Translate this page into:
A Prospective Observational Comparative Study of Novel Autologous Negative Pressure Epidermal Harvesting System (ANPEHS or EHS) and Suction Blister Grafting (SBG) in Treatment of Stable Vitiligo
Address for correspondence: Dr. Satish Chand, Department of Dermatology, Command Hospital Air Force, Cambridge Rd, Cambridge Layout, Jogupalya, Bengaluru 560007, Karnataka, India. E-mail: satishfz84@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Vitiligo surgery has evolved a long way from punch skin grafts to the epidermal cell suspension and latest to the extracted hair follicle outer root sheath cell suspension transplantation (EHFORSCS). In the latest development, the novel technique autologous negative pressure epidermal harvesting system (ANPEHS) seems to be a good addition to the prevailing therapy in vitiligo.
Aims and Objectives:
The aim of this work was to study and compare novel ANPEHS and suction blister grafting (SBG) in the treatment of stable vitiligo.
Materials and Methods:
This was a prospective, single-centered, observational, open-labeled comparative study of the rate and final extent of repigmentation in ANPEHS or EHS and SBG in the management of stable vitiligo. The patients in this study were drawn from the outpatient Department of Dermatology of a Tertiary Care Hospital of the Armed Forces from July 1 2015 to December 31, 2016. A total of 40 patients with at least two comparable depigmented patches of 6 months’ stability were recruited. Both procedures were performed in the same patient on the same day. Informed consents were taken from all the patients. Each patient in the study had undergone a detailed clinical, general physical, systemic, and a dermatological examination. Clinical photographs had been taken before and after grafting, monthly for the first 6 months then bimonthly for the next 6 months. Donor site was preferably inner aspect of thigh.
Statistical Analysis Used:
“Chi-square test” and “statistical significance” (P value) methods.
Results:
Of total 80 patches, excellent results were seen in 82.9% patches by using the EHS method and 80% excellent results by using the SBG method. Similarly, very good results were seen in 2.9% patches and good results in 5.7% patches by using both methods. 11.4% patches showed poor results by using the SBG method and 8.6% patches showed poor results by using the EHS method.
Conclusions:
The EHS method is a simple, painless, less time-consuming, expensive but effective technique to produce homogeneous repigmentation without any donor site anesthesia and complication.
Keywords
Autologous negative pressure epidermal harvesting system
stable vitiligo
suction blister grafting
INTRODUCTION
Vitiligo is an acquired skin disease, characterized by depigmented or hypopigmented macules, which results from absence or reduction in melanocytes in the skin and/or mucous membranes that affect 1% of the world’s population and it has immense sociopsychological ramifications in addition to its cosmetic disability. The highest incidence of the condition has been reported in India, followed by Mexico and Japan.[12] Although vitiligo does not cause direct physical impairment, it can produce an important psychosocial burden in the form of poor body image, low self-esteem, and experience a considerable level of disability.[3] Various therapeutic options for repigmentation of vitiligo are available, including medical therapy (topical and oral) and phototherapy. The vitiliginous areas may remain static without showing any repigmentation or depigmentation to medical therapy and phototherapy. Such type of patients with disease stability of 1-year duration are considered appropriate for surgical treatment with a wide variety of methods; these include mini punch grafting (MPG),[4] suction blister epidermal grafting (SBEG),[5] thin split-thickness grafting (TSTG),[6] transplantation of basal cell layer-enriched suspension (noncultured melanocyte transfer),[7] cultured epithelial/melanocytes transplantation,[89] single hair follicle transplant, and recently developed “modified dermabrasion” (MD) which uses dermabraded epidermal material (melanocytes and keratinocytes) entangled in an antibiotic paste.[10]
Cellular transplantation methods include cultured and noncultured mixed melanocyte–keratinocyte suspension with or without carrier, and cultured pure melanocyte suspension.[11] Problems such as scarring, cobblestoning, and milia formation in addition to issues regarding area of coverage per sitting and inadequate donor area in extensive cases exist in tissue grafting techniques; 100% repigmentation of vitiligo cannot be obtained with any of the existing surgical methods of treatment of vitiligo.[12]
There is no study from India comparing conventional technique suction blister grafting (SBG) and novel technique epidermal harvesting system (EHS) in the treatment of stable vitiligo. However, there is no consensus regarding which surgical technique is preferred in stable vitiligo lesions of equal size and also the effectiveness of the surgical technique at a particular site or the surgical technique that is going to produce early repigmentation. It is necessary to rigorously study these two modalities of vitiligo grafting in areas of depigmentation to compare the rate of repigmentation as well as the final extent of repigmentation to standardize and validate the protocols for the performance of these procedures in our population.
