Translate this page into:
A Comparative Study of Efficacy of 5% Minoxidil and 5% Minoxidil Plus Platelet-Rich Plasma in Same Patient for Treatment of Androgenetic Alopecia
Address for correspondence: Dr. Dilip Kachhawa, Bunglow No. 3 O/s MDM Hospital, Jodhpur, Rajasthan 342003, India. E-mail: drdilipkachhawa@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Androgenetic alopecia (AGA) is characterized by androgen-related progressive thinning of the scalp hair in a defined pattern. It has an effect on social and psychological well-being of the patient. It is often recalcitrant to medical treatment alone.
Aim:
The aim of the study was to compare the efficacy of 5% minoxidil and 5% minoxidil plus platelet-rich plasma (PRP) in same patient for the treatment of AGA.
Materials and Methods:
A prospective randomized study was conducted on 50 patients of AGA attending the outdoor department. Scalp of each patient was divided into right side and left side, to compare the effectiveness of 5% minoxidil on the right side with combination of 5% minoxidil and intradermal PRP on the left side at an interval of 1 month for a period of 6 months. Clinical improvement was assessed monthly till 6 months by the serial hair pull test, global photography, patient satisfaction score, trichoscopic evaluation, and hair density.
Results:
For post-procedure subjective perception at the end of 6 months, the minoxidil 5% side showed good response in 41% (n = 18), moderate in 20% (n = 9), and poor in 39% (n = 17), whereas the PRP + minoxidil 5% side showed good response in 59% (n = 26), moderate in 16% (n = 7), and poor in 25% (n = 11) of the patients.
Conclusion:
The combination consists of 5% minoxidil and intradermal PRP, which appears to be simple, safe, and effective treatment in AGA. It can be used in poor responders in conventional medical therapy.
Keywords
Androgenetic alopecia
global photography
platelet-rich plasma
INTRODUCTION
Androgenetic alopecia (AGA) is characterized by androgen-related progressive thinning of the scalp hair in a defined pattern. It affects social and psychological well-being of the patients. It usually begins around 20 years of age and affects 50% of the men by the age of 50 years.[12] Its etiopathogenesis is androgen-dependent and orchestrated via the testosterone metabolite dihydrotestosterone, the expression of androgen receptor, and genetic factors.[3]
AGA is characterized by the progressive miniaturization of hair follicles, with the transformation of terminal hair into vellus hair. AGA is believed to be attributed to genetic and environmental factors and is known to cause upregulated perifollicular 5-α reductase expression.
The 5-α reductase converts testosterone to dihydrotestosterone that binds to androgen receptors and leads to the activation of genes that transform healthy terminal follicles into vellus-like hairs in androgen-dependent areas of the scalp. These areas are the central, frontal, and parietal regions.[45]
A lot of medical and surgical treatment modalities is available for AGA including minoxidil, finasteride, spironolactone, nutritional supplementation, low-level light therapy, and hair transplantation surgery. These modalities may not be always effective, require long-term compliance and may be associated with unacceptable side effects.
Topical minoxidil was found to cause hypertrichosis by increasing microcirculation by vasodilation and stimulates the mitosis in epithelial cells. It is available in strength ranging from 2% to 12.5%, although only 2% and 5% have been approved by the Food and Drug Administration (FDA).
Another upcoming trend is platelet-rich plasma (PRP), an autologous preparation of platelets in concentrated plasma and an exciting non-surgical therapeutic option for hair growth and stimulation.
PRP contains an abundance of growth factors and cytokines, many of which are implicated in hair growth.[6] These growth factors include platelet-derived growth factor, transforming growth factor, vascular endothelial growth factor, and epithelial growth factor. Besides, PRP contains fibrin, fibronectin, and vitronectin, which are known to act as cell adhesion molecules. Thus, PRP plays a key role in cell migration, attachment, proliferation and differentiation, and extracellular matrix accumulation. The regenerative potential of PRP depends on the levels of growth factors released upon activation and thus has emerged as an effective alternative in the management of AGA.[78]
Combination therapy with topical minoxidil plus PRP provides a promising, effective, and safe modality for the treatment of AGA.
The aim of the study was to compare the efficacy of 5% minoxidil alone and 5% minoxidil plus PRP in the treatment of AGA and hence to observe the synergic effect when used with minoxidil 5%.
