Translate this page into:
A Dermoscopic Study of Cutaneous Warts and Its Utility in Monitoring Real-Time Wart Destruction by Radiofrequency Ablation
Address for correspondence: Dr. Niti Khunger, Department of Dermatology & STD, Vardhaman Mahavir Medical College, Safdarjang Hospital, New Delhi, India. E-mail: drniti@rediffmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Context:
Cutaneous warts can affect up to 7–12% of the general population. Usually diagnosed clinically, there may be diagnostic dilemmas in atypical presentations or immunocompromised patients. Radiofrequency ablation is a common method of treatment of warts, but recurrences occur due to incomplete removal. Dermoscopy has been used in the diagnosis of various infectious dermatoses including warts.
Aims:
The study aimed to assess dermoscopic features of various types of viral warts and its efficacy in monitoring the treatment response following radiofrequency ablation.
Settings and Design:
Prospective non-comparative descriptive study in a tertiary care centre.
Subjects and Methods:
A prospective study was conducted comprising 60 patients with clinically diagnosed, previously untreated warts, including common warts, plane warts, palmar and plantar warts. Dermoscopic features of a representative lesion were evaluated in terms of definition, background color, vascularity, surrounding halo, dermatoglyphics, and presence of hemorrhage or crust. It was done at baseline and immediately after radiofrequency ablation of the wart to observe for complete removal of wart.
Results:
Most common dermoscopic features observed were presence of papillae surrounding haloes (61.67%), vascularity (dots>globules>linear vessels>loops; 58.33%), interrupted skin lines (51.67%), and brown colored background (48.3%). Nine cases (15%) demonstrated incomplete removal of the wart that was not visible with the naked eye and picked up only on dermoscopy. On follow up, at 6 months there were four recurrences (6.67%).
Conclusion:
Dermoscopy shows consistent features in the examination of warts. This can be a quick clinical aid in distinguishing it from close differentials. It is also valuable in reviewing the lesion real time after any ablative procedure to check if it has been removed in its entirety.
Keywords
Dermoscopy
destruction
HPV
radiofrequency ablation
recurrence
viral warts
INTRODUCTION
Cutaneous warts caused by Human papilloma virus can affect up to 7–12% of the general population.[1] They are benign proliferations of the epidermis and may present in different forms, frequently seen as common warts, plane warts, palmar/plantar warts, or anogenital warts (condyloma acuminata). Majority of the times they can be diagnosed clinically, however, in certain situations uncertainty can arise. The presence of thrombosed capillaries is a characteristic feature; however, these are absent in plane warts. Common warts can mimic many conditions. Plantar warts may be similar to corns and callosities. Large hyperkeratotic warts may be difficult to distinguish from squamous cell carcinoma.[2] This diagnostic confusion can be further compounded in immune-compromised patients who have atypical presentations of warts. In the absence of a definite diagnosis, there may be difficulty in choosing the optimum management.
There has been an exponential rise in the use of dermoscopy to aid in the diagnosis of various dermatological disorders in the last decade. It is increasingly being employed to support the diagnosis of various infectious dermatoses including viral warts. There is a paucity of studies of dermoscopic features of warts in darker skin types IV–V. Among the available medical and destructive therapeutic options for cutaneous warts, none is uniformly effective or virucidal. Recurrent or difficult-to-treat lesions are often treated with alternative therapies like physical destruction that have drawbacks like high rates of recurrence or adverse effects.[3]
In this study, we describe dermoscopic features of warts and its significance in monitoring treatment.
SUBJECTS AND METHODS
This was a prospective study of 60 patients with all types of clinically diagnosed warts, irrespective of age and gender, who reported in a period of 1 month. Patients with anogenital warts and those who gave history of taking prior treatments were excluded. An informed consent was taken. Clinical examination was done and dermoscopic evaluation was performed using Dermlite II HR dermoscope (polarized mode, without interface) and photographs were captured by Apple Iphone 7. Clinical features examined were site, number, arrangement, and morphology of the warts. One representative lesion was then selected and examined dermoscopically. Polyvinyl chloride food wrap (plastic wrap) was applied on the lesions before placing the dermoscope to prevent cross infections. The variables included in the dermoscopic evaluation were definition of the wart (well defined/ill defined), background color (red/pink/yellow/brown/other), presence of vascular component, type of vascular component if present (dots/globules/linear/loops/others), papillae/surrounding halo, skin lines (interrupted/continuous/not visible), presence of hemorrhage or crust or any other new observation.
Standard method of radiofrequency ablation was carried out for the warts under local anesthesia. The lesion was re-examined dermoscopically immediately after cessation of hemorrhage to look for any remnant of the wart. End point was a homogenous pink background, with absence of red or black dots, brown pigment or haloes, which indicated complete clearance. Remnants were seen as presence of vascular structures such as red or black dots or globules, brown pigmentation or papillae.