MATERIALS AND METHODS
This was a prospective, single-center, observational, open-labeled comparative study of the rate of pigmentation at specified intervals and the final extent of pigmentation achieved at the end of 1 year of EHS and SBG in the treatment of vitiligo. The patients in this study were drawn from the outpatient Department of Dermatology of a Tertiary Care Hospital of the Armed Forces from July 1, 2015 to December 31, 2016. Ethical clearance was obtained before starting the study.
A total of 40 patients with at least two unresponsive depigmented patches in each patient were enrolled (both procedures were performed on the same patient on the same day). All patients of age group 16–60 years and both sexes with stable vitiligo, which is defined as no new lesions or increase in the size of existing lesions in the past 6 months, were included in the study. Patients having active vitiligo, active infection, keloidal tendency, unrealistic expectations, patients having less than two patches, patch over lips, and glans penis were excluded from the study.
Informed consents were taken from all the patients. Each patient in the study had undergone a detailed clinical, general physical, systemic, and a thorough dermatological examination with a set of investigations consisting of hemoglobin, total leukocyte count, differential leukocyte count, blood sugar (fasting and postprandial), hepatitis B, hepatitis C, venereal disease research laboratory (VDRL), and human immunodeficiency virus (HIV). Clinical photographs had been taken before the surgical procedure and every month for the first 6 months, then every 2 months for the next 6 months using standard aperture and lighting for the assessment. The sites were sequentially distributed into two groups of 40 each. In total, 40 sites into Group A were subjected to SBG and 40 sites into Group B were subjected to EHS. To calculate the size of vitiligo lesions, margins of rectangular lesions and radius of circular lesions were measured with a centimeter scale. Irregular big lesions were first divided into the nearest geometrical shapes, and then the areas were calculated.
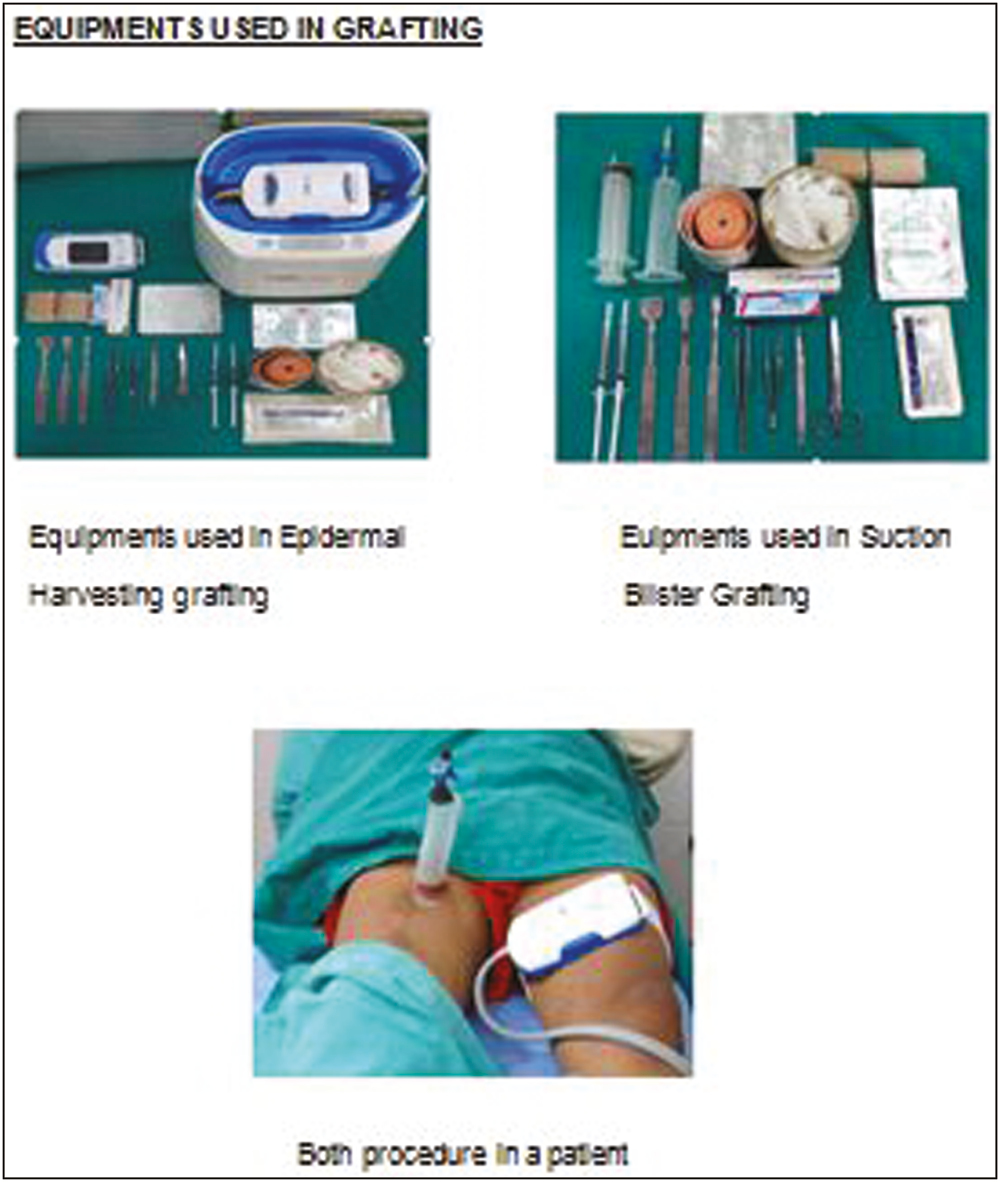
Suction blister grafting technique
