Translate this page into:
A Pocket-Friendly and Sustainable Iontophoresis Apparatus for Palmoplantar Hyperhidrosis: Advancement over a Previously Described Homemade Design
Address for correspondence: Dr. Sourabh Jain, Department of Dermatology, STD and Leprosy, All India Institute of Medical Sciences, Saket Nagar, Bhopal, Madhya Pradesh, India. E-mail: Sourabh.kem@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction and Objectives:
Tap water iontophoresis is a promising therapy for palmoplantar hyperhidrosis. Non-affordability and nonavailability of the marketed device restrict its usage for many patients hailing from villages or small cities.
Materials and Methods:
In an article named “A simple user-made iontophoresis device for palmoplantar hyperhidrosis” published previously in this journal, a simple inexpensive homemade device that runs on 12 V direct current battery was described. We made a small modification by using a 220–12 V alternate current to direct current semiconductor diode–based transformer for the current supply.
Results:
The added innovation made the device lightweight, cheaper, and usable with domestic electric supply at home/clinic. Sustained supply of current at same voltage without dip and non-requirement to change/replace battery are added advantages. Cost of the whole assembly is ₹310. Working and clinical efficacy of our device were comparable to the commercially available apparatus as reported by 13 patients who received thrice a week of 15min sessions with our device. Mild electric pricking sensation was felt by all patients. Four of thirteen reported that pricking sensation was a bit more with our device as compared to the marketed device. No calibration for intensity is available in our device.
Conclusion:
This simple to assemble and inexpensive device makes iontophoresis applicable in many needy patients with similar efficacy and few limitations compared to expensive marketed devices.
Keywords
Excessive sweating
hyperhidrosis treatment
inexpensive iontophoresis device
iontophoresis
palmoplantar hyperhidrosis
INTRODUCTION
Idiopathic (primary) hyperhidrosis is defined as excessive sweating without a clear etiology. Excessive sweating of the palmoplantar, axillary, or cervicofacial region usually occurs bilaterally and causes social, psychological, emotional, and professional difficulties for the afflicted. Its incidence is reported to be between 0.6% and 2.8% in both the genders.[12]
Tap water iontophoresis (TWI) is one of the safe and effective noninvasive first-line therapy in moderate and severe palmoplantar hyperhidrosis (PPH).[34] However, in a resource-poor setting such as ours, iontophoresis cannot be offered to all the affected patients because of high cost and/or nonavailability of the marketed device. Also frequent visits to hospital/clinics are not always possible for all patients. Thus, a home-based inexpensive device is the need of the hour for increasing acceptance of TWI in the management of PPH.
MATERIALS AND METHODS
A simple user-made iontophoresis device was described in this journal last year, which runs on 12 V direct current battery.[5] Excellent reduction in PPH without any adverse effects was reported within 3 months of therapy in one patient with the same device [Figure 1]. We made a small modification by using a 220–12 V alternating current (AC) to direct current (DC) semiconductor diode–based transformer for the current supply [Figure 2]. The transformer is easily available in most electrical shops and used in decorative light-emitting diode (LED) lights [Figure 3]. The components of the whole assembly with the cost are given in Table 1.

- Direct current battery–based homemade iontophoresis device described by Nagar and Sengar (Image used with permission from: Nagar and Sengar. A simple user-made iontophoresis device for palmoplantar hyperhidrosis. J Cutan Aesthet Surg 2016;9:32-3.)

