Translate this page into:
A comparative study to evaluate the safety and efficacy of low-dose isotretinoin monotherapy versus a combination of low-dose isotretinoin and superficial chemical peels in patients with moderate-to-severe acne vulgaris
*Corresponding author: Kolluri Siva Bala Vaishnavi, Department of Dermatology, Mallareddy Institute of Medical Sciences, Secunderabad, Telangana, India. ksbvaishnavi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Siva Bala Vaishnavi K, Vijaya Lakshmi C, Chandrapola V, Sompalli S, Kavya M, Spandana P. A comparative study to evaluate the safety and efficacy of low-dose isotretinoin monotherapy versus a combination of low-dose isotretinoin and superficial chemical peels in patients with moderate-to-severe acne vulgaris. J Cutan Aesthet Surg. doi: 10.25259/jcas_70_24
Abstract
Objectives:
The aim of the study was to compare the safety and efficacy of low-dose isotretinoin (LDI) monotherapy versus a combination of LDI and superficial chemical peels in treating moderate-to-severe acne in patients attending tertiary care hospital.
Material and Methods:
Sixty patients in the age group of 15–45 years having moderate-to-severe acne vulgaris were enrolled in the study. The patients were randomly divided into two groups of 30 patients each by random table number method. Group A – patients were put on LDI (0.25 mg/kg body weight [wt]) for 3 months. Group B – LDI (0.25 mg/kg body weight) was started, and these patients were subjected to six sessions of sequential superficial chemical peels every fortnightly for 3 months.
Results:
Treatment outcome was measured in terms of improvement in global acne grading (GAG) score, pigmentation, scarring, and seborrhea. The mean GAG score at week 0 in Group A was 29.2 ± 5.03, and Group B was 26.7 ± 5.11. The mean GAG score at week 12 in Group A was 15.9 ± 5.09, and in Group B was 9.23 ± 3.24, which showed statistically significant improvement (P < 0.001) in both groups. Post-inflammatory hyperpigmentation and erythema also improved significantly. There was no significant improvement in scarring, yet Group B showed a better response. The patient satisfaction score was high in Group B. Seborrhea improved equally in both groups.
Conclusion:
LDI gives a good balance between efficacy- and dose-related side effects. Both groups showed statistically significant results in terms of acne severity (global acne grading system (GAGS) W-0 26–29–W12 15– 9). Group B showed faster improvement than Group A.
Keywords
Acne
Low-dose isotretinoin
Superficial chemical peels
Global acne grading score
INTRODUCTION
Acne vulgaris is a common inflammatory disorder of the pilosebaceous unit, which has a chronic course in most patients. It commonly manifests as comedones, papules, pustules, or nodules, mostly on the face; it can also affect the upper arms, trunk, and back. Although it is predominantly seen in adolescents, it is not restricted to this age group and can affect individuals of various ages. Cutibacterium acnes, under the influence of circulating levels of dehydroepiandrosterone triggers this condition, causing polymorphic lesions over the seborrheic areas.1
The pathogenesis of acne vulgaris is multifactorial, involving the interaction of several host factors, such as the stimulation of sebaceous glands by circulating androgens, dysbiosis of the pilosebaceous follicle microbiome, and cellular immune responses.1
Inflammatory acne lesions can result in permanent disfiguring scars. Acne and its sequelae, such as post-inflammatory hyperpigmentation and scarring, are associated with substantial physical and psychological distress.2
Several acne scoring systems are available to grade acne, one of which is the global acne grading system (GAGS). This system divides the face, chest, and back into six areas (forehead, each cheek, nose, chin, and chest and back) and assigns a factor to each area based on size.3
Isotretinoin is an orally administered synthetic retinoid that was approved by the US Food and Drug Administration to treat severe, nodular, and resistant acne that is not responding to conventional therapy, including systemic antibiotics.4 The recommended dose is 0.5–1.0 mg/kg/day. As the side effects are dose-related, low-dose isotretinoin (0.25–0.5 mg/kg/day) therapy for acne is a good option.5 Cheilitis or dry lips are the most common adverse effects seen in patients taking isotretinoin. Dry skin, dry nose, dry mouth (xerostomia), dry eyes, and sun sensitivity are also very common adverse effects seen in patients taking isotretinoin.
