a month for 4 months, till lesions flattened or a maximum of 4 treatment sessions, whichever was sooner.
Statistical analysis
Data was entered into Microsoft excel data sheet and was analyzed using SPSS 22 version software. Chi-square test or Fischer’s exact test was used as test of significance for qualitative data. Independent t test was used as test of significance to identify the mean difference between two quantitative variables.
P value <0.05 was considered as statistically significant after assuming all the rules of statistical tests.
GROUP 1:-ILS Triamcinolone with Cryotherapy
GROUP 2:-Fractional CO2 LASER with Topical Betamethasone
Evaluation
All the subjects underwent a maximum of 4 treatment sessions, or lesser if the lesions get flattened prior to 4 treatment sessions.
All treatment sessions were performed by a single skilled dermatologist. Keloid status throughout the treatment and follow-up period was assessed by serial photographs under similar lighting conditions. Blinded scoring of pre- and post-treatment photographs was done by Modified Manchester Scar Scale (MSS) with regards to changes in color, finish, contour, distortion, texture.
Pain scoring of the patient was also assessed during the treatment sessions.
RESULTS
Amongst the subjects in both the groups, majority (31.8%) were in the age range of 31–40 years followed 25.3% subjects in 21–30 years age-group. [Table 1]
| AGE | GROUP | TOTAL | |
|---|---|---|---|
| 1 | 2 | ||
| <20yrs | 13 | 12 | 25 |
| 15.3% | 14.1% | 14.7% | |
| 21-30yrs | 17 | 26 | 43 |
| 20.0% | 30.6% | 25.3% | |
| 31-40yrs | 25 | 29 | 54 |
| 29.4% | 34.1% | 31.8% | |
| 41-50yrs | 26 | 14 | 40 |
| 30.6% | 16.5% | 23.5% | |
| >50yrs | 4 | 4 | 8 |
| 4.7% | 4.7% | 4.7% | |
| Total | 85 | 85 | 170 |
| 100.0% | 100.0% | 100.0% | |
46.5% of the total subjects were female and 53.5% of the subjects were male. Majority (95.3%) of the patients had no family history of keloids. Of those with a positive family history, only 1 (12.5%) patient developed multiple keloids.
As for the site of keloids, they were most commonly found on the mid-sternum (36.45%), followed by shoulder (24.1%), earlobe (22.9%), upper extremity (15.3%) and lower extremity (6.2%). 11.1% patients had keloids on other parts of the body. [Table 2]
| Site | Group 1 | Group 2 | Total |
|---|---|---|---|
| MID STERNUM | 29(34.1%) | 33(38.8%) | 36.45% |
| EAR LOBE | 22(25.8%) | 17(20%) | 22.9% |
| ARM | 14(16.4%) | 12(14.1%) | 15.3% |
| SHOULDER | 20(23.5%) | 21(24.75% | 24.1% |
| LEGS | 6(7.05%) | 12(14.11%) | 10.6% |
| OTHERS | 11(12.9%) | 17(20%) | 11.1% |
Majority (70.6%) of the patients sought medical intervention for cosmetic reasons, followed by 25.9% of patients who came for treatment for symptomatic relief. Treatment for job purposes comprised of 3.5% of treatment seekers.
Assessment of the keloids prior-to and post-treatment based on the individual parameters in Modified Manchester Scar Scale
Colour
Prior to treatment, 54.7% of patients had obvious mismatch of color of keloid with the surrounding skin while 12.4% of patients had gross mismatch of color. Following treatment, majority (72.9%) of patients just had slight mismatch of color with the surrounding skin. However, 34.1% patients in group 1 continued to have obvious match of color. It was also noted that 16.5% of subjects in group 2 had perfect color match with the surrounding skin, providing better cosmetic relief to the patient.
Finish
Keloids in subjects of both the groups had shiny finish prior to treatment. After receiving the treatment, 47.1% of subjects in group 2 had improvement in the finish of the keloid. However, none of the patient in group 1 had the improvement.
Contour
In both the groups, the contour before treatment was keloid in all the subjects. After receiving treatment, majority (58.8%) subjects had slightly raised or indented contour. 35.9% of subjects had flushing with the surrounding skin, but it was seen more in patients in group 2 than group 1. A very small proportion (5.3%) of subjects, however had hypertrophic contour of the keloid after treatment.
