Translate this page into:
A Comparative Study of Microneedling Alone Versus Along with Platelet-Rich Plasma in Acne Scars
Address for correspondence: Dr Meghna Gupta, 17, Naya Ganj Ghaziabad, Uttar Pradesh, New Delhi, India. E-mail: meghnagupta16@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Context:
There are several modalities of treating acne scars. The combination of microneedling and platelet-rich plasma (PRP) is a synergistic approach to treat acne scars.
Aims:
The aim was to compare the efficacy of microneedling alone versus microneedling with PRP in acne scars.
Materials and Methods:
This was a split face study conducted on 36 patients with acne scars who underwent four sessions of microneedling with PRP on right side and microneedling alone on left side at monthly interval. The total scars with subtypes and Ecchelle D’Evaluation Cliniques des Cicatrices D’Acne (ECCA) score were assessed at baseline and second, fourth, and sixth visits. Visual analog score (VAS) was evaluated by both physicians and patients.
Statistical Analysis:
The statistical analysis was carried out using Statistical Package for Social Sciences. Paired-t test and Wilcoxon signed rank test were used to compare the results.
Results:
Mean age was 23.7±3.2 years with 17 male and 19 female patients. The mean total scars on right and left sides declined from 42.14±21.15 to 25.08±14.14 and 43.28+23.08 to 27.17±15.68, respectively, with insignificant differences (P-value = 0.094). ECCA score on right and left sides declined from 88.31±32.78 to 62.92±23.68 and 89.58±32.43 to 66.25±23.89, respectively (P-value = 0.058). VAS evaluated by patient and physician showed maximum improvement at second and third visits, respectively.
Conclusions:
This study showed no added advantage of topical application of PRP over microneedling in acne scars.
Keywords
Acne scars
microneedling
platelet-rich plasma
INTRODUCTION
It has been observed that 95% of acne patients develop some degree of facial scarring, which has a psychosocial impact on its sufferers.[12]
Various therapeutic modalities are available for smoothening atrophic acne scars like microneedling, subcision, laser resurfacing, punch excision, microdermabrasion, chemical peeling, dermal fillers and grafts, focal treatment with trichloroacetic acid, and platelet-rich plasma (PRP).[3] All these procedures have been used alone or in combination.
Microneedling is a popular technique to create micropunctures in the dermis, which leads to release of various growth factors (GFs) resulting in neovascularization and neocollagenation leading to leveling up of atrophic scars.[34] Microneedling has been used in combination with many other treatment modalities such as subcision, PRP, chemical peels, etc.[567]
PRP is portion of plasma obtained from blood containing four to seven times higher concentration of platelets.[8] PRP has beneficial effects in healing of chronic skin ulcers, skin rejuvenation, alopecia, and post acne scars.
Microneedling releases various GFs, and PRP is an elixir of GFs which stimulate cell proliferation, differentiation, angiogenesis, and collagen deposition; hence, it can be assumed that combination of both will give better cosmetic results.
MATERIALS AND METHODS
We undertook a split face study to evaluate the clinical profile and to compare the efficacy of microneedling alone versus microneedling with PRP in atrophic acne scars. A total of 36 patients of age 18–50 years were included. Patients who had undergone any skin resurfacing procedures within the preceding 1 year and those taking systemic retinoids or immunosuppressive drugs during or within 6 months, with history of coagulation defects or bleeding diathesis, tendency to develop keloid scars and with active acne lesions were excluded.
ETHICAL CONSIDERATION
This study was approved by Institutional Ethics Committee, Maulana Azad Medical College, New Delhi, India. Written informed consent was taken from all the subjects enrolled in the study.
TREATMENT
Pre-procedure
Detailed clinical history and examination findings were recorded in preset Performa. Detailed examination of the face was done to assess the number, distribution, and type of post acne scars. Acne scars were scored according to Ecchelle D’Evaluation Cliniques Des Cicatrices D’Acne grading (ECCA).[9] Acne scars were divided according to the classification system devised by Jacob et al.,[10] named as icepick, boxcar, rolling scars. Patients were also evaluated for improvement on VAS by both physician and patient. Complete blood count, bleeding time and clotting time, serum reactivity for HIV, hepatitis B, and hepatitis C antigen were done. Pre-treatment and post-treatment photographs were taken.
PRP was prepared by double spin method. An aliquot of 8.5 mL of patient whole blood was collected in a tube containing 1.5 mL acid citrate dextrose. The whole blood was centrifuged at 1400 rpm for 10 min to separate buffy coat and plasma from RBC sediments [Figure 1A]. This supernatant was centrifuged at 3500 rpm for 10 min to get PRP (platelet-rich pellet with lower one-fourth of the plasma formed at the bottom of the vial) [Figure 1B]. Calcium gluconate was added as an activator (1:9), i.e. 1 mL of calcium gluconate in 9 mL of PRP.