Among the various treatment modalities available for treating acne one of the most performed procedures is chemical peels. Chemical peeling or chemoexfoliation causes controlled destruction of a part or entire epidermis with or without the dermis, followed by regeneration of new epidermal and dermal tissues.6
Keratolytic, anti-inflammatory properties of glycolic and salicylic acid (GA and SA) and bactericidal properties of SA make them the treatment of choice alone or as a part of combination therapy for all types of acne.7
Earlier isotretinoin was not combined with other modalities of treatment that involved destruction/remodeling of skin layers as it was thought to cause scarring, keloid formation, and delayed wound healing when used in high doses; however, recent studies show that low-dose isotretinoin (LDI) is safe and effective when combined with treatments such as chemical peels and lasers.8
There is a paucity of literature on the combination of isotretinoin and sequential chemical peels as a combination treatment; hence, we conducted this study to compare the safety and efficacy of oral isotretinoin and oral isotretinoin with the sequential chemical peel of 30% SA and 25% GA peel once every 2 weeks in acne vulgaris.
MATERIAL AND METHODS
The study was carried out between April 2023 and September 2023.
Sixty consecutive patients of either sex with moderate-to-severe acne were recruited for the study. GAGS was used as a tool to calculate the severity of acne. Patients were randomized using a random number table. Thirty patients were allocated to each group.
Inclusion criteria
The following criteria were included in the study:
Patients belonging to either sex in the age group of 15–45
Patients with moderate-to-severe acne who were not on any treatment previously.
Exclusion criteria
The following criteria were excluded from the study:
Patients below 15 years and above 45 years of age, patients with contraindications for isotretinoin use
Patients not willing to give consent
Pregnant and lactating patients
Patients with a keloidal tendency
Patients with endocrine abnormalities
Patients with very mild forms of acne were excluded from the study.
The Ethical Committee approved the study, and written consent was obtained from every patient. Patients were assigned into two Groups, A and B. Group A included patients receiving 0.25 mg/kg/wt isotretinoin as monotherapy, and Group B included patients receiving 0.25 mg/kg/wt isotretinoin once daily in combination with 30% SA peel (Salipeel DS, sesderma., Spain,) which was neutralized after 5 min followed by application of 25% GA (GA 25% sesderma., Spain) which was neutralized after 5 min. Sessions were carried out at 2-week interval for a total period of 12 weeks, that is, six sessions. All patients were put on isotretinoin (Capsule Acutret 10–20 mg), depending on body weight. All necessary laboratory investigations, such as complete blood count, liver function test (LFT), renal function test, lipid profile, urine routine, and microscopy, were carried out at baseline and at the final follow-up time to look for any drug-induced adverse effects. Lipid profile and LFT were carried out at monthly intervals. Patients were reviewed every 2 weeks and were instructed about the possible side effects and asked to report immediately if any occurred. Patient’s response to therapy and side effects were noted at each visit and they were instructed to avoid sun exposure using adequate sunscreen and other physical photo-protective measures. They were also instructed to use emollients in case of excessive dryness. Each type of lesion is given a value depending on severity: No lesions = 0, comedones = 1, papules = 2, pustules = 3, and nodules = 4. The score for each area (Local score) is calculated using the formula: Local score = Factor × Grade (0–4). The global score is the sum of local scores, and acne severity was graded using the global score. A score of 1–18 is considered mild; 19–30, moderate; 31–38, severe; and >39, very severe [Table 1]. A baseline 30% SA test patch and 25% GA test patch in the retro auricular region was carried out for all the patients in Group B, 2 days following which the patients were subjected to the 1st session of chemical peel. Each patient’s face was cleaned and degreased with acetone, and the sensitive areas (around the nostrils and mouth) were protected with petrolatum jelly. The peel was applied quickly with a Q-tip, exerting moderate pressure during the application, beginning with the forehead working from the center out, followed by each side of the face, and working from the cheek down. The peel was allowed to dry; the duration of contact was about 5 min for each peel. The peel was neutralized with a cotton swab dipped in normal saline, following which moisturizer and sunscreen composed of titanium dioxide, octyl methoxycinnamate, and diethylamino hydroxybenzoyl hexyl benzoate (Acne UV gel sunscreen SPF 50, IPCA) was applied to provide soothing, moisturizing as well as the photo-protective effect. The same moisturizer and sunscreen were used for all patients. Patients were advised to avoid direct sun exposure for 5 days following the procedure. GAGS was calculated every 2 weeks, and photographs were taken at every visit and the end of 12 weeks for comparison. Results were statistically analyzed using the Statistical Package for the Social Sciences 17 software IBM, Chicago.