Distortion
Distortion was moderate in 65.3% subjects, followed by 26.5% subjects who had mild distortion. A small proportion (8.2%) of subjects had severe distortion. Majority (72.4%) subjects had mild distortion after treatment. 19.4% of subjects had no distortion while 8.2% had moderate distortion.
Texture
63.5% of patients had firm keloids, followed by 19.4% who had hard. After treatment, majority (63.5%) of patients had just palpable keloids; followed by 18.8% patients who had firm keloid. 17.6% patients even achieved normal texture of the keloid post treatment.
Pain assessment
In our study, we found that patients in group 1 experienced more pain than patients in group 2. There was a statistically significant difference found between groups with respect to pain during the treatment.
Mean modified MSS score
Mean MSS score of patients in group 1 before treatment was 22.92 whereas for patients in group 2 was 22.60. Following treatment, Mean MSS score of patients in group 1 was 15.67 whereas for patients in group 2 was 12.56. [Table 3]
| Mss score | Group | Mean | Sd | P value |
|---|---|---|---|---|
| Before Treatment MSS score | 1 | 22.92 | 1.187 | 0.097 |
| 2 | 22.60 | 1.293 | ||
| After Treatment MSS Score | 1 | 15.67 | 1.546 | <0.001 |
| 2 | 12.56 | 1.459 |
This difference was statistically significant with respect MSS score after treatment.
Side effects
The most common side effect seen in patients after treatment was telangiectasia, seen exclusively in patients in Group 1, followed by skin atrophy, which was seen in 48.2% of the patients of Group 1.
Patients in both the groups had pigmentary changes, hypo or hyperpigmentation, with 25.8% from group 1 and 20% from group 2.
P value was 0.001, there was a statistically significant difference found between groups with respect to side effects post-treatment.
DISCUSSION
In this study, majority (31.8%) of the patients belonged to the age group of 31- 40 years, followed by 25.3% of patients in the age group of 21–30 years. The total range of age was from 12–60 years. More than 50% of the patients were within the age of 40 years.
A similar study has reported the onset of keloids are most commonly between 10 and 30 years of age and uncommon at age extremes.[12]
Out of 170 patients, 53.5% were males and 46.5% were females with a male to female ratio of 1.15:1. This concord with another study conducted, who also reported an almost equal incidence among both the sexes.[3]
In this study, keloids were most commonly found on the mid-sternum (36.45%), followed by shoulder (24.1%), earlobe (22.9%), upper extremity (15.3%) and lower extremity (6.2%). 11.1% patients had keloids on other parts of the body. In a similar study, a higher incidence of keloids over the presternal area followed by deltoid and ear.[4] In another study, it was observed that keloids occur most commonly over the chest, shoulder, upper back, nape of neck and ear lobes.[5]
In the present study, 4.7% of patients had a positive family history and reported a familial incidence ranging from 4% to 16% in black and Hispanic population.[1] In a different study, it was reported a familial incidence of 50%.[6]
Out of 170 patients, 70.6% of patients presented with cosmetic disfigurement and 25.9% complained of pruritus, which were of mild or moderate intensity. 3.5% of the patients came seeking for medical intervention for job purposes. In the study pruritus, pain, cosmetic disfigurement, skin discoloration and restriction of movements were the presenting complaints.[1] The main presenting symptoms in a similar study were itching (64.3%), pain (21.4%), cosmetic reasons (21.4%) and restriction of movement (7.1%).
RESPONSE OF PATIENTS TO RESPECTIVE REGIMENS
In this study, the primary outcome evaluated based on the Modified Manchester Scar Scale scoring and it was considered as the main parameter of efficacy.
Patients in both the regimens were comparable with respect to age, sex, site and number of lesions, with statistically no significant difference (P > 0.05).
Assessment of the keloids prior-to and post-treatment based on the individual parameters in modified manchester scar scale
Color
A study has suggested that dyschromia showed more improvement as a result of topical steroid plus laser therapy.[7] In another comparative study, it demonstrated good response of texture.[8]
In patients under treatment with laser plus triamcinolone, dyschromia did not show good response to this treatment probably because their study had no comparison group.
