Translate this page into:
A comparative study of fractional CO2 laser with topical triamcinolone acetonide versus intralesional triamcinolone acetonide in the treatment of alopecia areata
Address for correspondence: Dr. Rajashekar Talari Srinivas, Department of Dermatology Venereology and Leprosy, Sri Devaraj Urs Medical College, Tamaka, Kolar 563103, Karnataka, India. E-mail: yeshits@rediffmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Introduction:
Alopecia areata (AA) is a non-scarring alopecia of chronic autoimmune etiology with heterogenous severity against the anagen hair follicle over the scalp, beard, or any part of the body and is associated with a significant psychological morbidity in the mental status of the patients leading the patients to seek treatment for cosmetic reasons. The management of AA is very unpredictable and is associated with various cosmetic adverse effects. This study aimed at comparing the efficacy and safety of a novel procedure of laser-assisted drug delivery system of steroids with the first-line procedure of intralesional steroids (ILS) for the treatment of patchy AA.
Aims and Objectives:
To assess and compare the efficacy and safety of fractional CO2 laser in combination with topical triamcinolone acetonide aqueous solution and intralesional triamcinolone acetonide as a monotherapy and in the treatment of AA.
Materials and Methods:
A total of 60 patchy AA patients were included in this study. Patients were randomized into two equal groups: Group A and Group B with 30 patients in each group using a computer-generated block randomization. Patients in Group A received fractional CO2 laser with topical triamcinolone acetonide aqueous solution and Group B received ILS. Both groups received treatment for five settings with each setting a gap of 3 weeks. The efficacy and safety of treatment modalities in both groups were assessed using global photograph assessment (GPA)-scale, lesional area density score percentage of improvement (LAD score improvement %), visual discomfort scale (VDS), visual analogue scale, and documentation of adverse effects in each setting.
Results:
Efficacy of treatment modality-assessed using means score of GPA-scale and LAD score improvement % suggests quicker results to patients in Group B in initial settings but drastic improvement happens to patients in Group A in subsequent settings. At the end of 5th setting, GPA-scale and LAD score improvement % suggest maximum efficacy in patients in Group A and they are statistically significant (P-value < 0.001). The mean VDS in both groups suggests maximum discomfort in Group A, yet the patient satisfaction at the end of 5th setting was maximum with patients in Group A and they are statistically significant (P-value < 0.001). Cosmetic notable adverse effect of atrophy of skin was documented in 30% of patients in Group B.
Conclusion:
This study showed that fractional CO2 laser with topical triamcinolone acetonide is a better treatment modality than the intralesional triamcinolone acetonide for the treatment of AA with respect to efficacy, safety, and adverse events.
Keywords
Alopecia areata
combination therapy
fractional CO2 laser
intralesional steroids
laser-assisted drug delivery
INTRODUCTION
Alopecia areata (AA) is a non-scarring alopecia of chronic autoimmune etiology with heterogenous severity against the anagen hair follicle over the scalp, beard, or any part of the body. AA accounts for 2% of the global general population. The exact etiopathogenesis of AA is very elusive, whereas the most accepted theory is the immune privilege of the hair follicle getting collapsed by unpredictable immunological mechanism. Various genetic and environmental triggers contribute to their etiopathogenesis.[1]
The clinical profile of AA varies significantly. The most common presentation is a smooth, circular, complete patchy loss of hair that has occurred over weeks. This is called patchy AA and it ranges from single to multifocal patchy loss of hair. Special variants of AA include (1) ophiasis, (2) sisaipho, (3) alopecia reticularis, (4) alopecia subtotalis, (5) alopecia totalis, (6) alopecia universalis, (7) perinevoid alopecia, (8) linear alopecia, (9) acute diffuse and total alopecia of the female scalp, and (10) AA incognito.[23]
The clinical course of AA shows unpredictable episodes of relapsing and remission. The undividable response of the patients to various treatment modalities increases the mental struggle and hence association of anxiety and depression in AA is more than the general population.[4]
AA patients seek treatment exclusively for cosmetic reasons. Till now, innumerable local and systemic treatment options are accessible, and their efficacies are varied. Hence the clinical presentation should be assessed before deciding the therapy. Intralesional steroids (ILS) are a proven first-line treatment modality for patchy AA. Patients undergoing ILS should be observed for the notable side effect of atrophy of the skin which is not cosmetically appealing.[5]
Hence there is a hunt for an alternate treatment modality with less side effects and cosmetic concern. Fractional CO2 laser is one among the laser-assisted drug delivery systems. Fractional CO2 laser-assisted drug delivery of steroids for AA is a novel treatment discipline with a paucity of research and literature regarding their efficacy and safety.[6-8]
Thus, this study was proposed to assess and compare the efficacy and safety of fractional CO2 laser in combination with topical triamcinolone acetonide aqueous solution and intralesional triamcinolone acetonide as a monotherapy in the treatment of AA.
