Translate this page into:
A Curious Case of Paroxysmal Painful Thumb: Glomus Tumor Re-visited
Address for correspondence: Dr Vikas Pathania, Classified Specialist (Dermatology), Command Hospital (SC), Pune, Maharashtra 411040, India. E-mail: vikascongo@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Glomus tumor is a rare and benign vascular hamartoma originating from the neuro-myo-arterial apparatus of the glomus body in the reticular dermis. Most commonly, it presents as a solitary subungual lesion which is often painful and triggered by changes in temperature and pressure on the affected digit. However, multiple glomus tumors both digitally and elsewhere on the body which may or may not be painful are also known to occur. Due to its cryptic location and varied presentation, there is an invariable delay in the diagnosis and management of this condition. We report a case of glomus tumor in a 28-year-old woman presenting with paroxysmal painful lesion over her right thumb for 5 years.
Keywords
Glomus body
ildreth’s sign
Love’s sign
magnetic resonance imaging
INTRODUCTION
Glomus tumor is a rare vascular hamartoma and constitutes 1–5% of soft tissue tumors of the hand. It is commonly seen in women 20–40 years of age. It usually presents as a solitary digital lesion most often subungual in location with the classical triad of symptoms: spontaneous lancinating pain, extreme pain with gentlest touch, and intolerance to changes in temperature.[1] Diagnosis is often delayed by prolonged referral to various specialities before a definitive diagnosis is made. While diagnosis is essentially clinical, radiological modalities are often helpful in delineating the extent and differentiating between other soft tissue tumors. Surgical excision is the treatment of choice.[2] We report a case of 28-year-old woman who was symptomatic for 5 years before being finally diagnosed and managed as a case of glomus tumor.
CASE HISTORY
A 28-year-old housewife was referred to the Dermatology Outpatient Department after being symptomatic with spontaneous paroxysmal as well as induced pain to cold water in her right thumb for past 5 years. She had been evaluated in surgery, orthopedics, and even rheumatology outpatient department before being finally sent to us for opinion. The pain had particularly worsened over the past 6 months to the