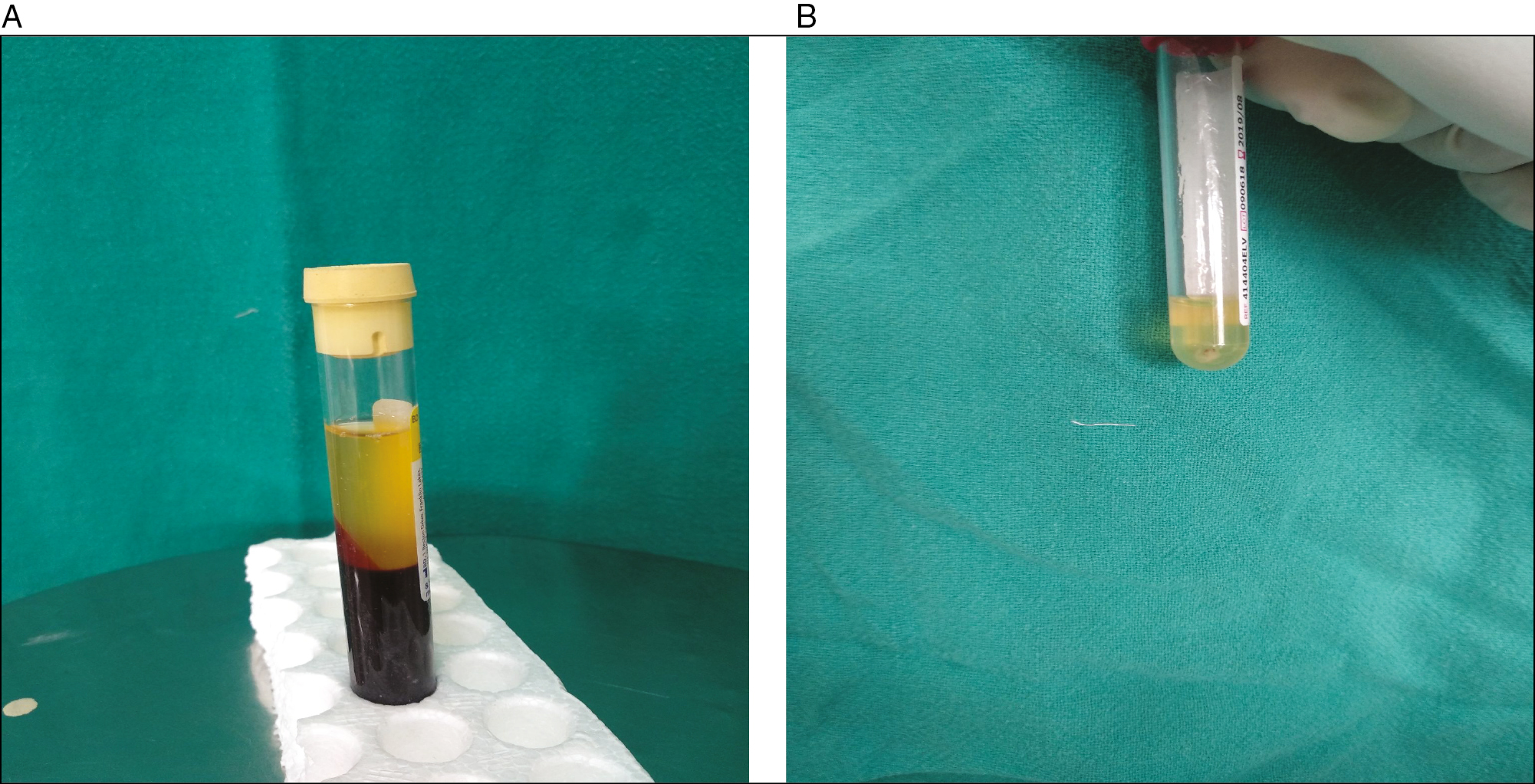
- A: Plasma separated from the RBC sediments. Platelet-rich pellet formed at the bottom of the vial. B: Platelet-rich pellet formed at the bottom of the vial
Procedure
As a standard procedure, right side of the face was subjected to microneedling with PRP and left side of the face was subjected to microneedling alone.
Topical anesthesia, lidocaine 2.5% plus prilocaine 2.5% cream, was applied under occlusion 1 h pre-operatively on the face. Patients were placed in a recumbent position, and the treatment area was cleaned and draped in a sterile manner. The dermaroller was rolled over both sides of the face (192 microneedles diameter 0.25 mm and needle length 2.0 mm) four times in four directions: horizontally, vertically, and diagonally right and left. The appearance of uniform pinpoint bleeding was considered end point of the treatment [Figure 2]. The oozing serum and blood were cleaned with saline soaked gauze and PRP gel was applied and spread by gloved finger over the face which was then left for 1 h [Figure 3].

- Pinpoint bleeding seen on face after microneedling

- Activated PRP applied on microneedled face
Post-procedure care
Patients were advised photoprotection and broad-spectrum sunscreen after treatment. They were reassured of the temporary erythema which may persist for few hours and were asked to report back if any crusting or pigmentation appeared.
Patients were evaluated and subsequent sittings were given in similar manner monthly intervals till a total of four sittings.
EVALUATION
The response to treatment on both sides was assessed on the basis of total scar count of each type and ECCA score, calculated at first, second, fourth, and sixth visits. Visual analog score (VAS) was evaluated by both physicians and patients in every visit.
Statistical analysis
The statistical analysis was carried out using Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA, version 17.0 for Windows). Paired-t test and Wilcoxon signed rank test were used to compare the results.