MATERIALS AND METHODS
This randomized controlled trial (RCT) hospital-based study was conducted in the outpatient clinic of Department of Dermatology Venereology and Leprosy from January 2021 to July 2022 after the Institutional Ethical Clearance. An informed consent was obtained from AA patients about the participation in the study, disease nature, and the necessity to follow-up.
Patients with patchy AA who had not taken treatment either topical or systemic treatment options in the past 3 months were included in the study. Patients with systemic illnesses—cardiac, renal, and hepatic disorders, immunocompromised patients, pregnant patients were excluded from the study.
Total sample size of 60 cases were screened from January 2021 to July 2022. These patients were divided in to two groups: Group A and Group B with 30 patients in each group and randomization of cases into both groups was done by using computer-generated block randomization from www.randomization.com.
Group A: Fractional CO2 laser with topical triamcinolone acetonide
A topical an aesthetic, containing a mixture of lidocaine—7.0% w/w and tetracaine—7.0% w/w in a cream base was applied for 45 min on the treatment area. After satisfactory topical anesthesia was achieved, the treatment area was cleaned with a gauze dipped in distilled water. Eyes was protected with eye shields. Fractional CO2 laser was then delivered to the AA site at the following setting as shown in Table 1.
| 1. | Power | 30 W |
| 2. | Duration | 1.5 ms |
| 3. | Distance | 0.8 cm |
| 4. | Point energy | 45 mJ/cm2 |
| 5. | Repeat | Single |
| 6. | Times | 2 |
| 7. | Mode | Normal |
Then within 2 min of laser procedure, topical triamcinolone acetonide aqueous solution (2.5–10 mg/mL) was applied depending on the site (10 mg/mL—scalp, 5 mg/mL—beard/mustache, 2.5 mg/mL—eyebrow).
Patients in Group A received fractional CO2 laser with topical triamcinolone acetonide aqueous solution for five settings with each setting a gap of 3 weeks.
Group B: Intralesional triamcinolone acetonide
Triamcinolone acetonide was injected intradermally with an insulin syringe as multiple 0.1 mL injections (4 units) at 1 cm intervals (10 mg/mL—scalp, 5 mg/mL—beard/mustache, 2.5 mg/mL—eyebrow).
Patients in Group B were treated with intralesional triamcinolone acetonide for five settings with each setting a gap of 3 weeks.
Assessment of efficacy and safety profile in both groups were done by using the following scales:
Global photograph assessment (GPA) scale
Lesional area and density (LAD) score percentage of improvement
Visual discomfort scale (VDS)
Visual analogue scale (VAS)
Documentation of adverse effects
The efficacy of the treatment in both groups was assessed using the following scales.