| Location | Factor |
|---|---|
| Forehead | 2 |
| Right cheek | 2 |
| Left cheek | 2 |
| Nose | 1 |
| Forehead | 2 |
| Right cheek | 2 |
| Chest and upper back | 3 |
RESULTS
In our study, both treatment groups experienced significant improvement in acne severity as measured by the global acne grading (GAG) score [Table 2]. Intragroup analysis showed that the baseline profiles were comparable and the difference in GAG scores at the end of the treatment compared with the baseline is statistically significant. In addition, Group B showed better improvement in terms of pigmentation and scarring. Chemical peel treatment was well tolerated, with no major adverse events reported in Group B. Sixty patients of either sex between 15 and 45 years of age were included in this study. Group A had 17 males and 13 females. Group B had 14 males and 16 females. The average age was 24.5 in Group A and 23.8 in Group B. Among 60 patients, 29 were female and 31 were male. Treatment outcome has been measured in terms of improvement in GAG Score [Figure 1], pigmentation [Figure 2], scarring, and seborrhea [Table 2]. The mean GAG score at week 0 in Group A was 29.2 ± 5.03, and Group B was 26.7 ± 5.11. The mean GAG score at week 12 in Group A was 15.9 ± 5.09, and Group B was 9.23 ± 3.24, which showed statistically significant improvement in the acne severity in both Group A [Figures 3a and b, 4a and b]. Post-inflammatory pigmentation and erythema were graded as mild, moderate, and severe. The improvement was documented in terms of shift in the grade, that is, severe-to-moderate and moderate-to-mild. There was no significant improvement in scarring, yet Group B [Figures 5a and b, 6a and b] showed a better response. Patient satisfaction score (PSS) was high in Group B [Table 3]. Seborrhea improved equally in both groups. All the Group B patients tolerated the peel well with no major adverse events.