RESULTS
Out of 40, 36 patients completed the study. The clinic-demographic details of the studied individuals are given in Table 1. Majority of the patients (86%) were in the age group of 21–30 years with mean age of 23.7±3.2 years. There were 17 male and 19 female patients. Twenty-five patients had all the three types of scars. Most common type of scars in patients was boxcar scars (39%), followed by icepick (34%) and rolling scars (27%).
| Characteristics of patients | Distribution (number of patients) |
|---|---|
| Age (years) | |
| <21 | 4 |
| 21–30 | 31 |
| 31–40 | 1 |
| >40 | 0 |
| Sex | |
| Males | 17 |
| Females | 19 |
| Marital status | |
| Married | 3 |
| Unmarried | 33 |
| Employment | |
| Employed | 19 |
| Unemployed | 17 |
| Age of onset of scars (years) | |
| <14 | 2 |
| 14–20 | 29 |
| >20 | 5 |
| Family history of acne scars | |
| Present | 7 |
| Absent | 29 |
| Types of scars | |
| Rolling | 31 |
| Boxcar | 31 |
| Icepick | 34 |
At baseline, the mean of total scars on right and left sides was 42.14 ± 21.15 and 43.28 ± 23.08, respectively, with insignificant differences (P ≤ 0.05). Mean ECCA score was almost the same on both the sides with mean values on right and left sides being 88.31 ± 32.78 and 89.58 ± 32.43, respectively.