Donor will be premedicated with antibiotics, shaving of donor site will be performed, and local anesthetic with 1% lignocaine will be given.[513141516] In this procedure, a 50-cc syringe will be used. Piston of the syringe will be removed and three-way connector will be attached to its needle end piece. The basal rim of this 50-cc syringe will then be applied to the fully stretched donor site. An assembly line consisting of polyvinyl tubing (intravenous [IV] line), three-way connectors, manometer (vacuum gauge), and 50-cc syringe will then be attached to the three-way connector of the 50-cc syringe. Suction will then be given by the 50-cc syringe and will be monitored on the connected vacuum gauge so as to create negative pressure of 250–350 mm Hg. The 50-cc syringe along with the attached three-way connector will be retained by changing the position of lock of three-way connector. Due to the negative pressure inside the basal rim of syringe, it will remain adherent to the donor site in a vertical position along with the attached three-way connector. Multiple such 50-cc syringes will be applied similarly next to each other as per the area of recipient site required to be grafted. Negative pressure will be retained for 1–2h. Time required for separation will be 1–2h. Local anesthetic with 1% lignocaine will be given. Vitiligo area will be dermabraded till pinpoint bleeding seen and dermabrasion will be performed 1–2 mm beyond the vitiligo area. Blister will be cut all along its border with curved iris scissors and its roof will be everted over glass slide which will be smeared with antibiotic cream which prevents chances of graft rejection and wrong placement of epidermal side. Over the dermabraded recipient area, glass slide with graft will be inverted. Each graft will be individually implanted. Graft edges should extend 1–2 mm beyond the vitiligo area. Surgical glue (N-butyl-2-cyanoacrylate) will be applied to the free edges of graft and not over dermabraded area. A distance of half inch to 1 inch between two adjacent droplets will be kept. Dressing will be performed with double layer of Framycetin Tulle, two layers of gauze piece, and pressure dressing with elastoplasts. If seroma is present, dressing will be opened after 24h. It will be drained by puncturing and redressing, otherwise dressing will be removed after 10–12 days. Topical/Systemic Psoralen Ultraviolet A Solution (PUVASOL) therapy will be advised to the patient as indicated; it will be started 3–5 days after removing the dressing and will be given thrice a week on nonconsecutive days according to standard protocol (0.1%). Psoralen topical application followed by sun exposure after 30 min for 30–60s increased by 30s per sitting and frequency to biweekly or triweekly sittings until the desired faint erythema is achieved. After treatment, the area should be washed with soap and water and covered with clothing or with a broad spectrum sunscreen).