extent that she was unable carry out her daily chores involving water. She did not give any history of preceding trauma to the digit. On examination, there was localized tenderness measuring around 2 × 2 mm on the right thumb placed 1 cm proximal to the junction of the proximal and lateral nail fold [Figure 1]. Love’s sign and Hilldreth’s sign were positive. Radiography of the digit was unremarkable. However, magnetic resonance imaging (MRI) revealed a nodular hyper vascular lesion subungually consistent with a glomus tumor [Figure 2].
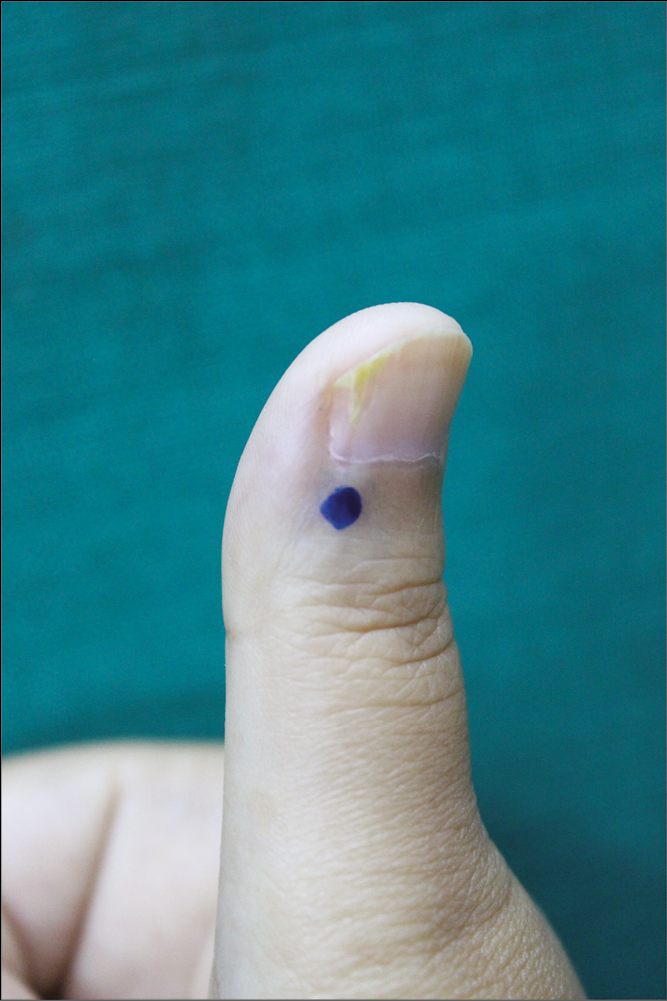
- Localized tender spot on right thumb located inferolateral in relation to the nail (Love’s sign)
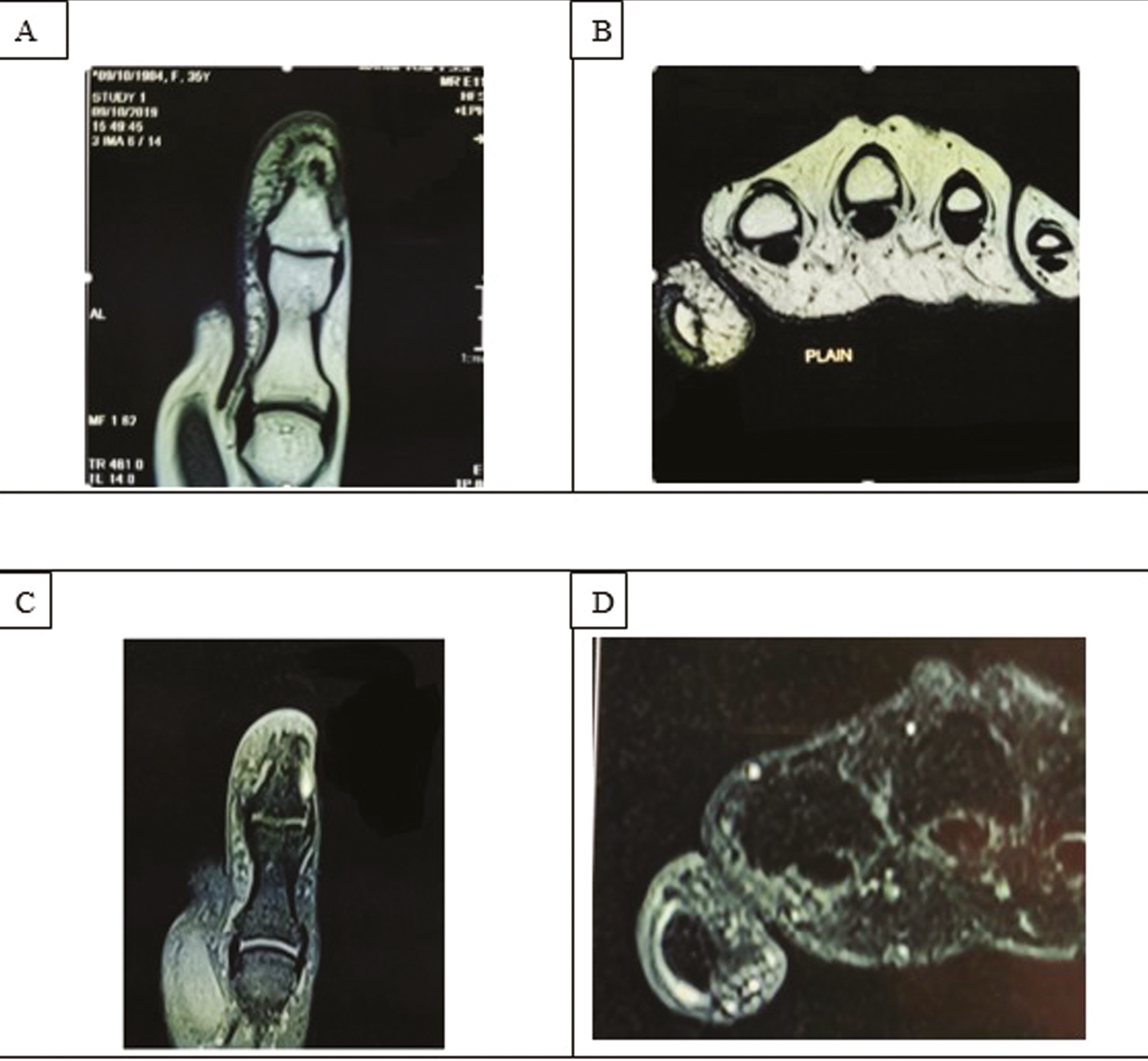
- MRI of the right thumb. A. T1 coronal for thumb. B. T1 axial. C. Post-contrast T1 fat saturated coronal image of the thumb. D. Post-contrast T1 fat saturated axial image of the thumb. MRI showed a focal soft tissue nodular thickening at subungual aspect of the thumb. On T1, the lesion was isointense to muscle. On post contrast, this lesion showed avid enhancement. Underlying bone was normal. Findings were suggestive of a benign hypervascular lesion
A surgical excision of the tumor was performed under local anesthesia. After administering a proximal digital block using 2% lignocaine hydrochloride with epinephrine (1:2,00,000) and digital exsanguination, a tourniquet was applied for avascular surgical field. An oblique incision on either side of the proximal nail fold was made for mobilizing the same. Then, the lateral part of the nail plate was lifted from the nail bed. Both the lateral half of the nail plate and the proximal nail fold were reflected up by extending the incision proximally till direct visualization of the tumor in the right lateral nail-matrix region [Figure 3A]. The tumor was dissected with a minimal margin to avoid excessive trauma to the matrix and submitted for histopathological confirmation [Figure 3B]. The nail plate was replaced back and secured to the lateral nail fold, and the proximal nail fold sutured with 4-0 interrupted proline sutures [Figure 3C]. The wound was dressed and sutures were removed on the 8th day. The post-operative period was uneventful and the patient was symptom-free on follow-up at 3 months [Figure 3D]. Histopathology was consistent with glomus tumor [Figure 4].