| Group A | Group B | |||||
|---|---|---|---|---|---|---|
| Mild (%) | Moderate (%) | Severe (%) | Mild (%) | Moderate (%) | Severe (%) | |
| GAG score | ||||||
| Pre-treatment | 0 | 16 (53.33) | 14 (46.66) | 0 | 23 (76.66) | 7 (23.33) |
| Post-treatment | 20 (66.66) | 9 (30) | 1 (3.33) | 30 (100) | 0 | 0 |
| P-value | <0.001 | <0.001 | ||||
| Pigmentation | ||||||
| Pre-treatment | 2 (6.66) | 10 (33.33) | 18 (60) | 5 (16.66) | 12 (40) | 13 (43.33) |
| Post-treatment | 12 (40) | 18 (60) | 0 | 22 (73.33) | 8 (26.66) | 0 |
| P-value | 0.009 | <0.001 | ||||
| Scar | ||||||
| Pre-treatment | 4 (13.33) | 12 (40) | 14 (46.66) | 9 (30) | 13 (43.33) | 8 (26.66) |
| Post-treatment | 9 (30) | 15 (50) | 6 (20) | 19 (63.33) | 11 (36.66) | 0 |
| P-value | 0.017 | <0.001 | ||||
GAG: Global acne grading
| PSS | Group A (%) | Group B (%) |
|---|---|---|
| 1. Highly unsatisfied | 0 | 0 |
| 2. Unsatisfied | 1 (3.33) | 0 |
| 3. Satisfied | 19 (63.3) | 11 (36.6) |
| 4. Highly satisfied | 10 (33.3) | 19 (63.33) |
PSS: Patient satisfaction score
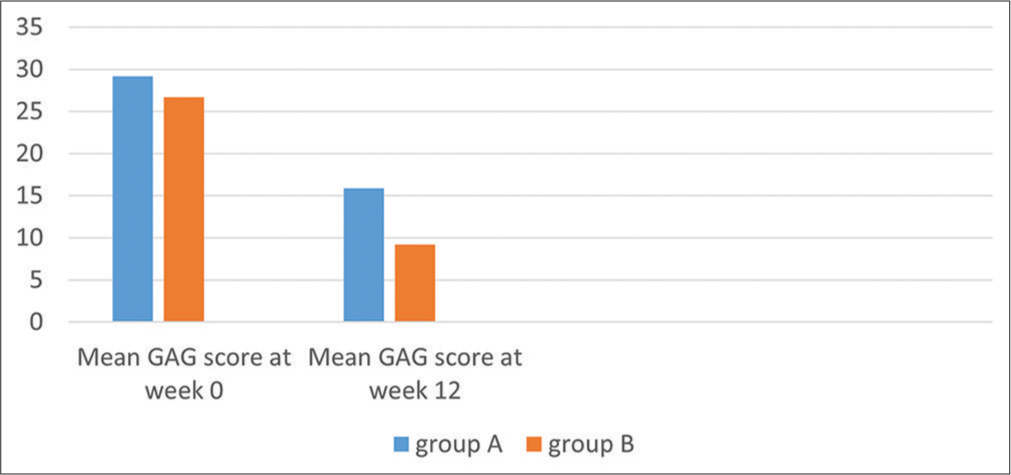
- Comparison of global acne grading score pre- and post-treatment. GAG: Global acne grading.
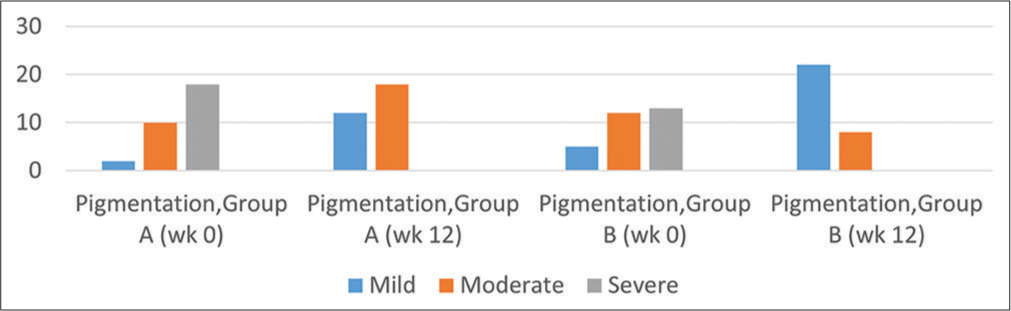
- Comparison of improvement in pigmentation in both groups.

- (a) Before and (b) after photographs of patient on isotretinoin monotherapy.

- (a) Before and (b) after photographs of patient on isotretinoin monotherapy.

- (a) Before and (b) after photographs of the patient on isotretinoin and sequential peel (30% salicylic acid followed by 25% glycolic acid).