Autologous negative pressure epidermal harvesting system Grafting
The system uses a combination of suction and warmth to enable cell splitting within the skin by causing the formation of tiny blisters (epidermal microdomes) on the skin surface.[17181920] These microdomes consist of skin tissue (epithelium) and cells (keratinocytes) which are harvested into skin grafts (epidermal micrografts). The EHS consists of (i) a control unit, which creates and regulates the suction (negative pressure: –400 to –500 mm Hg) and warming (37°C–41°C) required to raise the epidermal microdome; (ii) a vacuum, which delivers the suction pressure and warmth to the harvester; and (iii) a harvester, which provides the grid for microdome formation. The harvester will be positioned at the donor site on the patient’s inner thigh and delivers pressure and warmth to initiate the microdome raising process. An array of 128, 2 mm wide microdomes form gradually over approximately 30–40 min. Complete microdome formation will be confirmed by visual observation of microdomes with a raised height and encapsulating a clear fluid. The harvester then will cut the layer of skin with raised microdomes, which will be captured by 3M Tegaderm (3M, 12930 W Interstate 10, San Antonio, USA) film dressing. The film dressing with attached microdomes will create a transferrable skin micrograft, which should ideally be applied to the recipient site within 2 min of procurement. A Tegaderm film dressing will also be placed at the donor site after harvesting. The Tegaderm film will be perforated with an 18-gauge needle to allow for drainage of potential transudate. The patient will be instructed to leave the dressing intact and to return for review in 5–7 days. A nonadherent layer followed by a dry sterile dressing and four-layer compression will be reapplied, and the patient will be instructed to return for dressing. Topical PUVASOL therapy will be same as SBG.
Follow-up
The patients for both procedures were followed up at monthly intervals for the first 6 months and then every 2 months for the next 6 months. The response to the therapy was assessed subjectively as well as objectively. Subjective assessment was performed by the patient. Objective assessment was carried out using photographic evidences with standard aperture and lighting by two separate observers. Response to treatment was evaluated based on the degree of repigmentation, which was carried out at monthly intervals for the first 6 months and then every 2 months for the next 6 months. Final evaluation of area of involvement was performed after completion of 1 year. Rate of repigmentation was recorded as per the proforma. The response to the treatment based on the percentage of visible repigmentation will be graded as follows: poor: 0%–25%; good: 26%–50%; very good: 51%–75%; and excellent 76%–100%.
The response in terms of onset of repigmentation, type of repigmentation, and degree of repigmentation in both groups was considered for the analysis. The results were statistically analyzed using “chi-square test” and “statistical significance” (P value) methods.
RESULTS
Of 40 patients, 35 completed the study period of 12 months. Therefore, data of 35 patients including two depigmented patches in the same patients were considered for the analysis [Figures 1–9].