RESULTS
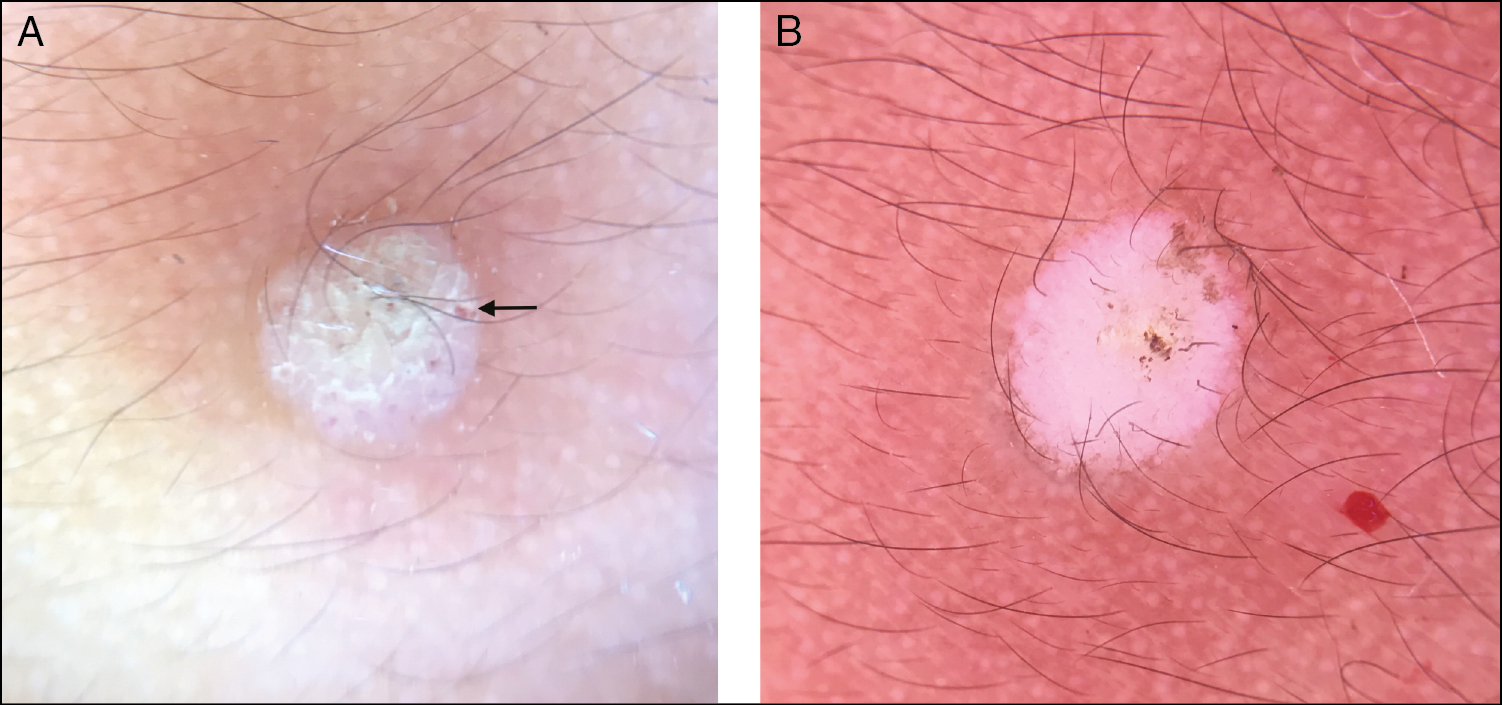
Sixty patients with extragenital warts were evaluated clinically and dermoscopically. The clinical details of the warts are given in Table 1. Dermoscopic examination showed that the warts were well defined in most of the cases (n = 50; 85%) [Box 1]. The most common background color was brown (n = 29; 48.3%), followed by yellow (n = 16; 26.67%) and pink (n = 15; 25%). Vascularity was appreciated in 35 lesions (58.33%). The vascularity comprised dotted vessels in 23 (38.33%) lesions, globules in 10 (16.67%), linear vessels in 7 (11.67%), and loops in 2 (3.33%) lesions. Skin colored papillae/haloes were also visible in majority of lesions (n = 37; 61.67%). Skin markings surrounding the lesions were interrupted in 31 (51.67%) cases and not visible in the remaining (n = 25; 41.67%). None of the lesions showed continuous skin markings. Six (10%) lesions showed presence of hemorrhage and no lesions showed crusting dermoscopically [Figures 1–4]. Table 2 depicts specific dermoscopic findings in relation to the morphology of the warts.3