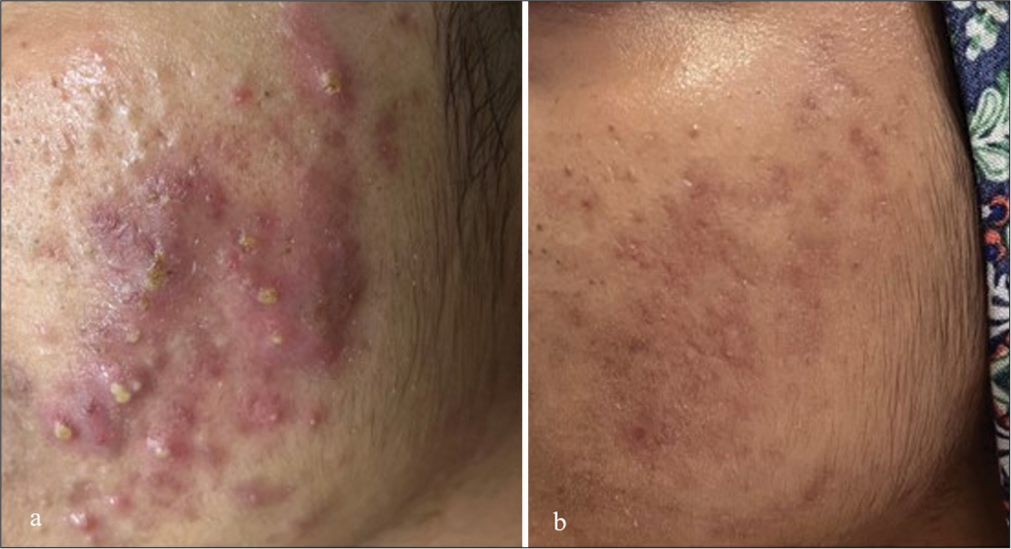
- (a) Before and (b) after photographs of the patient on isotretinoin and sequential peel (30% salicylic acid followed by 25% glycolic acid).
DISCUSSION
Isotretinoin at a dose of 0.5–1.0 mg/kg/day causes a significant reduction in sebum production; yet, the same effects can be achieved with a low dose, that is, 0.25–0.5 mg/kg/day, thus reducing comedogenesis. Among a wide armamentarium of chemical peels that are available, acids such as SA and GA are peeling agents of choice for treating acne. SA is a β hydroxy acid (2-hydroxy benzoic acid). It is a lipid-soluble agent that is miscible with epidermal lipids and sebaceous gland lipids in the hair follicle, attributing to comedolytic action, sebosuppressive. Being an organic acid, it extracts desmosomal proteins, including desmogleins, leading to loss of cohesion in epidermal cells, causing exfoliation; hence, it is regarded as a desmolytic agent rather than a keratolytic agent. About 20% and 30% of SA peels are used as superficial peels for acne.9
GA is an α hydroxy acid, which is a class of compounds derived from various foods. The depth of the peel in alpha hydroxy acid (AHA) is determined by the agent used, its concentration, volume applied, time of contact, frequency of application, integrity of stratum corneum, and skin thickness. At low concentrations, they cause a decrease in corneocyte adhesion, and at higher concentrations causes epidermolysis and upper dermal changes, giving vibrantly uniform colored skin.10
Our results are comparable to a study conducted by Kar et al.8 wherein they compared results of oral isotretinoin versus oral isotretinoin + 20% SA peel in the treatment of active acne using Michelson acne severity index score; however, in our study, we used GAG score and performed sequential peels of 30% SA followed by 25% GA peel.
In another study conducted by Zayed et al.,11 they compared results of sequential application of 70% GA, followed by 20% SA in Group A, sequential peel and oral doxycycline 100 mg PO BD (per oral [PO] bis in die (Twice Daily) [BD])for 1 month followed by 100 once daily (OD) for 2 months in Group B and only oral doxycycline 100 PO BD in Group C, and PSS in Groups A and B was higher compared to Group C likewise in our study PSS was high in Group B.
Successful management of acne involves a multifaceted approach, choosing multiple treatment modalities simultaneously or sequentially to attain quick response and maintain long periods of remission. The previous studies showed that combination peels with LDI showed a better and faster response when compared to single peel; however, there is a paucity of literature on the combination of LDI and sequential peels.
The advantage of sequential chemical peeling is that the first peeling agent enhances the penetration of the second, thus increasing the depth of the peel without increasing the concentration of the peeling agents.