- A. Trans-ungual approach to the tumor (black arrow) with exposure of nail bed and matrix after reflecting the nail plate and proximal nail fold. B. Excised tumor tissue. C. The nail plate and proximal nail fold re-positioned with the help of 4-0 non-absorbable sutures. D. Asymptomatic with well healed scar 3 months post-operatively
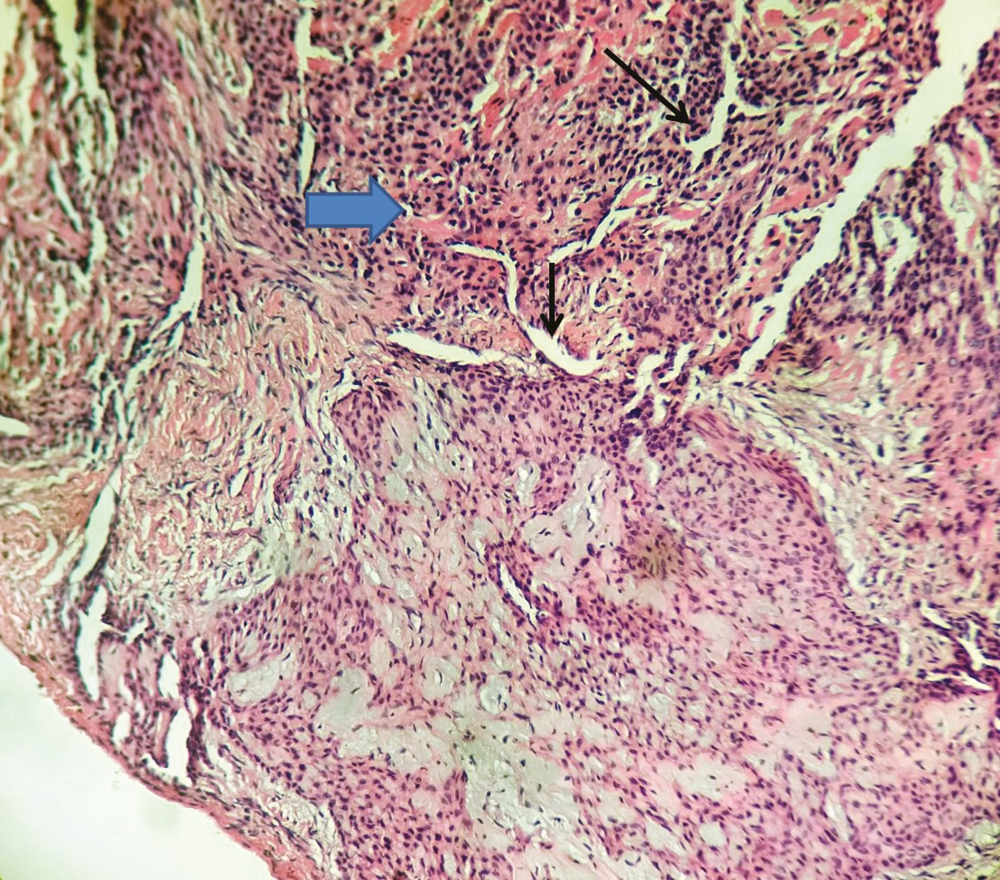
- Photomicrograph of the excised lesion showing varying sized vessels (black arrows) surrounded by collarettes of glomus cells (blue arrow) (H&E, ×10)
DISCUSSION
Glomus tumor was first described by Wood in 1812 and named by Masson in 1924.[2] A glomus body consists of three main structures: the glomus cells, the vasculature, and smooth muscles. It functions as a neuro-myo-arterial receptor which regulates blood flow in response to changes in temperature and pressure. Hypertrophy of any of these structures can result in a glomus tumor.[1] While they are distributed ubiquitously in the dermis, 75% of these are present in hands and 65% of these are situated subungually.[3] This explains their commonest presentation as solitary painful subungual tumors. Other uncommon presentations include multiple glomus tumors, painless tumors, familial cases with autosomal dominant inheritance, and those associated with neurofibromatosis.[34] Though underlying etiology is not entirely understood, it is proposed that they may arise because of reactive hypertrophy of individual components following trauma. The sensitivity of the tumor to changes in temperature can be explained by the contraction of myofilaments resulting in increased intracapsular pressure, transmitted by unmyelinated nerves responsible for pain sensations.[2] However, our patient did not give any such history of preceding trauma.