Finish
P value - <0.001, which was statistically significant between both groups with respect to finish of the keloid.
Contour
In both the groups, the contour before treatment was keloid in all the subjects.
Regimen II: Fractional CO2 LASER with Topical Betamethasone
Post treatment – Larger proportion (44.7% vs 27.1%) of subjects had achieved “flushed with surrounding skin” contour as compared to patients in Group 1. 52.9% patients continued to have a slightly raised of indented contour. A negligible proportion (2.4%) of patients had hypertrophic contour.
P value - 0.023, which was statistically significant between groups with respect to contour.
In a different study, it showed more than 50% improvement in the degree of hypertrophy of the 40% of the lesions treated in the study.[9]
Distortion
The results in our study are in concordance with similar studies, where the general appearance of the wound was better in the intralesional triamcinolone acetonide injection treated lesions.
Texture
P value - 0.040, which was statistically significant between both groups with respect to texture.
This result is likewise as a study conducted wherein the group receiving Fractional CO2 Laser with topical steroids had better improvement in texture.[10] In another study, it demonstrated good response of texture in patients under treatment with laser plus triamcinolone.[8]
Based on the overall improvement in modified manchester scar scale score
On the MSS, lower scores indicate a better scar character profile and thus the greater the magnitude of the decrease, the greater the improvement of the keloid.
Regimen 1- Studies have shown that contact spray cryotherapy with intralesional triamcinolone acetonide injection can bring about 68–81% remission with <2% recurrence. But around 20 sessions are required to achieve these results.[10]
Regimen 2 - Another recent study, concluded that local corticosteroids plus fractional laser therapy was more effective than intralesional corticosteroids injections for the improvement of dyschromia and texture of hypertrophic and keloid scars.[7]
In a contrasting study, it was reported that intralesional corticosteroid injection plus laser had no additional effects over treatment with PDL alone, which is not in congruence with our results.[11]
Pain
In our study, we found that patients in group 1 experienced considerably more pain than patients in group 2. There was a statistically significant difference found between groups with respect to pain experienced during the treatment.
In a separate study, pain and itching were reduced in 73.3% with triamcinolone betamethasone.[12] In this study, reduction in pain was statistically significant in both the groups.
The high pain associated with Regimen I might be a reason for high dropout rates seen in patients on cryotherapy with intralesional triamcinolone.
Treatment outcomes in both the regimens
Among the two regimens, both regimens had good response. However, the treatment outcome between the two regimens was statistically significant, (P < 0.05) with regimen II showing faster and more cosmetically acceptable results at the end of 4 treatment sessions. [Graph 1]
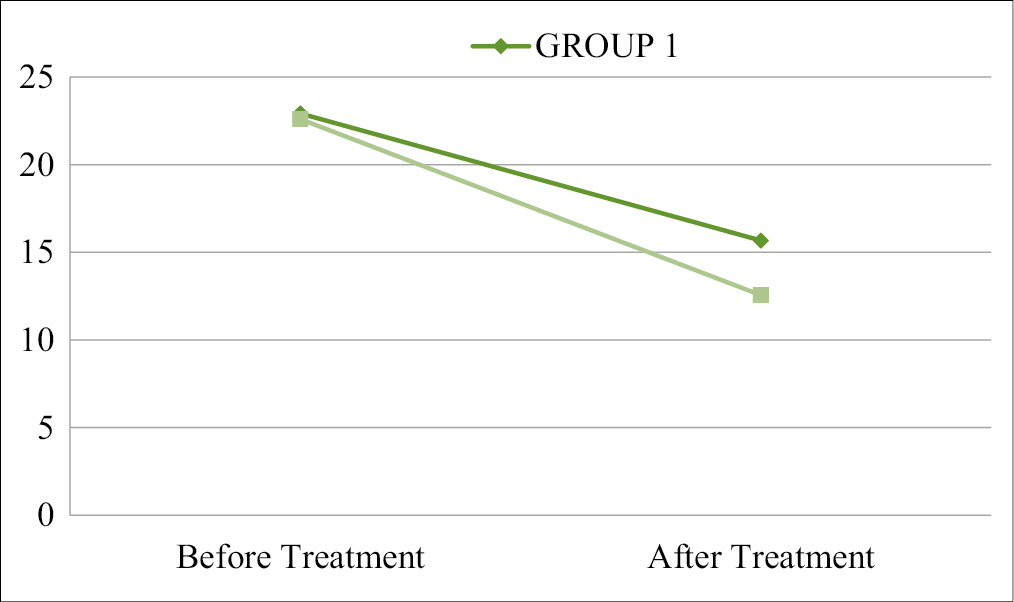
- Graph Showing Comparison of MSS Score Between Groups
Side effects
The most common adverse effects were seen 1–2 months after starting the treatment sessions.