In our study, we combined SA (lipophilic) followed by GA, which further enhanced the penetration of the latter, thus showing better results with negligible side effects. According to standard guidelines, procedures are contraindicated in patients on isotretinoin, yet many studies have shown many favorable results when combined with superficial chemical peels.
In our study, we considered LDI, which had a better side effect profile and better tolerability, thus making patients more compliant with the treatment. There was a significant improvement in both groups, although Group B showed faster response and better improvement in pigmentation and, to some extent, scarring.
Post-treatment follow-up up to 6 months showed less relapse rate in Group B, requiring no or minimal treatment. The PSS in Group B was high, and they were willing to maintenance a session of chemical peels.
CONCLUSION
Superficial chemical peels (single or combination sequential peels) are safe and effective in patients with LDI. LDI can also stand as a monotherapy in patients not willing for any procedures as it gives a good balance between efficacy and dose-related side effects. In our study, patients were more compliant in Group B as there were no significant complications, and there appeared to be a better and quicker response. More trials and studies are necessary to ascertain that better results in patients taking isotretinoin with combination sequential peels may be achieved, and if this is successfully demonstrated, administration of isotretinoin in combination with lasers and energy-based devices must be explored in the future.
Authors’ contributions
Kolluri Siva Bala Vaishnavi: Concept, design, data acquisition ,drafting article, statistical analysis, manuscript writing,editing and review, final approval for publication, Guarantor. Chelikani Vijaya Lakshmi: Concept, design, data acquisition, drafting article, statistical analysis, manuscript editing and review, final approval for publication, Guarantor. Chandrapola Vivek: Concept, design, data acquisition, drafting article, statistical analysis, manuscript writing and review. Sompalli Suryanarayana: Concept, design, data acquisition, drafting article, statistical analysis, manuscript writing and review. Meeripelli Kavya: Concept, design, data acquisition, drafting article, statistical analysis, manuscript writing and review. Parasuramapuram Spandana: Concept, design, data acquisition, drafting article, statistical analysis, manuscript writing and review.
Ethical approval
The research/study approved by the Institutional Review Board at Mallareddy Institute of Medical Sciences, number MRIMS/DHR-IEC-FAC/2023/10-B, dated March 13, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Acne vulgaris In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459173 [Last accessed on 2024 Apr 27]
- [Google Scholar]
- Acne scars: Pathogenesis, classification and treatment. Dermatol Res Pract. 2010;2010:893080.
- [CrossRef] [PubMed] [Google Scholar]
- Scoring systems in acne vulgaris. Indian J Dermatol Venereol Leprol. 2009;75:323-6.
- [CrossRef] [PubMed] [Google Scholar]
- Isotretinoin In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525949 [Last accessed on 2024 Apr 27]
- [Google Scholar]
- Safety and efficacy of low-dose isotretinoin in the treatment of moderate to severe acne vulgaris. Indian J Dermatol. 2014;59:316.
- [CrossRef] [PubMed] [Google Scholar]
- Chemical peels In: Alam M, Tung R, Gladstone H, eds. Cosmetic dermatology. United States: Saunders, Elsevier; 2009.
- [CrossRef] [Google Scholar]
- Chemical peels in the treatment of acne: Patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:365-72.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study of oral isotretinoin versus oral isotretinoin + 20% salicylic Acid peel in the treatment of active acne. J Cutan Aesthet Surg. 2013;6:204-8.
- [CrossRef] [PubMed] [Google Scholar]
- Salicylic acid as a peeling agent: A comprehensive review. Clin Cosmet Investig Dermatol. 2015;8:455-61.
- [CrossRef] [PubMed] [Google Scholar]
- Safety of performing superficial chemical peels in patients on oral isotretinoin for acne and acne-induced pigmentation. J Clin Aesthet Dermatol. 2021;14:41-3.
- [Google Scholar]
- Sequential peeling as a monotherapy for treatment of milder forms of acne vulgaris. J Cosmet Dermatol. 2019;19:1381-7.
- [CrossRef] [PubMed] [Google Scholar]