All the patients showed significant improvement on both the sides of face at the end of study period [Figures 4 and 5].
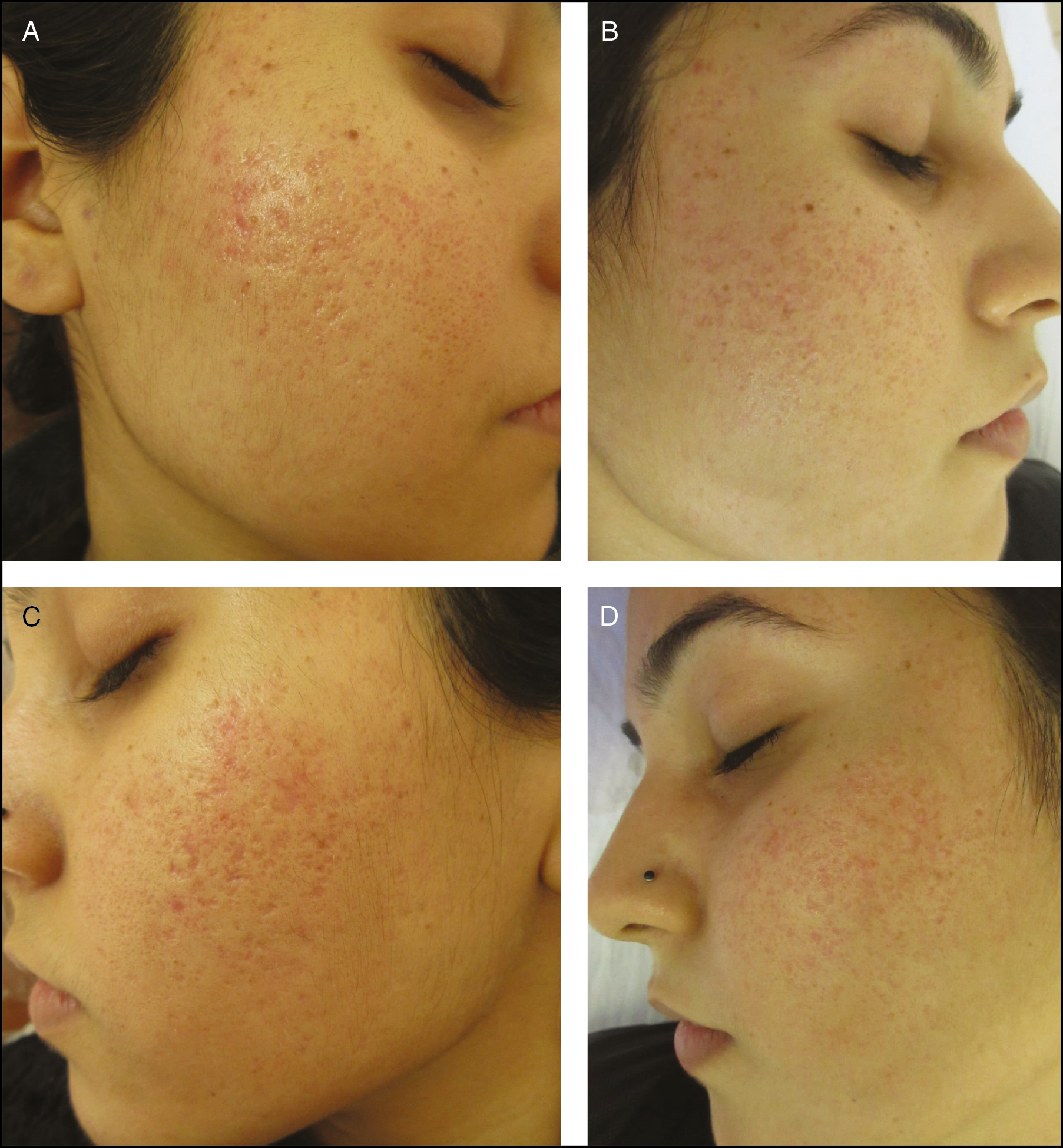
- A: Pre-treatment photograph of a patient with acne scars. B: Post-treatment photograph of a patient with acne scars after four sessions of microneedling with PRP. C: Pre-treatment photograph of a patient with acne scars. D: Patient with acne scars after four sessions of microneedling alone
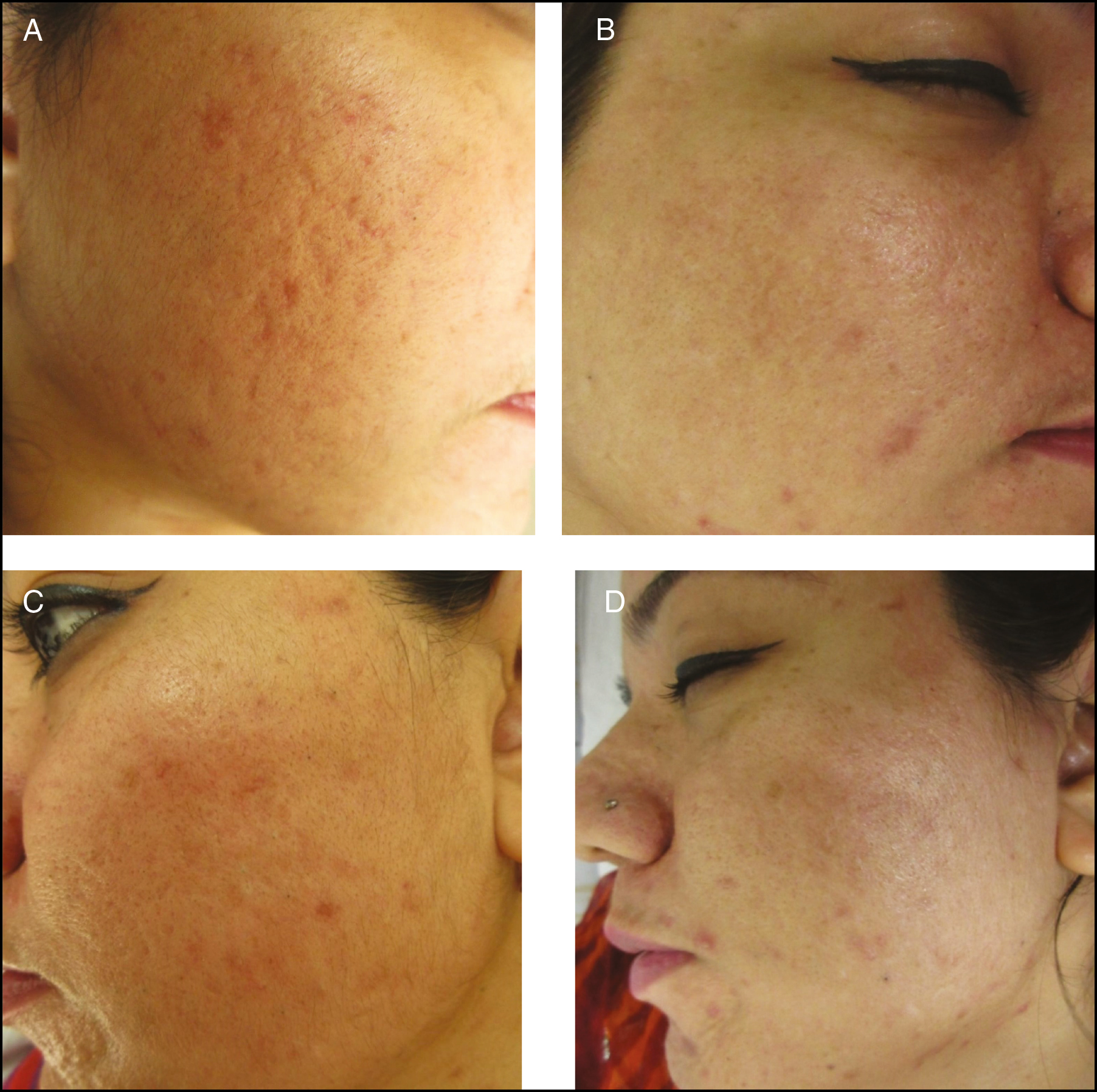
- A: Pre-treatment photograph of a patient with acne scars. B: Post-treatment photograph of a patient with acne scars after four sessions of microneedling with PRP. C: Pre-treatment photograph of a patient with acne scars. D: Patient with acne scars after four sessions of microneedling alone
The reduction in mean boxcar scars count was observed to be significant from second visit onwards; however, maximum improvement was seen after three sessions. The mean boxcar scars on right and left sides declined from 15.42 ± 13.34 to 9.53 ± 7.36 and 17.42 ± 18.32 to 10.31 ± 8.68 (P = 0.204), respectively.
In icepick scars, the reduction was maximum at the fourth visit. The mean icepick scars on right and left sides declined from 14.92 ± 16.14 to 11.19 ± 12.33 and from 14.33 ± 14.08 to 11.39 ± 11.61, respectively, with insignificant differences (P = 0.772).