Global photograph assessment scale
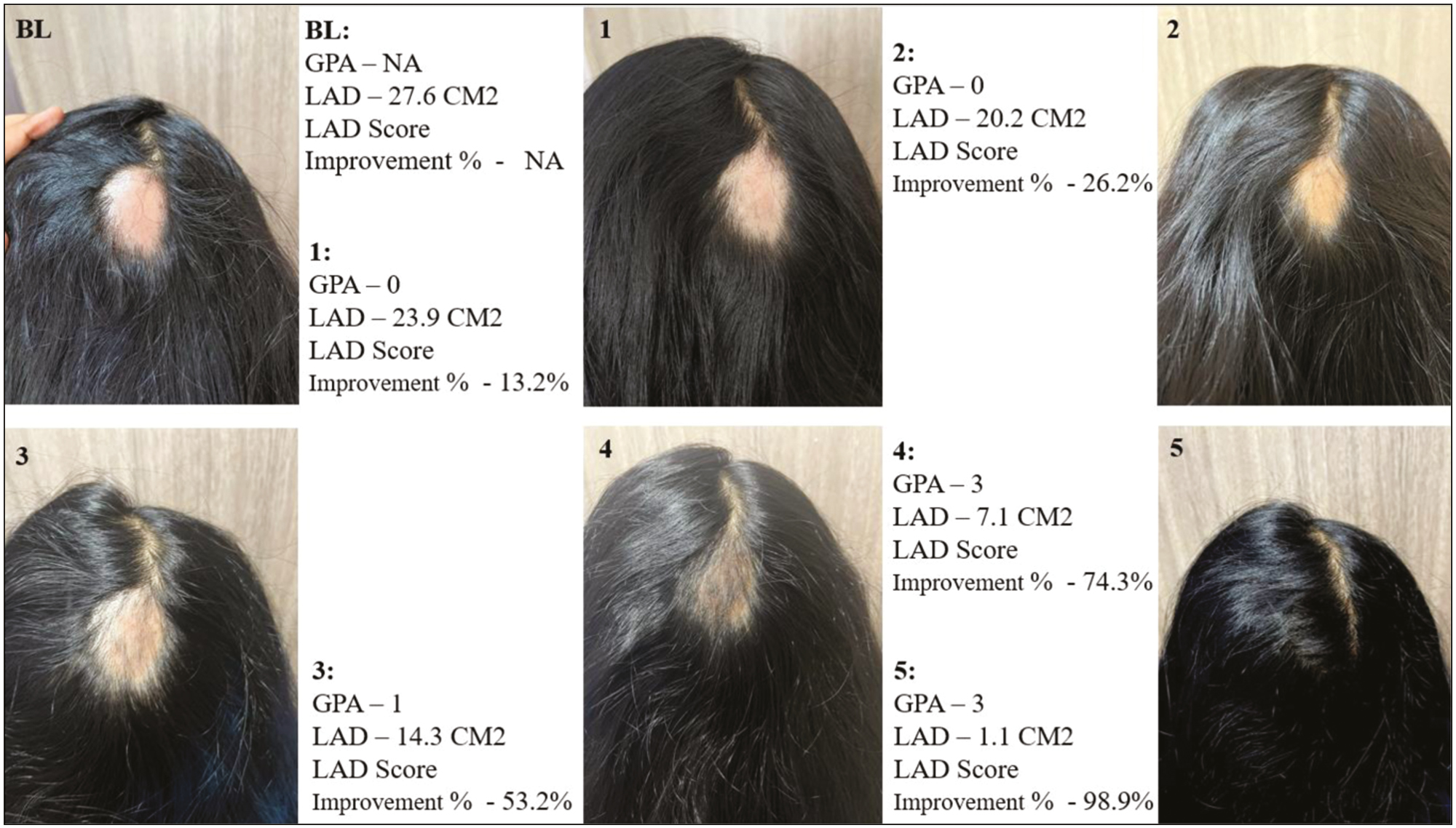
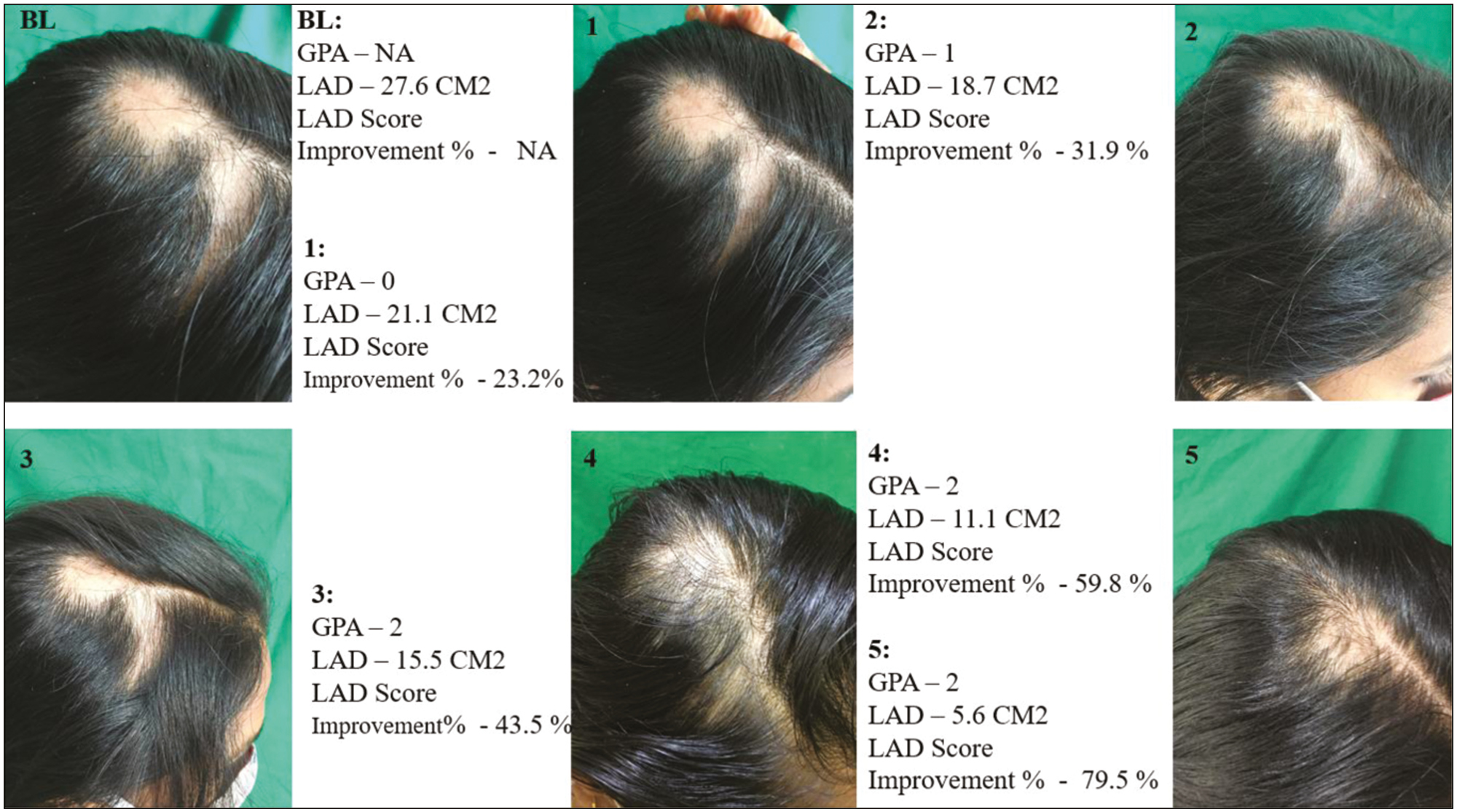
Patients of this study had undergone serial photography of the lesions at baseline and at subsequent settings. Lighting and positioning were kept identical for all serial photographs.
The serial photographs were assessed independently by a blinded third observer. The blinded third observer gave the grading of the efficacy of the treatment modality based on the GPA-scale. GPA-scale was used for all the patients of the study at the baseline presentation and at subsequent follow-up settings.
A score of 0, 1, 2, and 3 was given if the response was <25%, 25%–50%, 51%–75%, and >75%, respectively, by the blinded third observer.
Lesional area and density score percentage of improvement
LAD score percentage of improvement was used to determine the efficacy of the treatment modalities in each group.
LAD score was calculated by the formula:[9]
LAD score was calculated for all the patients of the study at the baseline presentation and at subsequent follow-up settings.
The LAD score percentage of improvement was assessed at each setting with the baseline presentation.
LAD score percentage of improvement was calculated by the formula:
The safety of both treatment modalities was assessed using the following:
-
1)
VDS:
VDS (score ranges from a scale of 0 to 10) was used to record the subjective discomforts of the patients during the procedure such as pain, burning sensation, and any other nonspecific discomforts.
-
2)
VAS:
VAS (score ranges from a scale of 0 to 10) was used to record the satisfaction of the treatment modality as perceived by patients at the end of five settings.
-
3)
Adverse effects:
Post procedural adverse effects were also documented to assess the safety of both the treatment modalities.
Statistical analysis
Study data were entered into a Microsoft Excel Data Sheet. It was then analyzed using SPSS 22.0 software (IBM). ∑ (average) was calculated for GPA and LAD improvement % at the end of all settings and VDS and VAS at the end of 5th setting. Categorical data were represented in the form of frequencies and proportions. Chi-square test or Fischer’s exact test was used as test of significance for qualitative data. Continuous data were represented as mean and standard deviation. Independent t test was used as test of significance to identify the mean difference between two quantitative variables.
P-value < 0.05 was considered as statistically significant after assuming all the rules of statistical tests.
