Translate this page into:
A Randomized Control Trial of 20% Glycolic Acid Versus 30% Salicylic Acid in the Management of Molluscum Contagiosum
Address for correspondence: Dr. Bhikam Chand Ghiya, Department of Dermatolgoy, Venereology and Leprosy, Sardar Patel Medical College, Bikaner, Rajasthan 334001, India. E-mail: bcghiya@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Molluscum contagiosum (MC) is a common self-limiting viral infection of the skin. Many therapeutic agents have been used for it with varying success rates.
Objective:
To evaluate and compare the efficacy and safety profile of topical 20% glycolic acid and 30% salicylic acid in the treatment of MC in pediatric patients.
Materials and Methods:
All patients of MC between 1 and 15 years of age attending the outpatient department of dermatology were randomized into two treatment groups A and B. Group A was treated with 20% glycolic acid solution, and group B was treated with 30% salicylic acid solution daily for 4 weeks. Parents of patients were instructed to apply the medication once daily at night for 1 h on the lesions only. The assessment of response and side effects were analyzed in all the patients weekly for 4 weeks during the daily treatment protocol. Follow-up was done monthly for 3 months after the completion of therapy.
Results:
At the end of 4 weeks, group A patients (60 patients) were treated with 20% glycolic acid out of which 34 (56.66%) patients had a complete clearance of lesions. Group B patients were treated with 30% salicylic acid out of which 38 (63.33%) had a complete clearance of lesions. Secondary bacterial infection was the most common side effect followed by postinflammatory hyperpigmentation in both groups.
Conclusion:
30% salicylic acid was found to be more effective and has less side-effect profile in the treatment of MC than 20% glycolic acid.
Keywords
20% glycolic acid
30% salicylic acid
molluscum contagiosum
INTRODUCTION
Molluscum contagiosum (MC) is a self-limiting infectious disease that is frequently observed in the pediatric population, sexually active adults, and immunocompromised individuals. It is caused by the molluscum contagiosum virus (MCV), which is a double-stranded DNA virus of the Poxviridae family.[1] Humans are the only host.[1] Patients infected with MCV usually present with firm, round papules of 2–5 mm size, pink- or skin-colored, with a shiny and umbilicated surface. In children, the commonly affected areas are the face, trunk, extremities, intertriginous regions, and genitals except for palms and soles.[2] The incubation period of MCV is variable between 2 and 6 weeks. Lesions are self-limiting, which heal within a period of 6–9 months.[3] It mainly affects children between 2 and 5 years of age and rarely below the age of 1 year. The diagnosis of the MC is done clinically, based on the classical characteristics of the lesions. In ambiguous cases, histopathology or dermoscopy is indicated.[45]
Treatment options for MC include extirpation, topical therapy, and oral therapy. Physical treatment modalities such as curettage, cryotherapy, needle extraction, electrodesiccation, photodynamic therapy, and laser ablation have good results but are poorly tolerated in children. Topical treatment includes trichloro-acetic acid, salicylic acid (SA), glycolic acid (GA), tretinoin, tazarotene, liquefied phenol, cantharidin, and potassium hydroxide. Oral treatments, namely, cimetidine, ranitidine, zinc, etc., only have a limited role.[6] Both GA and SA act against MC by causing the chemical necrotization of virus-infected keratinocytes.
In the current study, we compared the efficacy and safety of topical 20% GA with 30% SA in MC in pediatric patients.
MATERIALS AND METHODS
This was a hospital-based prospective randomized comparative study conducted in patients having MC, at our Dermatology, Venereology, and Leprosy, out-patient department from January 2020 to December 2020. The study was initiated after obtaining due approval from the institutional ethical committee.
Patients between 1 and 15 years of age, diagnosed as MC on clinical grounds, were enrolled in our study. Written informed consent was taken from parents of children, and additionally, also gave assent to be enrolled in the study.
Patients with active infection below 1 year and greater than 15 years of age were excluded. Additionally, any immunocompromised children, patients with keloidal tendency, or those with known hypersensitivity to any component of GA and SA solution were excluded. Information regarding age, sex, site of lesions, number of lesions, and previous treatment was recorded.