The improvement in rolling scars started from second visit onwards and continued at fourth and sixth visits. The mean rolling scars on right and left sides declined from 11.75 ± 10.89 to 4.39 ± 4.09 and from 11.39 ± 10.46 to 4.50 ± 5.01, respectively, with insignificant differences (P = 0.817).
The mean total scars on right and left sides declined from 42.14 ± 21.15 to 25.08 ± 14.14 and from 43.28 ± 23.08 to 27.17 ± 15.68, respectively [Figure 6]. The difference on both the sides was statistically insignificant (P = 0.094).
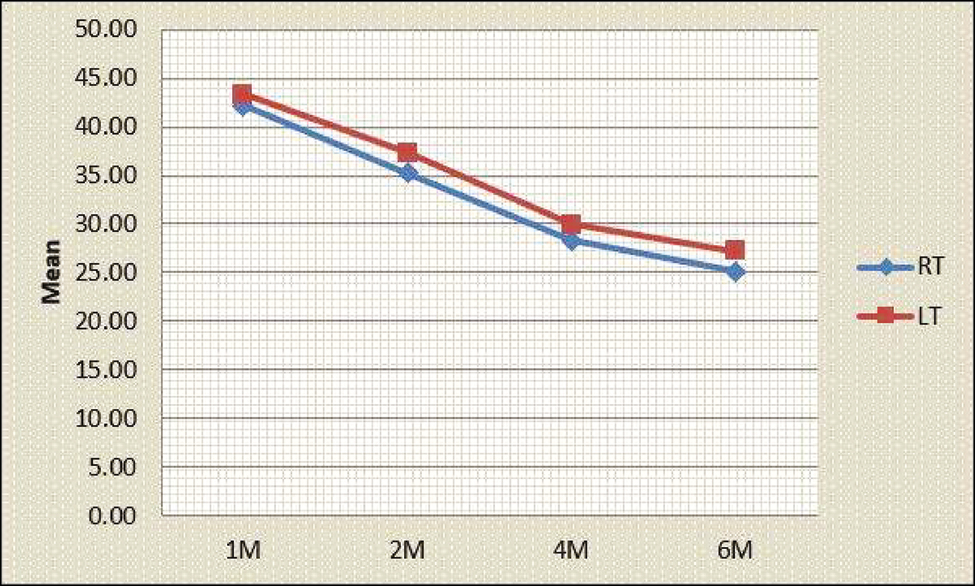
- Comparison of total scars on both the sides (RT and LT: mean of total scars on right and left sides of face, respectively, in all patients)
The improvement after four sessions was maximum for rolling scars followed by boxcar scars.
The ECCA score decreased significantly on both the sides after second, fourth, and sixth visits. The mean ECCA score on right and left sides declined from 88.31 ± 32.78 to 62.92 ± 23.68 and from 89.58 ± 2.43 to 66.25 ± 23.89, respectively, with insignificant differences (P = 0.058) [Figure 7].
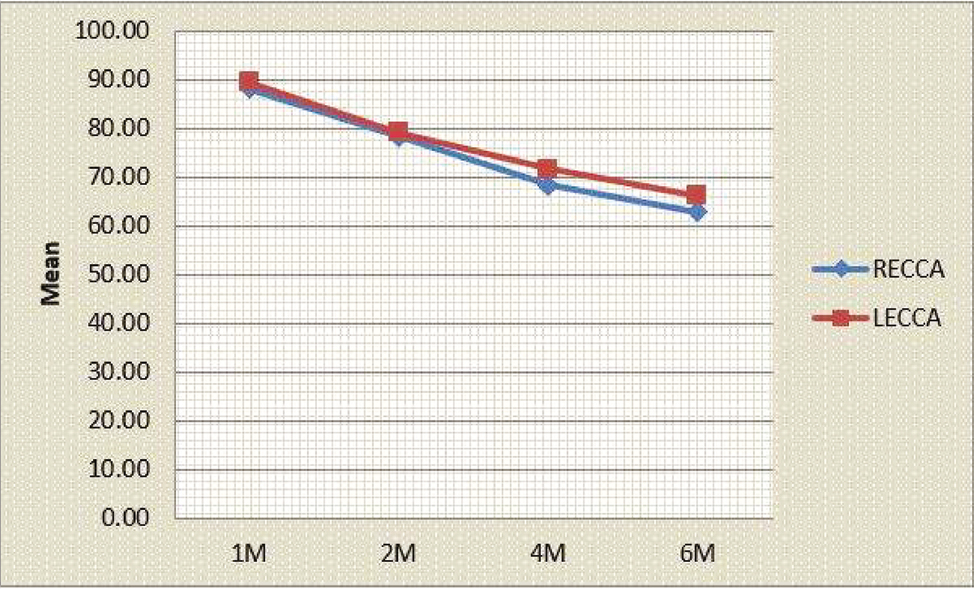
- Comparison of ECCA score on both the sides (RECCA and LECCA: mean of total ECCA score on right and left sides of face, respectively, in all patients)
The VAS evaluated by patients showed maximum improvement at second visit on both the sides. On the right side, six patients showed marked, 22 patients showed moderate, and eight patients showed mild improvement. On the left side, six patients showed marked, 21 patients showed moderate, and nine patients showed mild improvement. There were statistically insignificant differences on both the sides of face in every visit [Figure 8].