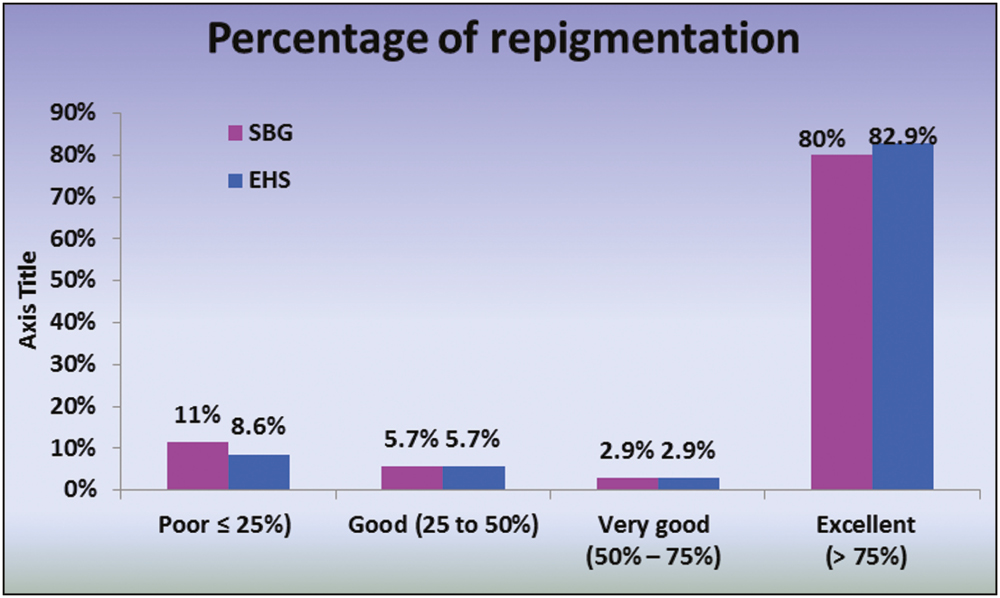
- Comparison of degree of repigmentation (objective) in both groups at the end of the 12 months
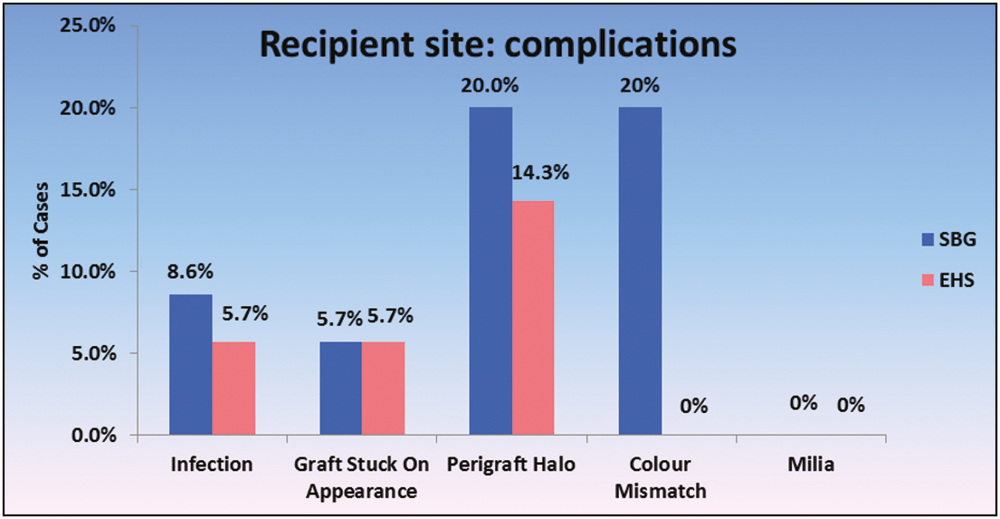
- Comparison of complication at recipient site in both groups
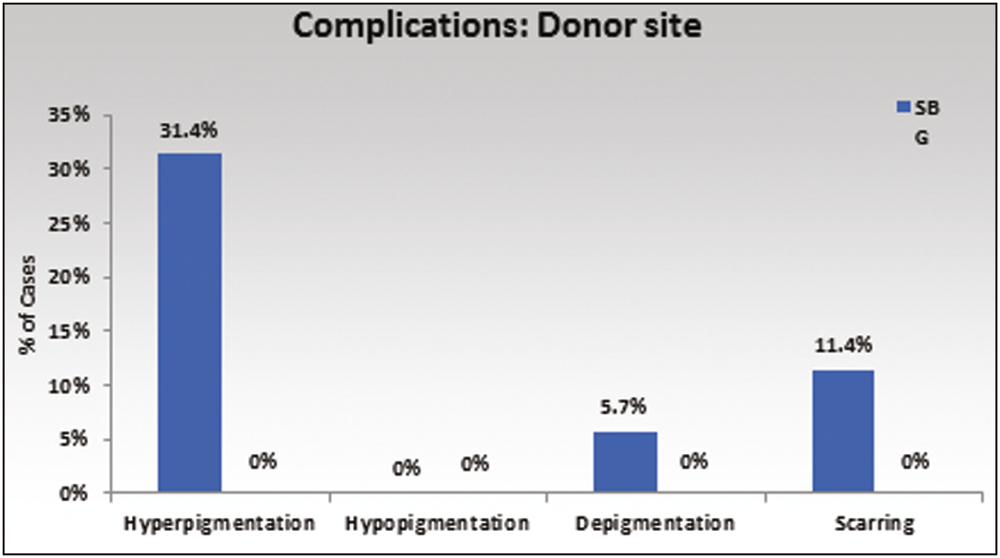
- Comparison of complication at donor site in both groups

- Comparison of repigmentation in both groups after 6 months

- Comparison of repigmentation in both groups after 6 months

- Comparison of repigmentation in both groups after 6 months
- EHS and SBG in a vitiligo patient

- Stepwise SBG grafting in a vitiligo patient

- Stepwise EHS grafting in a vitiligo patient
Demographic characteristics are shown in Table 1. Both procedures were performed in the same patient so both groups were comparable with regard to age, sex, and type of vitiligo. The majority (18/40) of the patients had vitiligo vulgaris. Distribution of vitiligo lesions was not comparable, but the period of stability was comparable in all patients.
| Characteristics | Group A (SBG) | Group B (EHS) |
|---|---|---|
| NUMBER OF PATIENTS | 35 | 35 |
| NUMBER OF LESIONS | 35 | 35 |
| AGE RANGE | 18-51 years | 18-51 years |
| AGE (years; mean±2SD) | 32.85 ± 10.04 | 32.85 ± 10.04 |
| SEX (male:female) | 2:3 | 2:3 |
| Duration of disease | 5.59 ± 5.00 years | 5.59 ± 5.00 years |
| (years; mean ± 2SD) | ||
| Period of stability (years; mean ± 2SD) | ||
| Type of vitiligo | 18/17/4/1 | |
| (nonsegmental/ focal/segmental/ acrofacial) |
Both Groups A and B had the maximum number of lesions over the extremities (82.5% and 80%, respectively), whereas only a few lesions were seen over trunk and acral parts with no lesions over flexures.
As shown in [Figure 1], total 70 patches operated on; excellent results were seen in 82.9% patches by using the EHS method and in 80% by using the SBG method. Similarly, very good results were seen in 2.9% patches and Good results in 5.7% patches by using both methods. 11.4% patches showed poor results by using the SBG method and 8.6% patches showed poor results by using the EHS method.
By using both the methods, patches over face, trunk, legs, and ankle showed good repigmentation, whereas patches over feet and elbow showed poor repigmentation.
There was a statistically significant difference in the rate of repigmentation in both procedures observed, that is, repigmentation rate was more in SBG graft during the second month.
Figure 2 shows the complications observed in the recipient site such as infections, graft stuck on appearance, perigraft halo, color mismatch, and milia, whereas Figure 3 shows the complications observed in the donor site such as hyperpigmentation, hypopigmentation, depigmentation, and scarring.