After explaining the procedure, the subjects were randomly allocated into two groups, namely, group A (20% GA) and group B (30% SA).
The sample size for each group was calculated using the probability of 90% with a significant result considered at 5%, giving the sample size to be 60 per group.
The study was participant blinded. Unstratified randomization was done using an open list of computer-generated random numbers chosen by the participant. The random number was mentioned on the patient’s prescription for further visits.
Both 20% GA solution and 30% SA solution were prepared at the Department of Pharmacology of our institution. In group A and group B, 20% GA solution and 30% SA solution were given daily for 4 weeks, respectively. Patient/patient’s relatives were instructed to apply medication once daily at night over the lesions only. The parents were advised not to apply any other agent over MC for the entire duration of treatment. The assessment of the response of the treated lesions and side effects was done weekly for 4 weeks. Follow-up was done monthly for 3 months after the completion of therapy.
Treatment response was measured as a complete cure: the disappearance of all lesions in the treatment period; moderate improvement: the disappearance of more than 50% of lesions; slight improvement: the disappearance of less than 50% of lesions; no response: persistence of all lesions throughout treatment period; relapse was labeled if there was the appearance of new lesions at a previously healed site within 3 months of the completion of treatment protocol.
RESULTS
Out of 132 patients, 120 patients completed the study with 60 patients in each group. The remaining eight patients in group A and four patients in group B discontinued the treatment with poor compliance.
The baseline demographic data were comparable between the two groups [Table 1].
| Group A (20% GA) | Group B (30% SA) | |
|---|---|---|
| Age distribution (years) | ||
| Range | 1–15 | 1–15 |
| Mean ± SD | 7.1 ± 3.7 | 6.1 ± 3.6 |
| Gender distribution | ||
| Male | 35 | 42 |
| Female | 25 | 18 |
| Male:female | 1.4:1 | 2.3:1 |
| Duration of MC (days) | ||
| Mean ± SD | 13.2 ± 8.1 | 13.5 ± 6.5 |
| Mean number of MC | ||
| Mean ± SD | 11.8 ± 3.2 | 9.2 ± 3.9 |
SD = standard deviation
In group A patients of MC, lesions were present most commonly on the face (45%), followed by trunk (18%). Similarly in group B patients of MC, lesions were present most commonly on the face (43%), followed by trunk (28%) [Figure 1]. None of the patients had periorbital lesions.
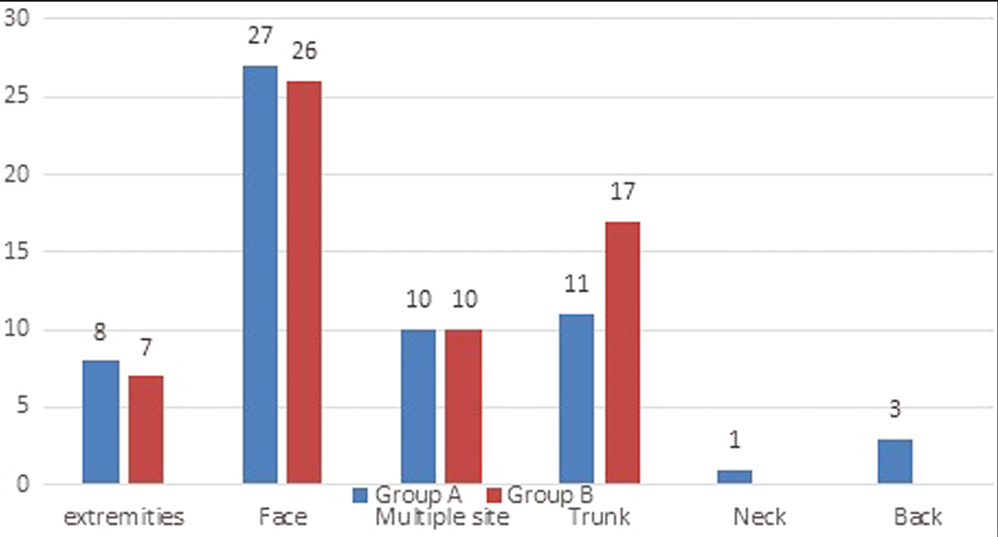
- Comparative analysis of the site of MC in two groups
Pseudokoebnerization was present in 16 (28%) patients in group A and 14 (25%) patients in group B. The incidence of pseudokoebnerization was comparable between the two groups (P = 0.17). Atopic dermatitis was present in 14 (23%) patients in group A and 12 (20%) patients in group B. Patients with atopic dermatitis had a higher incidence of pseudokoebnerization.