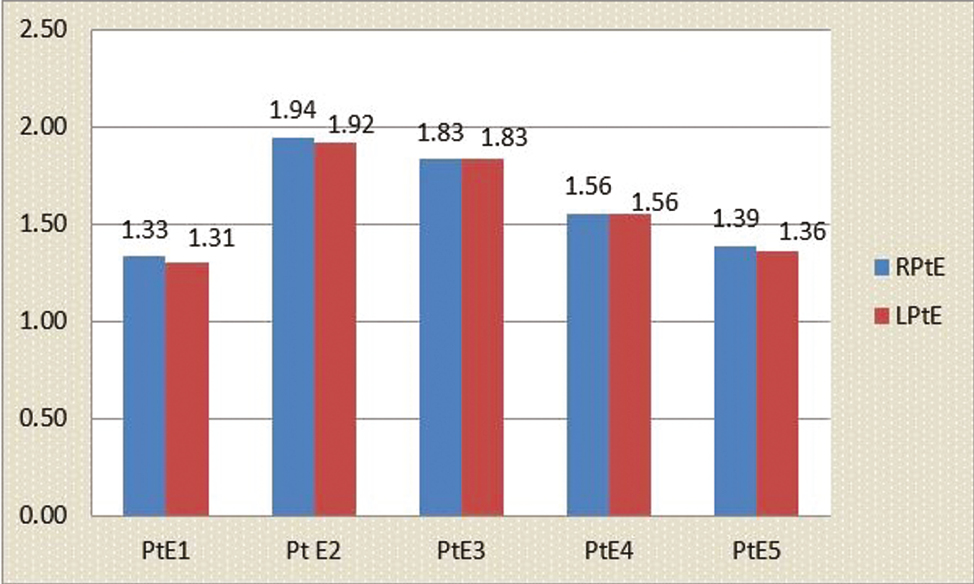
- Graph showing a comparison of the mean of VAS by the patient of all visits on both the sides (RPtE and LPtE: VAS by the patient on right and left sides of the face every month)
On VAS evaluated by physician, maximum improvement was seen at third visit on both the sides. On the right side, 25 patients showed moderate and 11 patients showed mild improvement. On the left side, 23 patients showed moderate and 13 patients showed mild improvement. The differences on both the sides were insignificant [Figure 9].
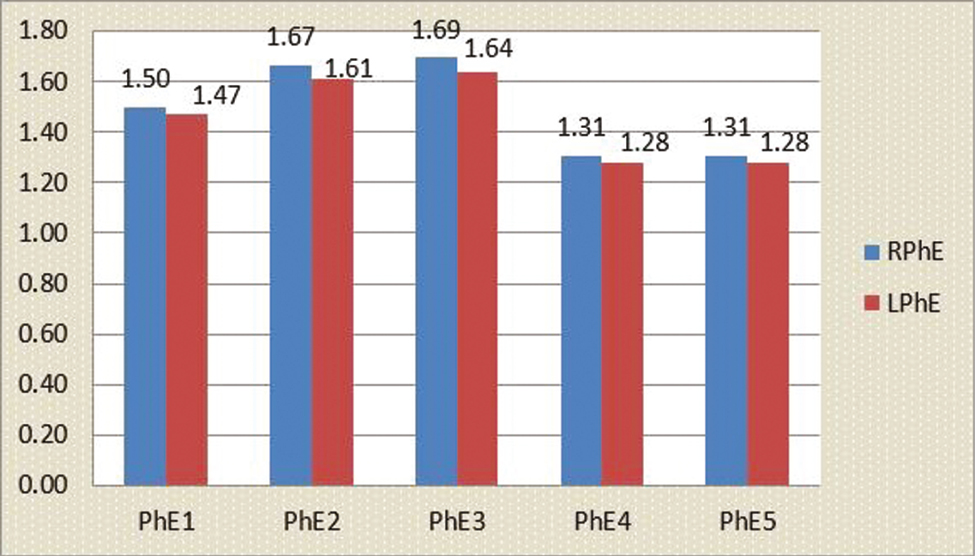
- Graph showing comparison of mean of VAS by physician of all visits on both the sides (RPhE and LPhE: VAS by the physician on right and left sides of the face every month)
Erythema and edema lasted for 1 and 2–3 days, respectively. Only two patients developed post-inflammatory hyperpigmentation which resolved in 2 weeks after topical application with tretinoin. No difference in side effect profile was seen on both the sides.
DISCUSSION
All types of acne have been associated with scars, but nodulocystic acne more commonly develops acne scars.[2] In a clinical survey, 49% of the total patients with acne had acne scars.[11]
Face was the most common site for acne scars (95%), followed by trunk.[2] Risk factors for acne scarring include severe inflammatory acne, time elapsed before treatment for acne scars starts, manipulation of lesions, family history of acne scarring, and involvement of trunk and frequent relapses.[12]
Many therapeutic approaches, both invasive and non-invasive, are used to treat acne scars but are marginally ineffective or causing considerable morbidity. These modalities can be energy-based devices such as ablative and non-ablative lasers, fractional radiofrequency, intense pulsed light, and plasma skin regeneration and non-energy-based devices include subcision, microneedling, dermal fillers, and chemical peels.