MATERIALS AND METHODS
Study design
This was a hospital-based interventional comparative study conducted in the outpatient Department of Dermatology over a period of 1 year from July 2018 to June 2019. Ethical approval for the study was obtained from the Institutional Ethics Committee.
Sample size
Sample size was calculated at 95% confidence interval assuming an expected 70% or more efficacy (as per findings of a previous study) for each procedure and taking 20% relative allowable error. Sample size was calculated using the formula for sample size for estimation of proportion:
where
 = standard normal deviate for 95% confidence interval (taken as 1.96),
= standard normal deviate for 95% confidence interval (taken as 1.96),
P = expected efficacy of each procedure (assumed as 70%),
E = relative allowable error (taken as 20% of P).
Sample size was calculated to be minimum of 43 subjects. Considering 10% attrition, sample size was enhanced and rounded off to 50 subjects.
Sampling technique
All consecutive eligible patients fulfilling inclusion criteria were enrolled till desired sample size is met.
Study subjects
A total of 50 patients with AGA attending the outpatient Department of Dermatology during the study period, who satisfied the following criteria, were enrolled in the study: patients of age group between 18 and 54 years with male-patterned hair loss Grade II–V (Norwood–Hamilton classification) and not taking any treatment for last 6 months. Patients with any serious systemic and metabolic disease, platelet disorders, hemodynamic instability, heavy nicotine, drug and alcohol consumption, and unrealistic expectation were excluded from the study.
Methodology
Detailed history and clinical examination include type of hair loss such as thinning, shedding, and breaking, presence of any inflammation, scaling, erythema, hair pull test, and relevant investigations including HIV, HBsAg, and platelet count. Grading was done according to the Hamilton–Norwood scale.
After obtaining informed consent, 8.5 mL of blood sample was aspirated using an 18G needle and collected in an acid citrate dextrose vacutainer tube. In an open system, the first centrifugation or soft spin was carried out at 1200 rpm for 8 min. The separated buffy coat with platelet-poor plasma (PPP) was collected with the help of a pipette in another test tube. This tube underwent a second centrifugation, a faster hard spin at 2400 rpm for 4 min. The upper layer containing PPP was discarded and the lower layer of PRP was taken for platelet count.
Before the administration of PRP, scalp of each patient is arbitrary, divided into right and left sides and cleaned with spirit and betadine. PRP was injected by an intradermal technique (multiple small injections in a linear pattern 1 cm apart) under proper aseptic precautions in the left side of the scalp at a monthly interval of 6 months. All patients were told to apply 1 mL of topical 5% minoxidil solution twice a day on both sides and were followed up similarly.
Clinical improvement was assessed monthly till 6 months by the serial hair pull test, global photography, patient satisfaction score, trichoscopic evaluation, and hair density.
Subjective improvements of patients were noted on a Dermatology Life Quality Index (DLQI) scale. The patients were further evaluated at the end of six sittings. Subjective satisfaction is assessed by patient’s self-assessment through the following set of questionnaires:
| Questionnaire | Score |
|---|---|
| Bald spot getting smaller | 1 |
| Improvement in appearance of hair | 1 |
| Increase in hair count | 1 |
| Decreased shedding of hair | 1 |
| Overall improvement in hair after therapy | 1 |
Response was graded by patients as follows:
Good response when score was ≥4
Moderate grade when score was 2–3
Poor response when score was <2
Statistical analysis
It was performed with PRIMER and SPSS, Trial version 20 for Windows Statistical Software Package (SPSS Inc., Chicago, IL, USA). Categorical data were presented as numbers (percent) and were compared among groups using the χ2 test. Groups were compared for demographic data and values were presented as mean and standard deviation. P-value less than 0.05 was considered statistically significant.
RESULTS
A total of 50 male patients were enrolled, and the most common age group was 31–40-year-age group, 46%(n = 23). In family history, out of 50 patients, 72% (n = 36) of the patients had positive family history of AGA and 28% (n = 14) had no family history.