Among the two groups of patients, there was a higher rate of complete response in group B than in group A [Figure 2]. In group A, the complete clearance was seen in 34 (56.66%) patients, moderate improvement was seen in 16 (26.66%) patients, whereas the remaining 10 (6.67%) patients showed signs of only slight improvement [Figure 3A and B]. On the other hand, in group B, the complete clearance was seen in 38 (63.33%) patients, moderate improvement was seen in 12 (20%) patients, whereas the remaining 10 (16.66%) patients showed a slight improvement [Figure 4A and B]. The results among the two groups were, however, comparable, and the difference in response was statistically nonsignificant (P = 0.67). Most of the cases having moderate or slight improvement had large MC.
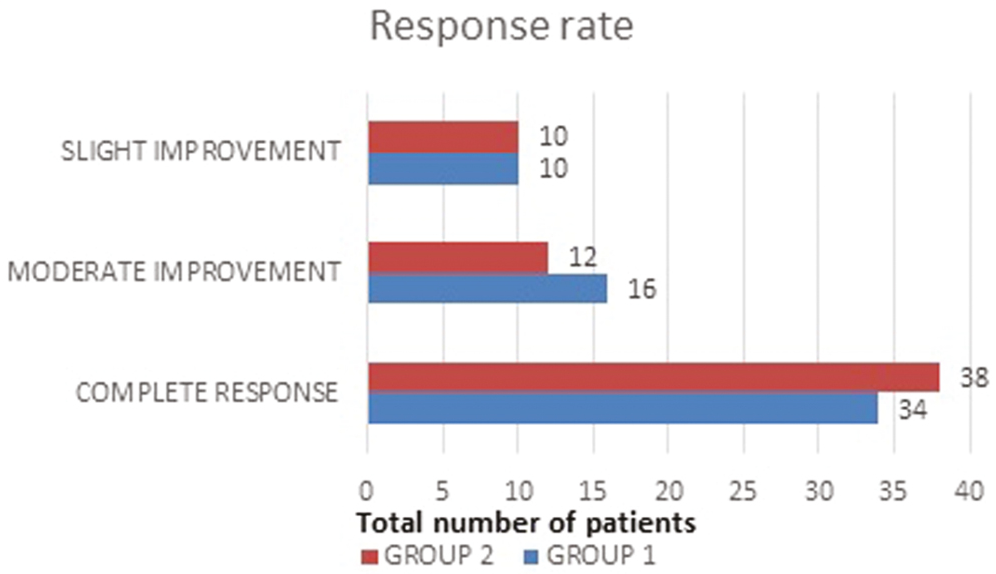
- Comparison of the clearance rate of MC in both groups
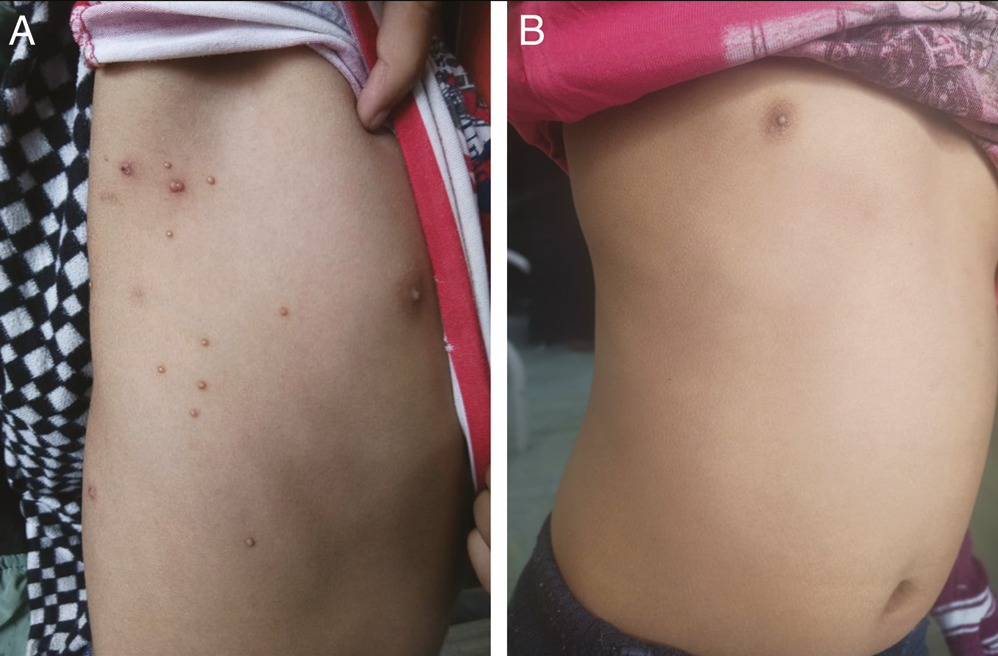