Small polka dot appearance was observed with EHS grafting on the recipient site.
DISCUSSION
There is an increasing trend toward the use of advanced technology in the surgical treatment of stable vitiligo. However, these technologies are not available at most of the treatment centers making them inaccessible to most patients. Replenishing melanocytes selectively in vitiliginous macules by grafting is a promising treatment. Both the EHS and SBG techniques are essentially based on the principle of seeding of melanocytes. Grafting is a state of the art procedure that requires expertise and is being practiced in a few centers only.
Among the study population, of total 40 patients, 16 were males (40%) and 24 were females (60%). Female preponderance was seen in the different studies as shown in Table 2. Our study also showed female preponderance sex distribution among the study population. The greater number of reports among females is probably due to the greater social consequences to women and girls affected by this condition.
In our study, the mean duration of vitiligo in all 40 patients was 5.59 ± 5.00 years. In both groups, the minimum duration of vitiligo was 3 years and the maximum duration was 10 years. Our groups were comparable to other studies as shown in Table 3.
In this study, among the study groups vitiligo vulgaris was present in 18 (45%) patients, focal vitiligo was present in 17 (42.5%) patients, segmental was present in 4 (10%) patients, and 1 (2.5%) patient had acrofacial vitiligo. Vulgaris type of vitiligo was present in most number of patients in our study and similarly in other studies as shown in Table 4.
Extent of the repigmentation was calculated by percentage of repigmentation. We divided percentage of repigmentation into four groups. Similar groups were formed in other studies; however, Ko and Chen divided percentage of repigmentation into >90%, 50%–90%, 20%–50%, and <20% groups.
After 12 months of procedure, percentage of repigmentation was calculated for both groups. In the SBG method, 28 (80%) patches showed excellent repigmentation, that is, more than 75% repigmentation, 1 (2.9%) patch showed very good repigmentation, that is, 50%–75% repigmentation, 2 (5.7%) patches showed good repigmentation, that is, 25%–50%, and 4 (11.4%) patches showed poor repigmentation, that is, less than 25%.
In the EHS method, 29 (82.9%) patches showed excellent repigmentation, that is, more than 75% repigmentation, 1 (2.9%) patch showed very good repigmentation, that is, 50%–75% repigmentation, 2 (5.7%) patches showed good repigmentation, that is, 25%–50%, and 3 (8.6%) patches showed poor repigmentation, that is, less than 25% repigmentation.
The percentage of repigmentation and final outcome was dependent on the site of the vitiligo lesions. As per the study by Pandya et al.,[25] the results were most favorable on the legs, feet, face, and forearms. Results were poor on the elbows and acral areas of the hand. Repigmentation was not observed in any of the control patches. As compared to the other studies in the literature, repigmentation was poor over bony prominences and nonhairy acral areas. Patches over face, trunk, and legs showed good repigmentation by using both the methods, whereas patches over elbow and feet had poor repigmentation. Both SBG and EHS were tried over bony prominences and acral areas. Our groups were not matched with respect to the site. This restricted us to compare the results according to sites.
Limitation of study
Till date, there is no study comparing EHS and SBG in treatment of stable vitiligo so it was necessary to rigorously study these two modalities of epidermal grafting in areas of depigmentation to confirm or refute these findings, as well as to standardize the protocols for the performance of these procedures in our population.
CONCLUSION
In our study, both procedures were performed in the same patient so various confounding factors such as sex, age of patient, and duration of disease were comparable in both the groups. The most common type of vitiligo was of vitiligo vulgaris type. Both groups showed comparable final extent of repigmentation after 12 months, however patients in the EHS group more patches showed excellent results and SBG group more patches showed poor results. During the initial few months, the rate of repigmentation was higher in SBG graft, but the final extent of repigmentation was found to be higher in EHS graft comparatively.