The most common morphological type in our study was Grade II of Norwood–Hamilton [42% (n = 21)], followed by Grades III, IV, and V having 28% (n = 14), 18% (n = 9), and 12% (n = 6) of the patients, respectively [Table 1].
| Grade | Number of patients | Percent |
|---|---|---|
| II | 21 | 42.0 |
| III | 14 | 28.0 |
| IV | 9 | 18.0 |
| V | 6 | 12.0 |
| Total | 50 | 100.0 |
On the minoxidil side, pre- and post-mean ± SD of hair density was 93.97 ± 4.0 and 104.8 ± 4.97, respectively. In the minoxidil + PRP side, pre- and post-mean ± SD of hair density was 93.97 ± 4.0 and 113 ± 7.66, respectively [Table 2].
| Minoxidil side | PRP + minoxidil side | P-value | |
|---|---|---|---|
| Pre | 93.97 ± 4.0 | 93.97 ± 4.0 | — |
| Post | 104.8 ± 4.97 | 113 ± 7.66 | <0.001 (S) |
| P-value | <0.001 (S) | <0.001 (S) |
PRP = platelet-rich plasma
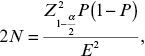
In our study, post-procedure subjective perception after the last visit was good in the minoxidil 5% side in 41% (n = 18), moderate in 20% (n = 9), and poor in 39% (n = 17), whereas in the PRP +minoxidil 5% side, 59% (n = 26) of the patients showed good response [Figures 1,–3], 16% (n = 7) showed moderate, and 25% (n = 11) showed poor response [Table 3].
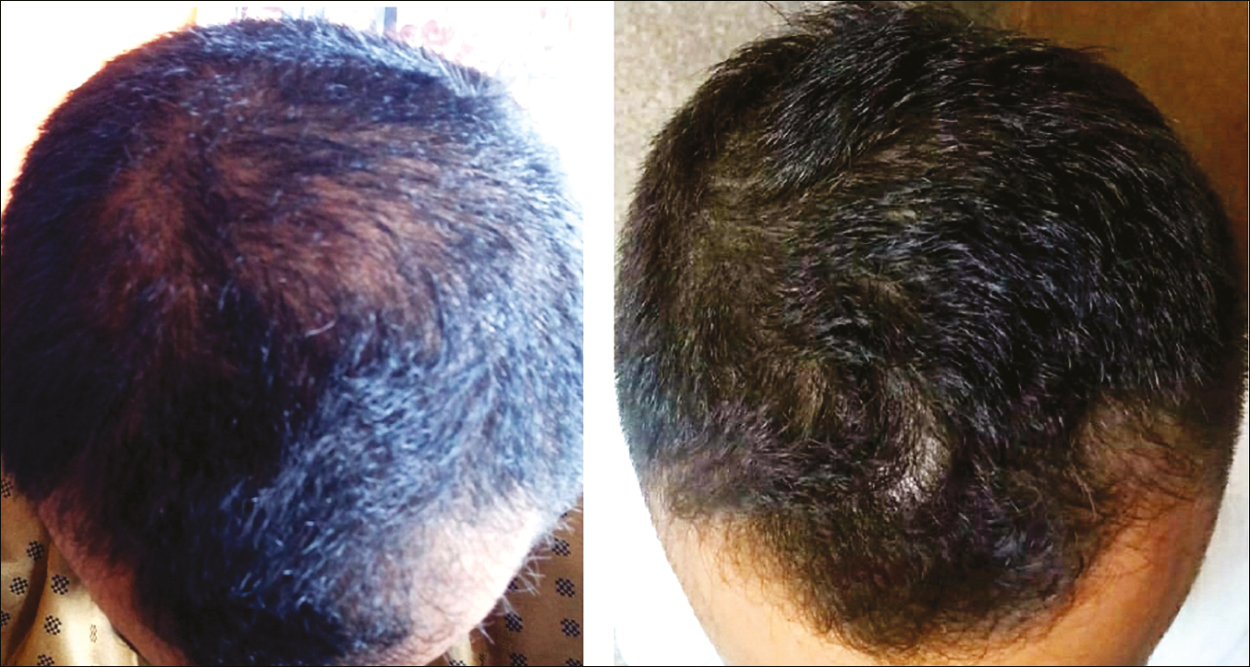
- Pre- (0 month) and post-procedural (6th month) global photographic assessment showing better results with platelet-rich plasma + minoxidil 5% therapy at the end of 6th month

- Pre- (0 month) and post-procedural (6th month) global photographic assessment showing good results with platelet-rich plasma + minoxidil 5% therapy at the end of 6th month
- Pre- (0 month) and post-procedural (6th month) global photographic assessment showing good results on both sides
| Response | Minoxidil 5% (n = 44) | PRP + minoxidil 5% (n = 44) |
|---|---|---|
| Good | 18 (40.9%) | 26 (59.09%) |
| Moderate | 9 (20.4%) | 7 (15.9%) |
| Poor | 17 (38.6%) | 11 (25%) |
In this study, 44 out of the 50 patients continued the study; 11.4% (n = 5) of the patients perceived side effects in the minoxidil side, whereas 9.1% (n = 4) perceived in the PRP + 5%minoxidil side.