RESULTS
In our study, 41.6% (25 cases) of the patients belonged to the age group of 18–30 years and 38.3% (23 cases) of the patients belonged to the age group of 30–40 years of age.
Among the AA patients in this current study, 77% of cases (46 cases) were males and 23% of cases (14 cases) were females. Our study’s AA patients showed a substantial familial history of AA in 43.3% (26 cases). Patchy AA had previously been treated with a variety of therapeutic modalities in 23.3% (14 cases).
In our study, 51.6% (31 cases) of the AA patients were students (school/college going students), 31.6% (19 cases) were skilled professionals (which includes IT professionals, doctors, bankers, policemen), 10% (6 cases) were semi-skilled workers, and 6.6% (four cases) were unskilled workers.
In the current study, 78.3% (47 cases) of the AA patients gave a history of constant stress in their day-today activities.
At the baseline presentation, 26.6% (16 cases) of the AA patients in our study were having a single patchy AA and 73.3% (44 cases) of the AA patients were having more than one patchy AA.
Regarding the site of patchy AA in our study, 86.6% cases (52 cases) had scalp involvement, 10% cases (6 cases) had beard involvement and 3.3% cases (2 cases) had mustache involvement. Nil cases were enrolled with eyebrow involvement or any other part of the body.
Among the patchy AA patients in our study, 55% (33 cases) of cases had AA surface area > 50 cm2, 26.6% (16 cases) of cases had AA surface area 30–50 cm2 and 18.3% (11 cases) of cases had AA surface area < 30 cm2.
Majority (95%) (57 cases) of the patchy AA patients in our study were asymptomatic. 5% (3 cases) of the patchy AA patients in our study were associated with itching.
Almost 76.6% (46 cases) of the cases in our study resorted treatment for cosmetic non-appealing nature of AA whereas 23.3% (14 cases) of the cases in our study resorted treatment for therapeutic benefit.
The results of GPA-scale were as provided in Table 2.
| Groups | Mean score (∑) | Percentage of cases with GPA-3 at the end of 5th setting | ||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||
| Group A | 0.33 | 1.13 | 2.13 | 3 | 3 | 100% |
| Group B | 0.93 | 1.76 | 2 | 2 | 2.16 | 16.6% |
| P-value | <0.001 | <0.001 | 0.112 | <0.001 | <0.001 | |
The results of LAD score percentage of improvement were provided in Table 3.
| Groups | Mean score (∑) | Percentage of cases with LAD score percentage improvement >90% at the end of 5th setting | ||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||
| Group A | 14.84 | 26.39 | 54.09 | 74.84 | 91.85 | 66.6% |
| Group B | 24.05 | 36.76 | 48.17 | 60.82 | 80.92 | 10% |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
The results of VDS and VAS were provided in Table 4.
| Groups | VDS [mean score (∑)] (out of 10) | VAS [mean score (∑)] (out of 10) | VDS > 5 (out of 10) | VAS ≥ 8 (out of 10) |
|---|---|---|---|---|
| Group A | 6.1 | 8.8 | 83.3% | 100% |
| Group B | 4.3 | 7.43 | 6.6% | 50% |
Efficacy of treatment modality-assessed using mean score of GPA-scale and LAD score improvement % suggests quicker results to patients treated with ILS in initial settings but drastic improvement in GPA-scale and LAD score improvement % happens to patients treated with laser-assisted drug delivery of steroids in subsequent settings. At the end of 5th setting, GPA-scale and LAD score improvement % suggest maximum efficacy in patients treated with laser-assisted drug delivery of steroids.
The mean VDS in both groups suggests maximum discomfort during laser procedure with topical steroids yet the patient satisfaction at the end of 5th setting was maximum in patients undergoing laser procedure with topical steroids.
P-value was <0.001 for GPA-scale and LAD score improvement % at the end of 1st, 2nd, 3rd, 4th, and 5th setting. However, the GPA-scale at the end of third setting was not <0.001 (P-value = 0.112). Hence the data of efficacy of both treatment modalities assessed at the end of 5 settings using GPA-scale and LAD score improvement % were statistically significant.
P-values were <0.001 for VDS and VAS and they were statistically significant.