| Morphological types of warts | Number of patients (%) |
|---|---|
| Common warts/verruca vulgaris | 30 (50) |
| Plane warts/verruca plana | 10 (16.67) |
| Palmo-plantar warts | 20 (33.33) |
| Total | 60 (100) |
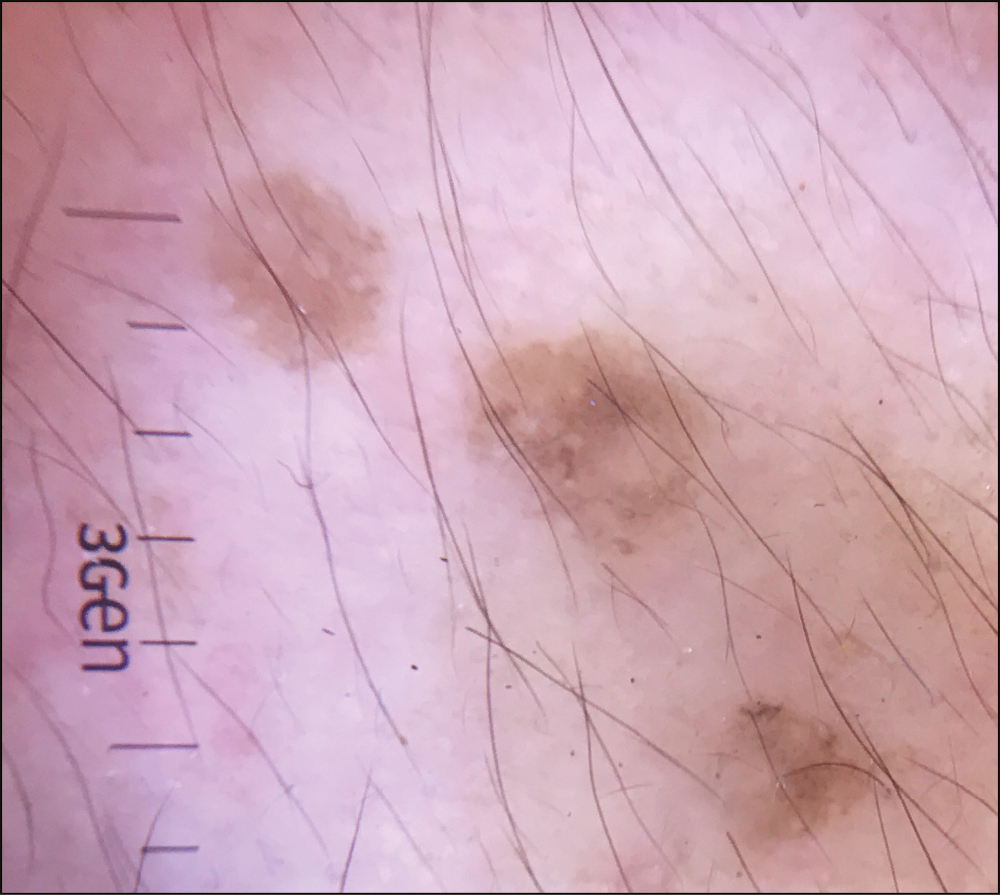
- Dermoscopy of verruca plana showing ill defined margins, even brown background and absence of vascularity
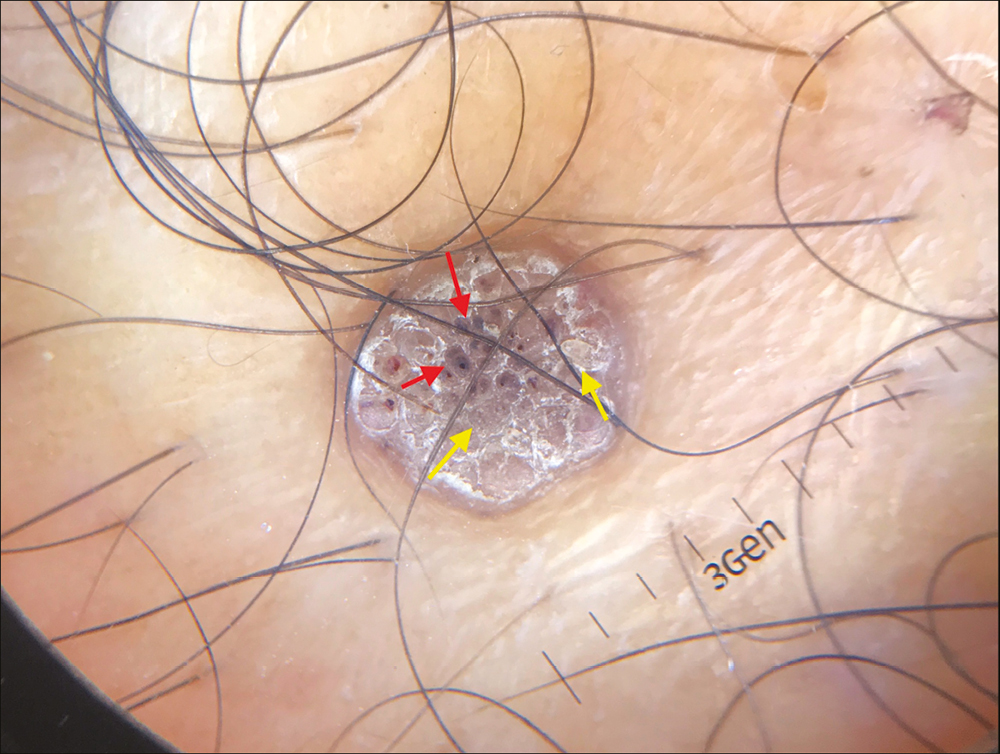
- Dermoscopy of verruca vulgaris showing well-defined margins, brown background, skin colored papillae (yellow arrows) with red dots and globules (red arrows) and hemorrhage

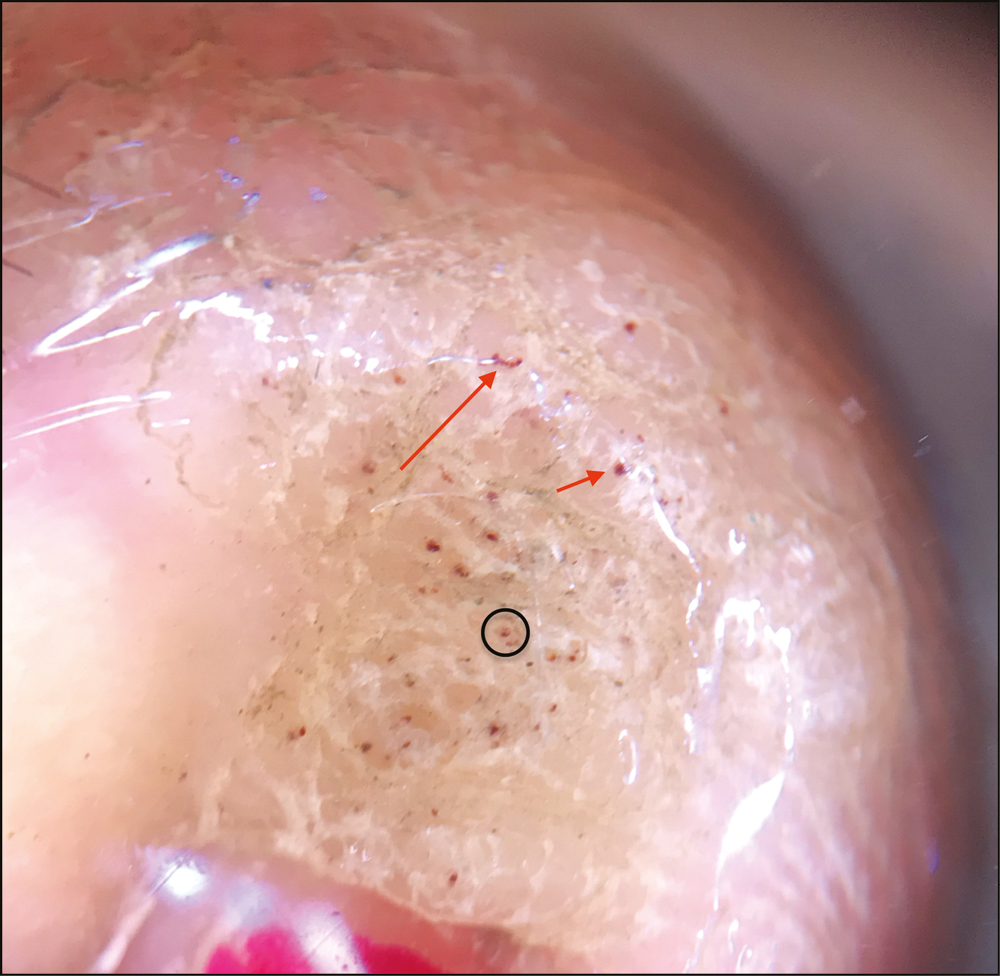
- Dermoscopy of palmar wart showing well defined margins brown background, papillae and haloes (yellow arrows), with red dots and globules (red arrows), interrupted skin lines
- Dermoscopy of plantar wart showing ill defined margins, yellow background, few papillae/haloes with red dots (black circles), red dots (short red arrow) and linear vessels (long red arrow)