Side effects were erythema, burning, fever, persistent pain, edema, and flaking. Erythema and flaking were the most common side effects observed. Less side effects in the PRP + minoxidil 5% group show the superiority of adding PRP to the regimen.
Comparing the mean change in DLQI from the first to the last visit, we observed a highly significant (P <0.001) decline in DLQI in both sides. In the minoxidil 5% side, the DLQI reduced from a mean value of 16.61 ± 2.2 before treatment to 4.75 ± 4.0 after treatment; in the PRP + minoxidil 5% side, it reduced from a value of 16.61 ± 2.2 to 3.0 ± 3.53, thus suggesting that minoxidil 5% + PRP had better DLQI response. However, both were statistically significant [Table 4].
| Minoxidil side | PRP + minoxidil side | P-value | |
|---|---|---|---|
| Pre | 16.61 ± 2.2 | 16.61 ± 2.2 | — |
| Post | 4.75 ± 4.0 | 3.0 ± 3.53 | <0.001 (S) |
| P-value | <0.001 (S) | <0.001 (S) |
PRP = platelet-rich plasma
DISCUSSION
AGA has a significant influence on psychological distress and is associated with low self-esteem and depression. It is thus important to provide them with the best possible modality of treatment and help them to cope up better. Treatment options for AGA are very limited and include topical minoxidil and oral finasteride (FDA-approved) either alone or in combination.[910]
Although many studies have been done in the past demonstrating the efficacy of minoxidil therapy and PRP therapy independently, there has not been much in the literature about the comparison of both forms of therapies. Our study compares minoxidil 5% therapy and PRP therapy (a newer therapy) with minoxidil 5% therapy, to assess the synergic effect of PRP with minoxidil 5% in the treatment of AGA.
In our study, clinical improvement was assessed by the hair pull test, global photography, patient satisfaction score, and trichoscopic evaluation of hair density for both minoxidil 5% and PRP + minoxidil 5% sides. The endpoints were improvement in hair density and thickness as noted by a hair densitometer (Dermoscope), patient’s self-assessment through a set of five validated questionnaires, and less time taken to achieve negative hair pull test and increased volume of hair in global photography.
In the present study, we observed significant improvement in hair volume in global pictures after four sessions of PRP. These findings were compared with the study conducted by Betsi et al.[5]
Trichoscopic examination of hair density
The mean hair density in the minoxidil 5% only side at the first visit was 93.97 ± 4.0 and the last visit was 104.77 ± 4.97, and that PRP + minoxidil 5% side at the first and last visits was 93.97 ± 4.0 and 113 ± 7.66, respectively. Both sides showed a statistically significant increase in their mean hair density, whereas the PRP + minoxidil 5% side showed better results in increasing density of hair at the last visit. The mean hair density after the last visit showed a significant difference in the PRP + minoxidil 5% side.
Gentile et al.[11] conducted a randomized, evaluator-blinded, placebo-controlled, and half-head group study of 20 male patients with male pattern hair loss stages II–IV of the Norwood–Hamilton classification. After three treatments at 30-day intervals, patients showed an improvement in mean hair count and total hair density (by computerized trichogram) compared with those who received placebo. This is in accordance with the results we observed in the present study.
Uebel et al.[12] in 2005 showed that area treated with PRP demonstrated a yield of 18.7 follicular units/cm2 vs. 16.4 follicular units/cm2 of the placebo group, an increase in follicular density of 15.1%. Greco and Brandt[6] in 2009 observed an increase in hair density of 18.8% at 3 months and 29% at 9 months in patients treated with the PRP group. Olsen et al.[13] studied 31 men using 2% or 3% minoxidil for AGA and showed that hair regrowth tended to peak at 1 year and that non-vellus hair, beyond that seen at baseline, was maintained at 4.5–5 years later. Another study with the topical use of 2% and 5% minoxidil demonstrated a statistically significant increase in hair volume when compared with placebo.[14] Knighton and Hudson[7] in 2007 used PRP for the treatment of non-healing wounds and found that topical application of PRP to areas of tissue containing hair follicles showed increased hair growth, where no growth or limited growth was previously observed.