Microneedling, also called collagen induction therapy (CIT), percutaneous collagen induction (PCI), needle dermabrasion, and intradermabrasion, involves repetitive puncturing of the skin using sterilized microneedles causing percutaneous collagen induction.[413,14]
The micropunctures produced in epidermis are approximately four cells in diameter. The needle seems to divide the cells from each other rather than cutting through the cells with 250–300 pricks per square centimeter. The target when we needle the dermis is intermediate reticular layer which contains maximum number of stem cells which produces maximum collagen. These micro-injuries set up a wound healing cascade with release of various GFs such as platelet derived GF, transforming GF-alpha, transforming GF-beta, fibroblast GF, connective tissue activating protein, and connective tissue GF.[3] Neovascularization and neocollagenesis are initiated by migration and proliferation of fibroblasts and laying down of intercellular matrix.[3] The needles also break the old hardened scar strands.
In a study, histological examination carried out of the skin treated with four microneedling sessions 1 month apart showed up to 400% increase in collagen and elastin deposition at 6 months postoperatively, with a thickened stratum spinosum and normal rete ridges at 1 year post-operatively.[15] Collagen fiber bundles changes to normal lattice pattern from the parallel bundles present in scar tissue.[16]
In 1970, PRP was first used as a transfusion product to treat thrombocytopenia and subsequently it was used in sports injuries, cardiac surgery, pediatric surgery, gynecology, urology, plastic surgery, and ophthalmology.[17] In dermatology, it is used for tissue regeneration, wound healing, scar revision, skin rejuvenating effects, and alopecia.[1819]
PRP contains around 20 types of GFs including vascular endothelial GF, fibroblast GF, endothelial GF, matrix metalloprotein-2, 9, and interleukin-8. The various GFs are mitogenic for smooth muscle cells and fibroblasts and stimulate fibroplasia and angiogenesis and proliferation of fibroblasts.[20]
Various studies had evaluated the efficacy of microneedling for the management of atrophic acne scars. Fabbrocini et al.[3] found that severity of rolling scars significantly decreased with two sessions of microneedling. Dogra et al.[21] found a mean improvement of 50–75% after five sittings in acne scars. Majid[22] assessed efficacy of microneedling in 36 patients with excellent response in 80% patients. Sharad[5] assessed the efficacy of microneedling alone versus combination of microneedling and 35% glycolic acid peels in 30 patients for the management of acne scars with 31% and 60% improvement after five sittings.
All the studies showed moderate improvement in post acne scars with two to five sessions of microneedling with gap between two sessions being 4–8 weeks.[323,24] In our study, we did four sittings of microneedling at 1-month interval. Most of the patients showed moderate grade improvement in acne scars, with maximum improvement in rolling scars followed by boxcar scars. Icepick scars also showed improvement in our study; it may be due to the use of dermaroller with 2 mm needles which might have enhanced the penetration of needle in the skin and remodeling effect on deep icepick scars. Other studies have used dermaroller with 1.5 mm needles.
PRP has been evaluated for its benefits in the treatment of acne scars. A split face study showed no significant differences between the topical and intradermal L-PRP treatment after fractional carbon dioxide laser treatment for acne scars.[24] There are few studies comparing efficacy of microneedling with PRP; however, mostly studies used intradermal injections of PRP.
A study evaluating the efficacy of microneedling with intralesional PRP and microneedling with intralesional distilled water in post acne scars observed 62% and 45.8% improvement, respectively.[25] Ibrahim et al.[26] included 90 patients with atrophic scars, with 28 patients treated with microneedling monthly, 34 patients treated with intradermal injection of PRP, 28 patients treated with alternative sessions of microneedling and intradermal PRP each with mean improvement of 39.71±13.06, 48.82 ± 23, and 70.43 ± 13.32, respectively, with higher response in patients treated with microneedling with intradermal PRP.
Few studies also assessed topical PRP with microneedling in atrophic acne scars; however sample size was limited, with comparison of photographic records with no objective assessment being done.[624]
Fabbrocini et al.[6] found that two sessions with skin needling after topical application of PRP showed improvement in acne scarring. Chawlaet al.[23] showed better efficacy of microneedling with topical PRP than microneedling with vitamin C. However, microneedling was performed after topical application of PRP which might be the reason for better results unlike the present study. Porwal et al.[27] compared the Dermatology Life Quality Index of patients treated with microneedling alone and microneedling with PRP in acne scars, with 42.67% and 58.47% improvement, respectively, after three sessions.
Ibrahim et al.[28] did a split face study comparing microneedling alone and microneedling with PRP in 35 patients. Patients underwent four sessions with final assessment after 3 months with insignificant improvement in both the sides.
At the end of our study, mean percentage reduction of total number of scars was 40% on the right side and 37% on the left side and the difference between the two was insignificant.
Rolling scars responded the most followed by boxcar scars. although the difference between both the sides was insignificant. Icepick scars responded the least.