| Type of wart | Common warts (n = 30) | Plane warts (n = 10) | Palmoplantar warts (n = 20) |
|---|---|---|---|
| Dermoscopic features | |||
| Well defined, n (%) | 27 (90%) | 4 (40) | 19 (95) |
| Background color, n (%) | Pink: 10 (33.33) | Pink: 0 (0) | Pink: 5 (25) |
| Yellow: 7 (23.33) | Yellow: 0 (0) | Yellow: 9 (45) | |
| Brown: 13 (43.33) | Brown: 10 (100) | Brown: 6 (30) | |
| Presence of Papillae/surrounding haloes, n (%) | 21 (70) | 5 (50) | 11 (55) |
| Presence of vascularity, n (%) | Dots: 10 (33.33) | Dots: 1 (10) | Dots: 12 (60%) |
| Globules: 5 (16.67) | Globules: 0 (0) | Globules: 5 (25) | |
| Linear: 4 (13.33) | Linear: 0 (0) | Linear: 3 (15) | |
| Loop: 2 (6.67) | Loop: 0 (0) | Loop: 0 (0) | |
| Skin markings, n (%) | 9 (30) | 2 (20) | 20 (100) |
| Presence of Hemorrhage/crusting, n (%) | 4 (13.33) | 0 (0) | 2 (10) |
| Presence of papillae/ surrounding haloes |
| Evidence of vascularity (dots>globules>linear vessels>loops) |
| Interrupted skin lines |