- Semiconductor electronic transformer–based device connected to main AC current supply
- Easily available LED strip light adapter/transformer that converts 220 V/5 A AC current to 12 V/1.5 A DC current
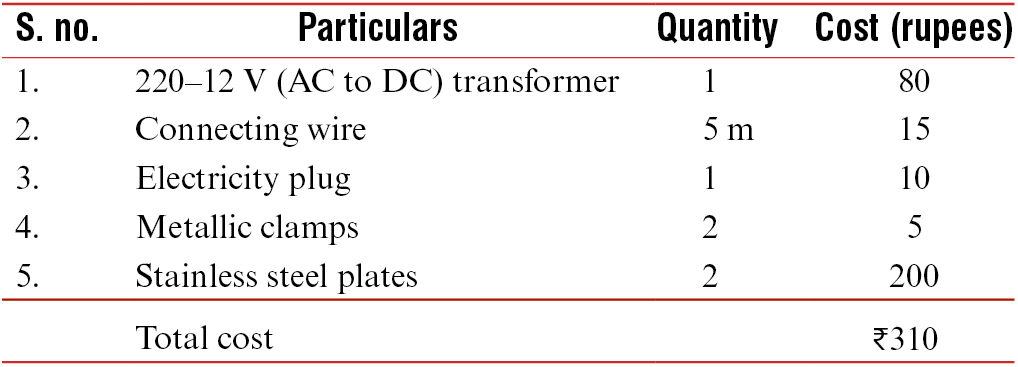
The transformer has the input end for AC supply. It is connected with the help of connecting wires and electricity plug to the domestic current supply. The two output ends of DC supply are connected with the help of wires and clamps to each stainless steel plates containing tap water. When the current is switched on, the device is ready to be used.
PROCEDURE
The stainless steel trays are to be placed on a nonconducting surface without touching each other. The trays are filled with tap water enough to completely dip the palms/soles. One clamp is connected to each of the tray and the 12-V DC flows through the transformer once it is connected to the main supply. The patient can be seated on a wooden stool or stand with shoes on and made to dip soles/palms in the trays [Figure 4].

- Tap water iontophoresis being performed in a patient of palmer hyperhidrosis
RESULTS
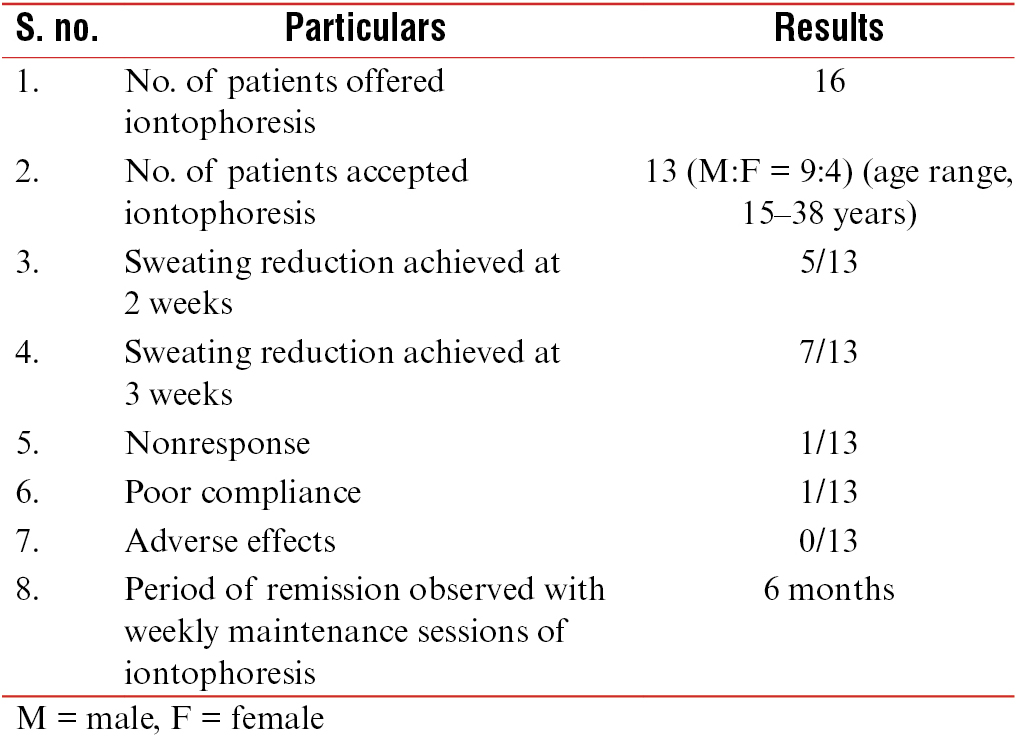
The added innovation made the device lightweight, cheaper, and usable with domestic electric supply at home/clinic. Sustained supply of current at same voltage without dip and non-requirement to change/replace battery are added advantages. TWI with our device was offered to 16 patients. However, only 13 (9 men, 4 women, age ranging from 15 to 38 years) of them could accept it. Other three did not accept the therapy because of fear/anxiety. The initial working of our device was compared with the commercially available device (manufactured by Dermaindia, Chennai, India) for all 13 patients. Mild electric pricking sensation was felt by all, which was similar to both the devices. Four patients told that pricking sensation was a bit more with our device as compared to the marketed device; however, all tolerated the therapy well. Further TWI was continued with our device. Three sessions of 15min each were given alternate days, 3 days in a week for 1 month. Five patients noted reduction in sweating at the end of 2nd week, whereas seven mentioned reduction in sweating after eight sessions in the 3rd week. One male patient did not get any reduction even after 16 sessions. He was then given tablet glycopyrrolate (1mg) twice daily. For other patients, TWI sessions were continued at the same frequency for 2 months. Thereafter, all the patients continued 15min session once a week as maintenance. One patient who stopped the therapy altogether experienced increased sweating after 3 weeks of discontinuation. Rest others did not complain of increase in sweating at 6-month follow-up. No objective tests (e.g., starch iodine test) were performed to measure the effectiveness. No adverse effects were noted. Results are summarized in Table 2.