Sharad[5] found that maximum improvement with microneedling was seen with rolling scars followed by boxcar scars. Ibrahim et al.[26] showed microneedling with PRP showed increased efficacy to boxcar and icepick scars. Our findings are in concordance with these.
Improvement in ECCA score on the right and left sides was 29% and 26%, respectively, from the baseline with insignificant difference on both the sides after 6 months.
It was observed that post-inflammatory hyperpigmentation and macular erythematous scars also decreased in few patients.
The side effects profile was also similar to adverse effects observed in other studies.[2122] No difference in side effect profile was seen on both the sides. Ibrahim et al.[28] found that erythema and edema lasted for less duration on the side treated by microneedling with PRP.
It is apparent from our study that topical PRP had no added advantage over microneedling. It might be due to the following reasons in the present study: no occlusion was done after application of PRP, decreasing the absorption of PRP from microneedling, created micro-channels; we did not repeat microneedling after topical application of PRP for further enhancing penetration of PRP; PRP penetrated well but had no added efficacy.
The sample size was small, observer bias was present to score the scars, and patients were lost to follow-up. Hence, more studies are required with large sample size to validate the results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- A clinical evaluation of acne scarring and its incidence. Clin Exp Dermatol. 1994;19:303-8.
- [Google Scholar]
- Percutaneous collagen induction: An alternative to laser resurfacing. Aesthet Surg J. 2002;22:307-9.
- [Google Scholar]
- Combination of microneedling and glycolic acid peels for the treatment of acne scars in dark skin. J Cosmet Dermatol. 2011;10:317-23.
- [Google Scholar]
- Combined use of skin needling and platelet-rich plasma in acne scarring treatment. J Cosmet Dermatol. 2011;24:177-83.
- [Google Scholar]
- A split-face comparative study to evaluate efficacy of combined subcision and dermaroller against combined subcision and cryoroller in treatment of acne scars. J Cosmet Dermatol. 2014;13:38-43.
- [Google Scholar]
- Platelet-rich plasma (PRP): What is PRP and what is not PRP? Implant Dent. 2001;10:225-8.
- [Google Scholar]
- ECCA grading scale: An original validated acne scar grading scale for clinical practice in dermatology. Dermatology. 2007;214:46-51.
- [Google Scholar]
- Acne scarring: A classification system and review of treatment options. J Am Acad Dermatol. 2001;45:109-17.
- [Google Scholar]
- An epidemiological study of acne in female adults: Results of a survey conducted in France. J Eur Acad Dermatol Venereol. 2001;15:541-5.
- [Google Scholar]
- Prevalence and risk factors of acne scarring among patients consulting dermatologists in the USA. J Drugs Dermatol. 2017;16:97-102.
- [Google Scholar]
- Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg. 1995;21:543-9.
- [Google Scholar]
- Percutaneous collagen induction therapy: An alternative treatment for scars, wrinkles, and skin laxity. Plast Reconstr Surg. 2008;121:1421-9.
- [Google Scholar]
- Is the use of autologous platelet-rich plasma gels in gynecologic, cardiac, and general, reconstructive surgery beneficial? Curr Pharm Biotechnol. 2012;13:1163-72.
- [Google Scholar]
- Autologous platelet-rich plasma: A potential therapeutic tool for promoting hair growth. Dermatol Surg. 2012;38:1040-6.
- [Google Scholar]
- The use of platelet-rich plasma in plastic surgery: A systematic review. J Plast Reconstr Aesthet Surg. 2013;66:301-11.
- [Google Scholar]
- Applications of platelet-rich fibrin matrix in facial plastic surgery. Facial Plast Surg. 2009;25:270-6.
- [Google Scholar]
- Microneedling for acne scars in asian skin type: An effective low cost treatment modality. J Cosmet Dermatol. 2014;13:180-7.
- [Google Scholar]
- Microneedling therapy in atrophic facial scars: An objective assessment. J Cutan Aesthet Surg. 2009;2:26-30.
- [Google Scholar]
- Split face comparative study of microneedling with PRP versus microneedling with vitamin C in treating atrophic post acne scars. J Cutan Aesthet Surg. 2014;7:209-12.
- [Google Scholar]
- Autologous platelet rich plasma: Topical versus intradermal after fractional ablative carbon dioxide laser treatment of atrophic acne scars. Dermatol Surg. 2014;40:152-61.
- [Google Scholar]
- Combined autologous platelet rich plasma with microneedling versus microneedling with distilled water in the treatment of atrophic scars: A concurrent split face study. J Cosmet Dermatol. 2015;0:1-10.
- [Google Scholar]
- Therapeutic effect of microneedling and autologous platelet-rich plasma in the treatment of atrophic scars: A randomized study. J Cosmet Dermatol. 2017;16:388-99.
- [Google Scholar]
- A comparative study of combined dermaroller and platelet-rich plasma versus dermaroller alone in acne scars and assessment of quality of life before and after treatment. Indian J Dermatol. 2018;63:403-8.
- [Google Scholar]
- Skin microneedling plus platelet-rich plasma versus skin microneedling alone in the treatment of atrophic post acne scars: A split face comparative study. J Dermatolog Treat. 2018;29:281-6.
- [Google Scholar]