| Brown colored background |
Dermoscopic examination of the selected lesion after radiofrequency ablation showed that 9 (15%) lesions retained few of the baseline dermoscopic characteristics suggesting incomplete removal which was not visible with the unaided eye [Figures 5–7]. On follow up, out of 60 patients, 20 patients returned after 3 and 6 months, out of which four showed features of recurrence at the same site. The rest of the 40 patients were contacted telephonically, out of which 35 denied recurrence and 5 could not be contacted [Figure 8].
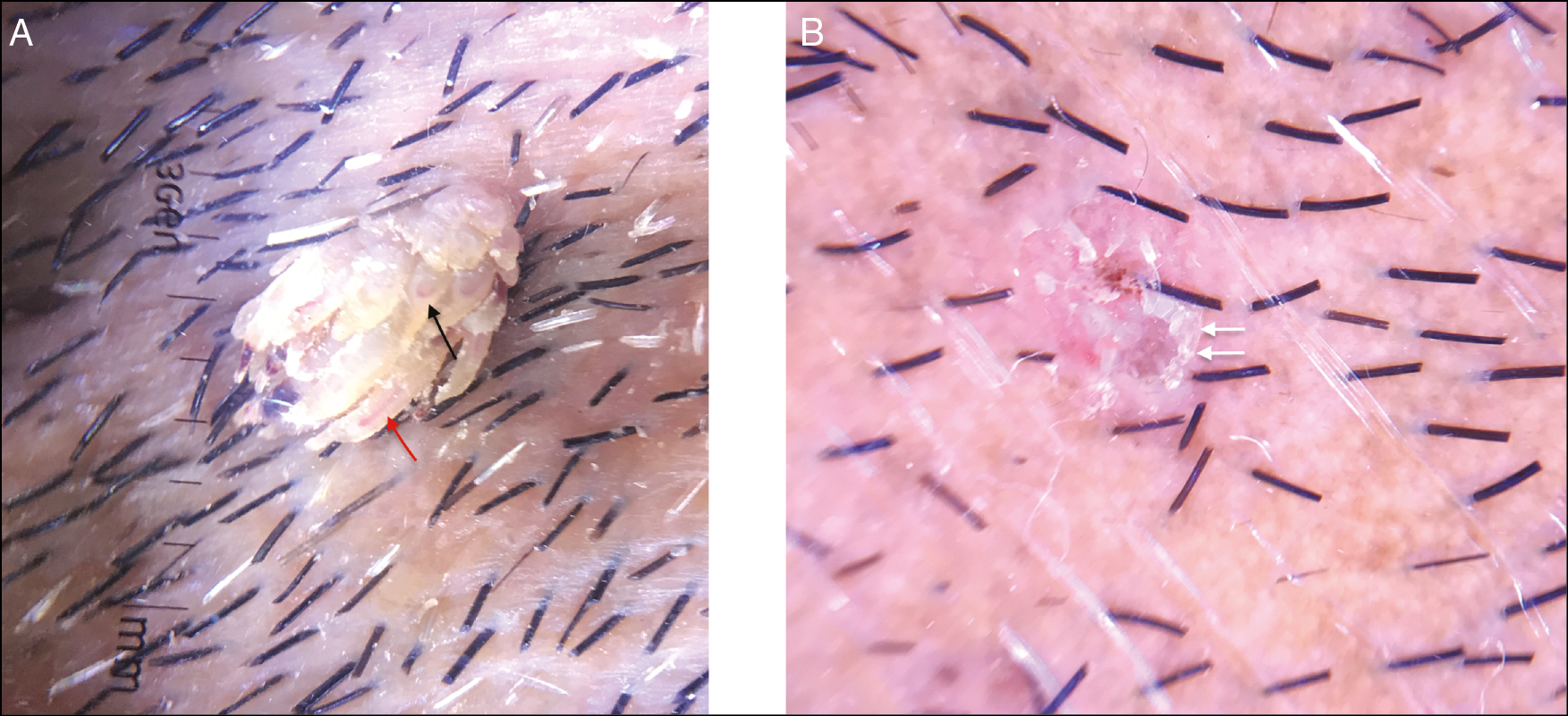
- (A) Dermoscopy of filiform wart (pre RFA) showing yellow papillae with linear (red arrow) and looped (black arrow) vessels. (B) Dermoscopy of filiform wart (post RFA) showing few yellow papillae (white arrows) remaining indicating incomplete wart removal (note the artefactual shiny lines due to plastic wrap application)
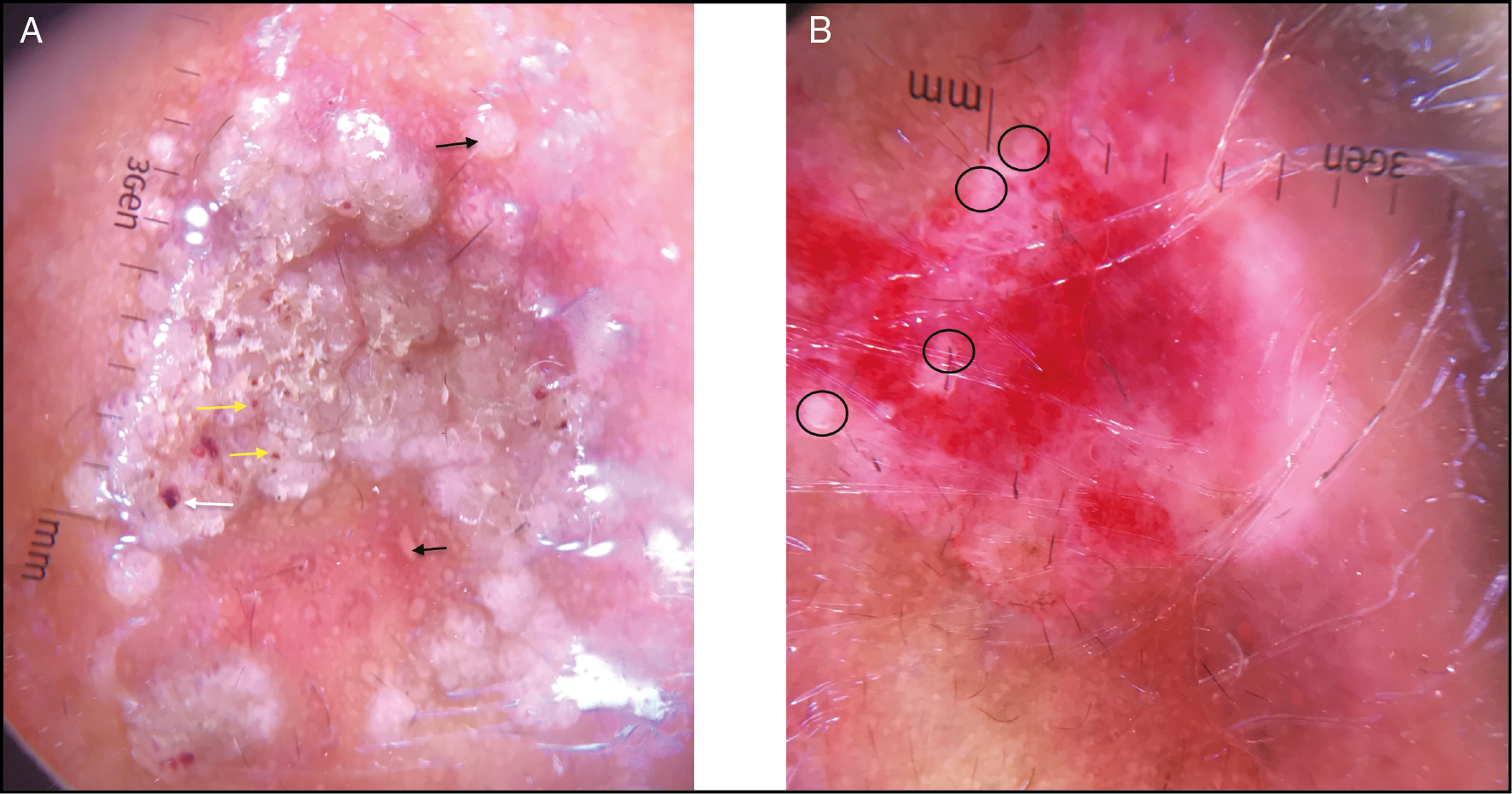