The documentation of adverse effects was provided in Table 5. Figure 1 and Figure 2 shows the documentation of a case in Group A and Group B respectively.
| Groups | Erythema | Edema | Atrophy of skin | Post inflammatory hyperpigmentation | Bleeding |
|---|---|---|---|---|---|
| Group A (out of 30 cases) | 24 (80%) | 5 (16.6%) | 0 | 8 (26.6%) | 9 (30%) |
| Group B (out of 30 cases) | 3 (10%) | 0 | 9 (30%) | 0 | 12 (40%) |
- Group A
- Group B
DISCUSSION
AA is a non-cicatricial alopecia that has a significant psychological morbidity due to their cosmetic non-appealing presentation. In this study, 41.6% of the study population belonged to the age group of 18–30 years, 77% were men with 78.3% of them having a constant stress in their day-today activities. 86.6% of them had scalp involvement and 95% of them were asymptomatic. Almost 76.6% of them sought treatment for cosmetic benefit rather than therapeutic benefit. This finding is in association with the observations of Juárez-Rendón et al.,[10] Minokawa et al.,[11] Pratt et al.,[12] Strazzulla et al.,[13] and Liu et al.[14] in their studies.
Innumerable treatment options for AA are available with their own side effect profile. ILS being the first-line therapy for patchy AA is often noted with atrophy of skin which is not cosmetic appealing. As a result, researchers are looking for a different type of treatment that has less adverse effects and cosmetic issues. The novel idea of utilizing laser-assisted drug delivery for AA has limited research and hence the primary motive of our research was to compare its efficacy and safety with a proven first-line treatment modality-ILS.
The underlying mechanism of action of fractional CO2 laser as a therapeutic option for AA is presumed to be telogen hairs getting arrested due to the apoptosis of T cells and prolonged anagen hair stage.[1516] Fractional CO2 laser in murine model study shows induction of anagen hairs due to Wnt/β-catenin signaling pathways.[17] Thermal effect caused by laser over papillary dermis stimulates the stem cells in hair bulge.[18] Microthermal treatment zones formed by fractional CO2 laser can act as trans epidermal drug delivery system for topical steroids.[15-18]
In our study, the efficacy of both treatment modalities was assessed using GPA-scale and LAD score improvement %. At the end of 5th setting, the GPA-scale showed a score of 3 (>75% improvement) to all cases treated with lasers followed by topical steroids (100%) and 16.6% of cases treated with ILS. > 90% LAD score improvement % was seen in 66.6% of cases treated with lasers followed by topical steroids and 10% of cases treated with ILS.
In a case series study of utilizing fractional CO2 laser followed by topical steroids for recalcitrant AA by Majid et al.[18] observed seven out of eight cases showed >75% regrowth at the end of three sessions with session a gap of 3 weeks. This finding is consistent with our study where mean LAD improvement % at the end of 4th setting was 74.84% in patients who was treated with fractional CO2 laser followed by topical steroids.
In a study by Halim et al.[19] observed statistically significant reduction in SALT score for 10 patients receiving fractional CO2 laser followed by topical steroids for AA. This finding is consistent with our study.
In a study by Soror et al.[20] compared the effectiveness of fractional CO2 laser with topical triamcinolone with ILS in two different AA patches in the same individual. Their study showed statistically significant higher mean grading score for patches treated with ILS, when compared with patches treated with ablative fractional CO2 laser followed by topical steroids. This finding was statistically significant for the initial two settings of our study where GPA and LAD score improvement % for patients treated with ILS was better than that of fractional CO2 laser followed by topical steroids. Although in subsequent settings, drastic statistically significant GPA and LAD score improvement % for patients treated with fractional CO2 laser followed by topical steroids occur in our study. In the study by Soror et al.[20] two patches of same patient was given separate treatment whereas our study is a RCT involving two groups of patients with different treatment regimens.
In agreement with our study, Majid et al.[18] and Halim et al.[19] documented maximum discomfort in patients undergoing laser treatment for AA. In our study, 83.3% of cases treated with fractional CO2 laser followed by topical steroids had VDS > 5 despite anesthesia over the patch. Only 6.6% of cases treated with ILS had VDS > 5.
In our study, all patients treated with fractional CO2 laser followed by topical steroids (100% cases) had VAS ≥ 8% and 50% of patients treated with ILS had VAS ≥ 8. This finding is consistent with the study done by Majid et al.,[18] Halim et al.,[19] and Soror et al.[20]
In our study, patients treated with fractional CO2 laser followed by topical steroids had more transient adverse effects such as erythema (80% cases) and edema (16.6% cases) which fades away in a day or two. This finding is consistent with the study done by Majid et al.,[18] Halim et al.,[19] and Soror et al.[20] Atrophy of skin was observed in 30% of patients treated with ILS and is consistent with the findings of Yee et al.[21]
CONCLUSION
From the results of our study, it is evident that the patients who require cosmetic improvement for AA are suggested to be treated with laser-assisted drug delivery of potent steroids because it has less to no serious cosmetic adverse effects except few transient adverse effects, post procedure immediately which fades away in a day or two.