DISCUSSION
TWI is a very promising but limitedly used therapy for idiopathic PPH.[34] A controlled trial including 112 patients of palmer hyperhidrosis showed that after eight treatments, sweating was reduced by 81.2% from the baseline. This reduction was seen 20 days after the eighth treatment with the mean return of symptoms occurring at 35 days.[6]
Marketed iontophoresis devices are not easily available and are expensive. To the best of our knowledge, Levit[7] was the first person to report a homemade iontophoresis device in 1968. However, assembling such a device as described by Levit[7] is cumbersome. With the advancement in electronics and use of semiconductor-based transformers, assembling can be made very simple as with our device. Although very simple, we have not come across any published reports or any clinicians who suggested such devices to the needy patients. The device described by Nagar and Sengar[5] was also designed by a patient himself who came from an engineering background. Such devices will increase not only acceptance but also long-term compliance in the maintenance phase. A recent report on compliance with TWI in PPH concluded that the main reason for poor compliance during maintenance phase was the lack of time to visit the hospital; on the other hand, some patients could do it regularly at home with the purchased device.[8]
Our device is usable with domestic electric supply and is expected to produce sustained current without voltage dip till the transformer is functioning well. Transformer, which may become nonfunctional with time, can be easily replaced. Although four patients told the pricking sensation was more, no serious side effects such as erythema, vesiculation, and fissuring were observed. Inability to calibrate the intensity of voltage was one major limitation; however, if desired, this can be achieved by using a coil-based transformer that costs around ₹300–₹500.
CONCLUSION
Homemade inexpensive devices such as this can make iontophoresis therapy widely accepted with better compliance. Similar efficacy and few limitations compared to expensive marketed devices are expected; however, further randomized trials with objective measurements can be conducted for better comparison.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Hyperhidrosis—causes and treatment of enhanced sweating. Dtsch Arztebl Int. 2009;106:32-7.
- [Google Scholar]
- US prevalence of hyperhidrosis and impact on individuals with axillary hyperhidrosis: results from a national survey. J Am Acad Dermatol. 2004;51:241-8.
- [Google Scholar]
- Canadian Hyperhidrosis Advisory Committee. A comprehensive approach to the recognition, diagnosis, and severity-based treatment of focal hyperhidrosis: recommendations of the Canadian hyperhidrosis advisory committee. Dermatol Surg. 2007;33:908-23.
- [Google Scholar]
- A simple user-made iontophoresis device for palmoplantar hyperhidrosis. J Cutan Aesthet Surg. 2016;9:32-3.
- [Google Scholar]
- Safe control of palmoplantar hyperhidrosis with direct electrical current. Int J Dermatol. 2002;41:602-5.
- [Google Scholar]
- Simple device for treatment of hyperhidrosis by iontophoresis. Arch Dermatol. 1968;98:505-7.
- [Google Scholar]
- Compliance with tap water iontophoresis in patients with palmoplantar hyperhidrosis. J Cutan Med Surg. 2014;18:109-13.
- [Google Scholar]