- (A) Dermoscopy of common wart (pre RFA) showing pink background, papillae (black arrows) with dots & globules (yellow arrows) and hemorrhages (white arrow). (B) Dermoscopy of common wart (post RFA) showing few papillae remaining at periphery (black circles) indicating incomplete wart removal
- (A) Dermoscopy of common wart (pre RFA) showing yellow background, papillae and dots (black arrow). (B) Dermoscopy of common wart (post RFA) showing no papillae or dots indicating complete wart removal
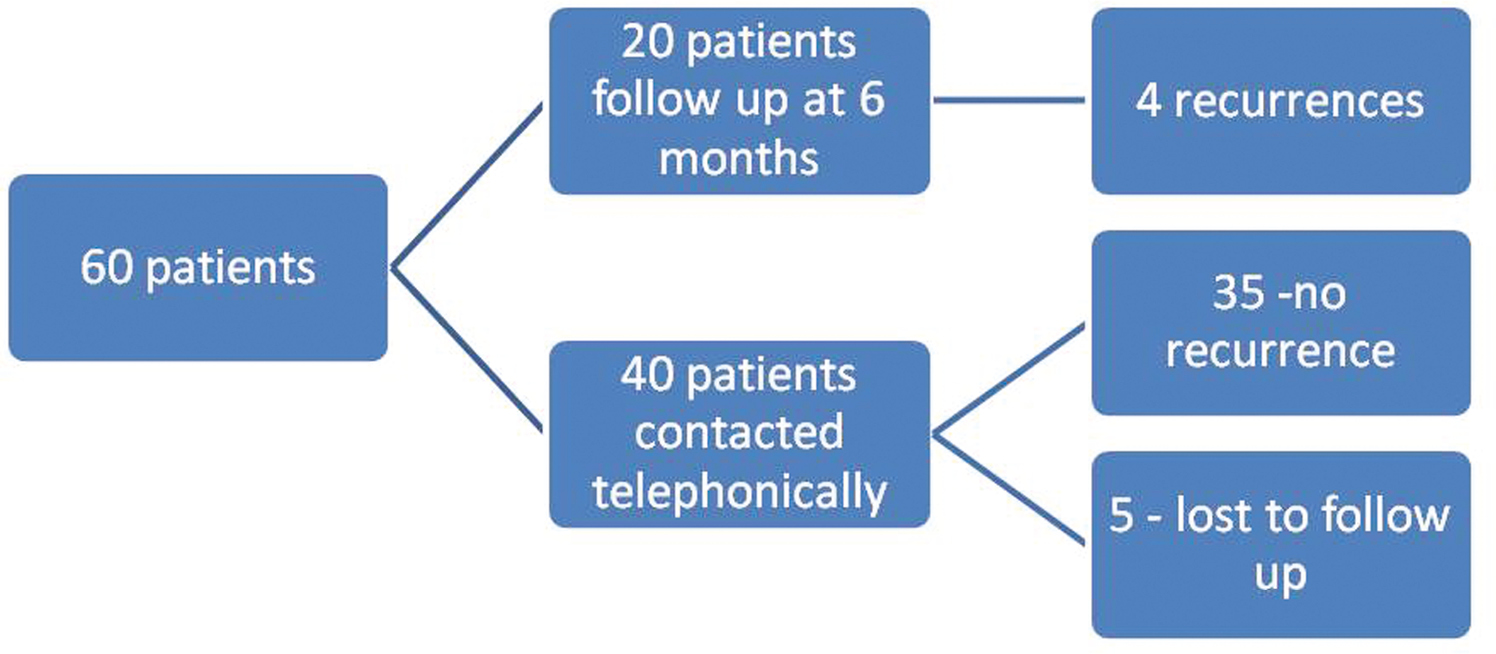
- Follow up of patients
DISCUSSION
Warts are primarily a clinical diagnosis, although a few cases may resemble other dermatological disorders. Facial warts may be confused with syringoma, molluscum, or lichen nitidus. Common warts may mimic a variety of disorders like hypertrophic actinic keratosis, basal cell carcinomas, benign appendageal tumors, or congenital epidermal nevi. Plane warts often resemble seborrhoeic keratosis, melanocytic lesions, or lichen planus papules.[2] In doubtful cases, especially when histopathological examination is refused by the patient or cannot be conducted, dermoscopy can guide as an auxillary tool for the confirmation of diagnosis. Dermoscopy of warts in darker skin types has been described in few studies so far. Dermoscopic features of verruca plana include even colored light brown to yellow patches with dots or globular vessels and regularly distributed red dots on a brown or yellow background.[45] Dermoscopic features of plantar warts include presence of homogenous black/red dots and globules with papilliform surfaces and interrupted skin lines and rarely parallel ridge pattern.[67] Bae et al.[7] dermoscopically differentiated corns and callosities from plantar warts and reported that the former have translucent central core and homogenous opacities. Tanioka et al. and Arpaia et al. also reported parallel ridge pattern in acral warts.[89] Lallas et al.[10] described dermoscopic features of common warts as densely packed papillae with central red dot/loop surrounded by whitish haloes.