EHS is a simple, painless, less time-consuming, expensive but effective technique to produce homogeneous repigmentation without any donor site anesthesia and complication. SBG is time-consuming, painful, and labor-intensive technique with more infection over donor as well as recipient site, color mismatch, depigmentation, and hyperpigmentation over donor site, so EHS grafting technique has an advantage over conventional SBG technique.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Vitiligo: compendium of clinico-epidemiological features. Indian J Dermatol Venereol Leprol. 2007;73:149-56.
- [Google Scholar]
- Repigmentation of stable leukoderma by autologous minigrafting. J Dermatol Surg Oncol. 1986;12:172-9.
- [Google Scholar]
- Transplantation of melanocytes by epidermal grafting. An Indian experience. J Dermatol Surg Oncol. 1993;19:231-4.
- [Google Scholar]
- Repigmentation in vitiligo patients. Melanocyte transfer via ultra-thin grafts. Dermatol Surg. 1998;24:365-7.
- [Google Scholar]
- Leucoderma treated by transplantation of a basal cell layer enriched suspension. Br J Dermatol. 1998;138:644-8.
- [Google Scholar]
- A surgical treatment for vitiligo: autologous cultured-epithelial grafts. J Dermatol Surg Oncol. 1989;15:1161-6.
- [Google Scholar]
- Keratinocyte-melanocyte graft technique followed by PUVA therapy for stable vitiligo. Indian J Dermatol Venereol Leprol. 2008;74:622-4.
- [Google Scholar]
- Treatment of “stable” vitiligo by timedsurgery and transplantation of cultured epidermal autografts. Arch Dermatol. 2000;136:1380-9.
- [Google Scholar]
- Modified technique of suction blistering for epidermal grafting in vitiligo. Int J Dermatol. 1999;38:306-9.
- [Google Scholar]
- Use of octyl-2 cynoacrylate for skin closure in facial plastic surgery. Plast Reconst Surg. 1998;102:2209-19.
- [Google Scholar]
- Suction blister technique. In: Satish S, Sawant , eds. Textbook of dermatosurgery & cosmetology (2nd ed.). Mumbai, India: ASCAD; 2008. p. :357.
- [Google Scholar]
- Autologus graft by suction blister technique in management of vitiligo. Ind J Dermatol Venereol Leprol. 1991;57:91-3.
- [Google Scholar]
- Use of a novel epidermal harvesting system in resource-poor countries. Adv Skin Wound Care. 2015;28:107-12.
- [Google Scholar]
- Initial experience with a new epidermal harvesting system: Overview of epidermal grafting and case series. Surg Technol Int. 2014;25:55-61.
- [Google Scholar]
- Epidermal micrografts produced via an automated and minimally invasive tool form at the dermal/epidermal junction, and contain proliferative cells that secret wound healing growth factors. Adv Skin Wound Care. 2015;28:397-405..
- [Google Scholar]
- Clinical trial to evaluate blister graft utilizing a novel harvesting device for treatment of venous leg ulcers [Online]. Available from: http://www.clinicaltrials.gov/ct2/show/NCT02148302
- Suction blister epidermal grafts combined with CO2 laser superficial ablation as a good method for treating small-sized vitiligo. Dermatol Surg. 2009;35:601-6.
- [Google Scholar]
- Suction blister epidermal grafting versus punch skin grafting in recalcitrant and stable vitiligo. Dermatol Surg. 1999;25:955-8.
- [Google Scholar]
- Punch grafting versus suction blister epidermal grafting in the treatment of stable lip vitiligo. Dermatol Surg. 2008;34:166-78; discussion 178.
- [Google Scholar]
- Epithelial grafting for vitiligo requires ultraviolet A phototherapy to increase success rate. J Cosmet Dermatol. 2007;6:119-24.
- [Google Scholar]
- A study of autologous melanocyte transfer in treatment of stable vitiligo. Indian J Dermatol Venereol Leprol. 2005;71:393-7.
- [Google Scholar]