Olsen et al.[13] in 2007 in a placebo-controlled trial of 5% foam of minoxidil showed a statistically significant increase in hair counts and subjective assessment over placebo during a 16-week period of twice daily usage. Rinaldi et al.[8] found that growth factors from PRP could prevent dermal papilla apoptosis, prolong anagen phase, delay catagen and telogen, eventually reducing diffuse hair loss and stimulating hair re-growth in AGA, without side effects during the treatment period, and after 12 months from the end of treatment.
Post-procedural subjective perception in study
We observed significant result in the protocol followed in our study. When compared with previous studies, few studies were equally efficacious but very few studies showed no change in hair fall. In our study, the PRP + minoxidil 5% side in comparison with minoxidil 5% side had better efficacy at the end of 6 months. This can be explained that minoxidil will paradoxically increase hair fall in the early stage of treatment and PRP by protecting the hair follicle reduces this side effect of the drug. A few people had increased hair fall at the end of visit, which is minimal, hence most patients had satisfying perception scores. Post-procedure subjective perception is assessed by patient’s self-assessment.
According to the questionnaire, response was graded as good, moderate, and poor. In the present study after the last visit, 59% (n = 26) of the patients had good response, 16% (n = 7) showed moderate, and 25% (n = 11) showed poor response in the minoxidil 5% + PRP side, which is comparatively better than the minoxidil 5% side that was good in 41% (n = 18), moderate in 20% (n = 9), and poor in 39% (n = 17). So our study postprocedural satisfaction score was better in the PRP + minoxidil 5% side than that in the minoxidil 5% side.
Limitations of our study included an unblinded design, small sample size, no placebo control, and a short follow-up period of only 6 months.
CONCLUSION
In conclusion, we found that topical 5% minoxidil and intradermal PRP has higher efficacy than topical 5% minoxidil alone in AGA. It is a useful therapy in poor responders to conventional therapy.
A combination of the above therapies can not only boost hair growth but can also arrest the progression of hair loss for a considerable amount of time. PRP is an exciting new non-surgical therapeutic option for hair growth and stimulation in patients of AGA. Platelet growth factors are probably capable of regulating the life cycle of hair bulbs, thus ensuring better growth of hair. As a result, growth of hair and even an increase in its density could be obtained.
Considering its excellent safety profile, PRP with minoxidil 5% is a promising treatment option for patients with AGA of mild-to-moderate grade.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Male pattern androgenetic alopecia in an Indian context: A perspective study. J Eur Acad Dermatol Venereol. 2007;21:473-9.
- [Google Scholar]
- Psychological effect, pathophysiology, and management of androgenetic alopecia in men. Mayo Clin Proc. 2005;80:1316-22.
- [Google Scholar]
- Medical treatments for male and female pattern hair loss. Am J Dermatol. 2008;59:547-66.
- [Google Scholar]
- Platelet-rich plasma injection is effective and safe for the treatment of alopecia. Eur J Plast Surg. 2013;36:407-12.
- [Google Scholar]
- The effects of autologous platelet rich plasma and various growth factors on non-transplanted miniaturized hair. Hair Transplant Forum Int. 2009;19:49-50.
- [Google Scholar]
- Regents of the University of Minnesota, Minneapolis, Minn, Curative Technologies. Method for Promoting Hair Growth. (September 18). US Patent 4957742
- [Google Scholar]
- The role of platelet rich plasma to microneedling anagen phase: Evaluation in vitro & in vivo in hair transplant and hair treatment. Int J Trichol. 2011;3 suppl.:14-5.
- [Google Scholar]
- Finasteride in the treatment of androgenic alopecia. J Am Acad Dermatol. 1998;39:578-89.
- [Google Scholar]
- The effect of platelet-rich plasma in hair regrowth: A randomized placebo-controlled trial. Stem Cells Transl Med. 2015;4:1317-23.
- [Google Scholar]
- The role of platelet plasma growth factors in male pattern baldness surgery. Plast Reconstr Surg. 2006;118:1458-66.
- [Google Scholar]
- A randomized clinical trial of 5% topical minoxidil versus 2% topical minoxidil and placebo in the treatment of androgenetic alopecia in men. J Am Acad Dermatol. 2002;47:377-85.
- [Google Scholar]