The most common dermoscopic features of warts in our study have been outlined in Table 2. In the current study, the most common background color was found to be varying shades of brown probably reflecting the study population which consisted of darker skin types IV–V population. The main dermoscopic features of warts are the presence of a vascular component reflecting the dilated and thrombosed vessels within the papillary dermis. However, in our study vascularity was observed only in 35 (58.33%) cases. A reason for this could be the pigmented nature of lesions obscuring fine vascularity in skin of color population and the use of a handheld dermoscope offering lesser magnification. We also observed that in order to prevent cross infections, the pressure from the use of a plastic cling film wrap or contact dermoscope easily led to blanching of vascularity especially in smaller warts. Hence a certain amount of expertise is required to gently place the dermoscope on the lesion. Perhaps videodermoscopes and non-contact dermoscopes which also can offer higher magnifications may be more sensitive in picking up vascular structures. The most common finding in our study was the presence of papillae and haloes. Interrupted skin markings as observed in our study can also signify viral warts dermoscopically as in the majority of our cases. We did not report any case showing parallel ridge pattern as suggested in previous studies.
Another very important aspect that our study uncovered was the use of dermoscopy to check for the complete clearance of the wart after radiofrequency ablation. There were a significant number of lesions (n = 9; 15%) showing remnant features of warts after removal which were not visible to the naked eye. This advantage can possibly be extrapolated to all forms of ablative treatments to judge the adequate depth and size of ablation, thus prevent or reduce the incidence of recurrences as well as scarring. In non-ablative treatments, dermoscopy may assist in deciding the end point of treatment. Wide variation in terms of recurrence rates has been reported with different treatment modalities used for warts. Recurrence rates ranging from 10 to 30% have been reported with various destructive treatment modalities for warts.[111213] Our study had a recurrence rate of 6.67%. This may be due to the fact that in patients with multiple warts, all the warts were not assessed by the dermoscope. Dermoscopy can also be used to monitor response in other forms of treatment as well. The limitation of our study was inadequate follow up of lesions.
CONCLUSION
In conclusion, dermoscopy shows consistent features in the examination of warts such as vascular structures, black dots, papillae, and haloes on a background of brown pigmentation. The pigmentation may obscure red dots in darker skins. It can be a quick clinical aid in distinguishing it from close clinical differentials. It also has value in monitoring the lesion real time after any ablative procedure to check if it has been removed in its entirety and deciding the end point. This will help in reducing recurrences and repeated procedures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Immunotherapy for recalcitrant warts in children using intralesional mumps or candida antigens. Pediatr Dermatol. 2003;20:268-71.
- [Google Scholar]
- Treatment of cutaneous warts: an evidence-based review. Am J Clin Dermatol. 2012;13(Suppl 2):73-96.
- [Google Scholar]
- Clinical clues for differential diagnosis between verruca plana and verruca plana-like seborrheic keratosis. J Dermatol. 2015;42:373-7.
- [Google Scholar]
- Evaluation of verruca plana by in vivo reflectance confocal microscopy and dermoscopy. Skin Res Technol. 2017;23:437-40.
- [Google Scholar]
- The use of dermoscopy for the diagnosis of plantar wart. J Eur Acad Dermatol Venereol. 2009;23:726-7.
- [Google Scholar]
- Differential diagnosis of plantar wart from corn, callus and healed wart with the aid of dermoscopy. Br J Dermatol. 2009;160:220-2.
- [Google Scholar]
- Pigmented wart due to human papilloma virus type 60 showing parallel ridge pattern in dermoscopy. Eur J Dermatol. 2009;19:643-4.
- [Google Scholar]
- Acral viral wart showing a parallel ridge pattern on dermatoscopy. Eur J Dermatol. 2009;19:381-2.
- [Google Scholar]
- Dermoscopy in general dermatology: practical tips for the clinician. Br J Dermatol. 2014;170:514-26.
- [Google Scholar]
- Cryotherapy versus CO2 laser in the treatment of plantar warts: a randomized controlled trial. Dermatol Pract Concept. 2018;8:168-73.
- [Google Scholar]
- A two-week interval is better than a three-week interval for reducing the recurrence rate of hand-foot viral warts after cryotherapy: a retrospective review of 560 hand-foot viral warts patients. Ann Dermatol. 2011;23:53-60.
- [Google Scholar]