However, for patients who require immediate quick response within initial settings—ILS should be considered but complete remission cannot be guaranteed.
But on the long run in our study in subsequent settings, laser-assisted drug delivery of potent steroids is proven to be cosmetically pleasing and therapeutically beneficial with minimal adverse effects.
Hence, fractional CO2 laser with topical triamcinolone acetonide is a better treatment modality than the intralesional triamcinolone acetonide for the treatment of AA with respect to efficacy, safety, and adverse events.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This work was supported by Indian Council of Medical Research (ICMR).
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Alopecia areata: An update on etiopathogenesis, diagnosis, and management. Clin Rev Allergy Immunol. 2021;61:403-23.
- [Google Scholar]
- Alopecia areata: A review on diagnosis, immunological etiopathogenesis and treatment options. Clin Exp Med. 2021;21:215-30.
- [Google Scholar]
- Alopecia areata: New treatment options including janus kinase inhibitors. Dermatol Clin. 2021;39:407-15.
- [Google Scholar]
- Alopecia areata: A multifactorial autoimmune condition. J Autoimmun. 2019;98:74-85.
- [Google Scholar]
- Alopecia areata: An appraisal of new treatment approaches and overview of current therapies. J Am Acad Dermatol. 2018;78:15-24.
- [Google Scholar]
- Comparative study between fractional carbon dioxide laser vs intralesional steroid injection in treatment of alopecia areata. Dermatol Ther. 2020;33:e13742.
- [Google Scholar]
- Fractional laser-assisted hair regrowth and microneedling for the treatment of alopecia areata: A review. Cureus. 2019;11:e4943.
- [Google Scholar]
- Lessons learned from the first decade of laser-assisted drug delivery. Dermatol Ther (Heidelb). 2021;11:93-104.
- [Google Scholar]
- Objective outcome measures: Collecting meaningful data on alopecia areata. J Am Acad Dermatol. 2018;79:470-8.e3.
- [Google Scholar]
- Alopecia areata. Current situation and perspectives. Arch Argent Pediatr. 2017;115:404-11.
- [Google Scholar]
- Lifestyle factors involved in the pathogenesis of alopecia areata. Int J Mol Sci. 2022;23:1038.
- [Google Scholar]
- Alopecia areata: Disease characteristics, clinical evaluation, and new perspectives on pathogenesis. J Am Acad Dermatol. 2018;78:1-12.
- [Google Scholar]
- Alopecia areata is associated with impaired health-related quality of life: A survey of affected adults and children and their families. J Am Acad Dermatol. 2018;79:556-558.e1.
- [Google Scholar]
- Treatment of alopecia areata with fractional photothermolysis laser. Int J Dermatol. 2010;49:845-7.
- [Google Scholar]
- Clinical effects of non-ablative and ablative fractional lasers on various hair disorders: A case series of 17 patients. J Cosmet Laser Ther. 2013;15:74-9.
- [Google Scholar]
- Hair regrowth through wound healing process after ablative fractional laser treatment in a murine model. Lasers Surg Med. 2015;47:433-40.
- [Google Scholar]
- fractional carbon dioxide laser in combination with topical corticosteroid application in resistant alopecia areata: A case series. J Cutan Aesthet Surg. 2018;11:217-21.
- [Google Scholar]
- Evaluation of fractional carbon dioxide laser alone versus its combination with betamethasone valerate in treatment of alopecia areata, a clinical and dermoscopic study. Arch Dermatol Res. 2023;315:505-11.
- [Google Scholar]
- Fractional carbon dioxide laser-assisted topical steroid delivery versus intralesional steroid in the treatment of alopecia areata. J Egypt Womens Dermatol Soc. 2021;18:43-51.
- [Google Scholar]
- Efficacy of different concentrations of intralesional triamcinolone acetonide for alopecia areata: A systematic review and meta-analysis. J Am Acad Dermatol. 2020;82:1018-21.
- [Google Scholar]