Of the 170 patients included in the study, 60% of patients developed complications, of which majority (83.3%) of patients belonged to regimen I and rest (16.7%) of the patients belonged to regimen II. In the study it was reported hypopigmentation, local edema and epidermolysis as the observed side effects following intralesional cryotherapy.[13] These results are in concordance with another study, also reporting hypopigmentation / depigmentation along the needle tracks in all cases, which improved during the follow-up period.[14] The results in our study are also in concordance with results of another study,wherein there was reduced incidence of hypopigmentation and atrophy in the group receiving Fractional CO2 Laser treatment.[1516]
In a different study, Fractional CO2 + ILS group had more side effects compared to ILS only group, though the difference was not statistically significant.[9] In the present study, Group II had remarkably lesser side effects resulting in better acceptability and compliance with the treatment.
CONCLUSION
Combination therapies are highly effective in treatment of keloids, especially those resistant to standard monotherapies. Of the two regimens, although both combinations were equally efficacious, rate of improvement was better with regimen II. However, based on the side effect profile, wherein more troublesome and persistent complications were observed in regimen I, regimen II was considered to be far safer and with aesthetically superior outcomes.
Thus, Regimen II can be recommended for the successful treatment of keloids by the authors with a better side-effect profile.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Hypertrophic scars and keloids. A collective review. Plast Reconstr Surg. 1974;53:140-54.
- [Google Scholar]
- Description of site-specific morphology of keloid phenotypes in an afrocaribbean population. Br J Plast Surg. 2004;57:122-33.
- [Google Scholar]
- Keloid disease: Clinical relevance of single versus multiple site scars. Br J Plast Surg. 2005;58:28-37.
- [Google Scholar]
- Intralesional 5-fluorouracil as a treatment modality of keloids. Dermatol Surg. 2004;30:54-6; discussion 56-7.
- [Google Scholar]
- Comparative effect of ablative fractional CO2 laser plus triamcinolone acetonide cream versus intralesional injection of triamcinolone acetonide in keloid and hypertrophic scars: A randomized clinical trial. J Skin Stem Cell [Internet]. 2018;5:e69394.
- [Google Scholar]
- Treatment of hypertrophic scars using laser and laser assisted corticosteroid delivery. Lasers Surg Med. 2013;45:135-40.
- [Google Scholar]
- Efficacy of fractional CO2 laser with intralesional steroid compared with intralesional steroid alone in the treatment of keloids and hypertrophic scars. J Cosmet Dermatol. 2019;00:1-9.
- [Google Scholar]
- Laser scar revision: Comparison study of 585-nm pulsed dye laser with and without intralesional corticosteroids. Dermatol Surg. 2003;29:25-9.
- [Google Scholar]
- Use of intralesional cryosurgery as an innovative therapy for keloid scars and a review of current treatments. J Clin Aesthet Dermatol. 2013;6:23-6.
- [Google Scholar]
- Intralesional cryotherapy for enhancing the involution of hypertrophic scars and keloids. Plast Reconstr Surg. 2003;111:1841-52.
- [Google Scholar]
- Therapeutic efficacy of intralesional steroid with carbon dioxide laser versus with cryotherapy in treatment of keloids: A randomized controlled trial. Dermatol Surg. 2016;42:1188-98.
- [Google Scholar]
- Surgical excision and immediate postoperative radiotherapy versus cryotherapy and intralesional steroids in the management of keloids: A prospective clinical trial. Med Princ Pract. 2010;19:402-5.
- [Google Scholar]