The diagnosis of glomus tumor can usually be made clinically. In this regard, two signs are helpful: the Love’s sign which is eliciting localized tenderness by applying pressure with a pinhead and the Hildreth’s test in which the patient’s arm is elevated to exsanguinate it followed by a tourniquet application with a sphygmomanometer inflated to 250 mmHg, which significantly ameliorates the pain and tenderness elicited by the Love’s test.[25] Both the signs were positive in our patient. Radiological modalities can prove valuable adjuncts in diagnosis. Plain digital radiographs may reveal bone erosion in up to 30% of the cases. Ultrasonography may help localize and assess size of the tumor preoperatively, whereas Doppler sonography may further help in identifying low signals within hypoechoic masses. MRI is the most useful non-invasive preoperative modality in diagnosing glomus tumors with a sensitivity of 90%, specificity of 50%, positive predictive value of 97%, and negative predictive value of 20%. Most glomus tumors are seen as a dark lesion on T1-weighted image and as a bright signal intense lesion on T2-weighted images.[5] In our patient, plain radiograph did not reveal any bony lesion, whereas MRI located a nodular hypervascular lesion in the lateral subungual region of the right thumb.
Management of glomus tumor is essentially surgical. Two principal approaches have been described in the literature: the transungual approach for centrally placed subungual tumors and a periungual (lateral) approach. While the transungual approach is the more popular method by affording better visualization of the tumor in the nail bed and lower risk of recurrence, the periungual approach has the advantage of lower risk of nail deformity.[6] A subungual approach has also been described for aesthetically superior results, whereby the entire nail bed is raised as a flap and repositioned after excision of the tumor.[7] In case of tumors of the nail matrix as in our case, an eponychial flap should be raised for better visualization.[2] Histopathology can have variable composition of glomus cells, blood vessels, and smooth vessels. Accordingly, they can be categorized into three types: glomangioma with abundance of vessels, solid glomus tumors with predominantly glomus cells, and glomangimyomas constituted chiefly by smooth vessels.[4] In our patient, histopathological examination of the excised tumor revealed a well-circumscribed mass composed of branching capillary sized vessels lined by endothelial cells and surrounded by collars of uniform glomus cells forming nests, sheets, and trabeculae in a myxoid stroma.
We reported this case to highlight the fact that despite its characteristic presentation, there is invariably a delay in management of this painful condition in most instances due to the diagnostic challenges owing out of its rarity and subungual location as well as the adjunctive role of imaging in its diagnosis and management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Transungual surgical excision of subungual glomus tumour. J Cutan Aesthet Surg. 2013;6:196-203.
- [Google Scholar]
- Multiple glomus tumours in multidigit nail bed. Handchir Mikrochir Plast Chir. 2017;49:321-5.
- [Google Scholar]
- Magnetic resonance imaging in the diagnosis of glomus tumours of the hand. J Hand Surg Br. 2005;30:535-40.
- [Google Scholar]
- Transungual resection of subungual glomus tumour. BMJ Case Rep. 2017;2017:bcr2017221211.
- [Google Scholar]
- Excision of subungual glomus tumor by subungual approach: A useful yet underutilized technique. J Cutan Aesthet Surg. 2019;12:187-90.
- [Google Scholar]