- (A) A 9-year-old boy with MC showing before the procedure, and (B) after the procedure (20% GA) after 4 weeks
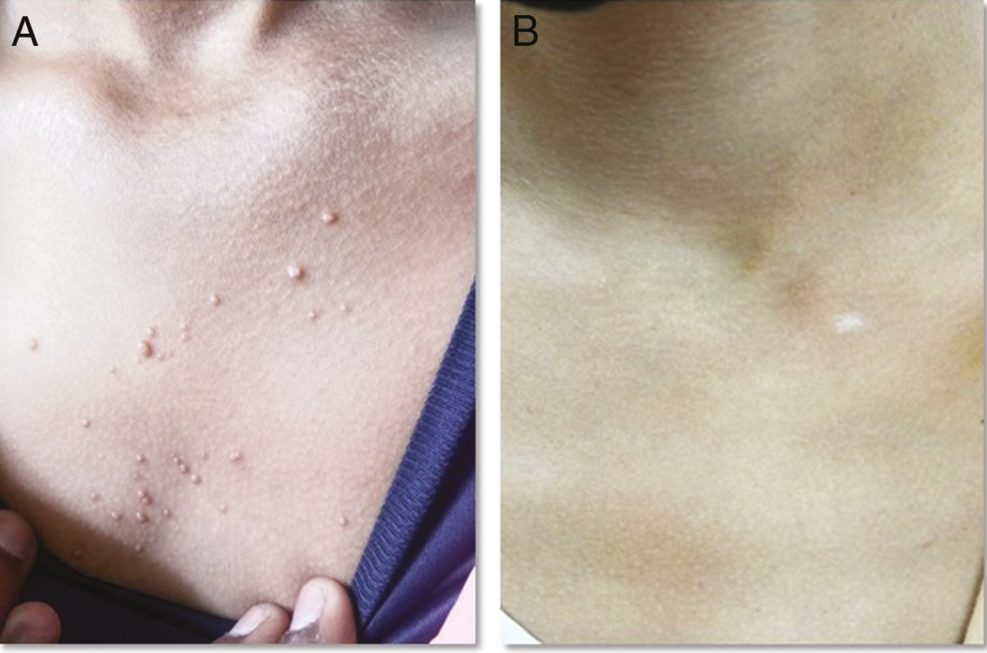
- (A) A patient with MC showing before the procedure, and (B) after the procedure (30% SA) after 4 weeks
In group A, out of 60 patients, 18 (30%) patients showed adverse events. The most common adverse event was secondary bacterial infections in eight (44.4%) patients [Figure 5] followed by postinflammatory hyperpigmentation in five (27.7%) patients. Similarly in group B, out of 60 patients, 16 (26.6%) patients showed adverse events [Figure 6A and B]. The most common adverse event was secondary bacterial infections in six (37.5%) cases, followed by postinflammatory hyperpigmentation in five (31.2%) patients. The most common site of postinflammatory hyperpigmentation in both groups was face. In our study, none of the patients with the complete clearance had relapse in any of their lesions during the 3 months of follow-up.
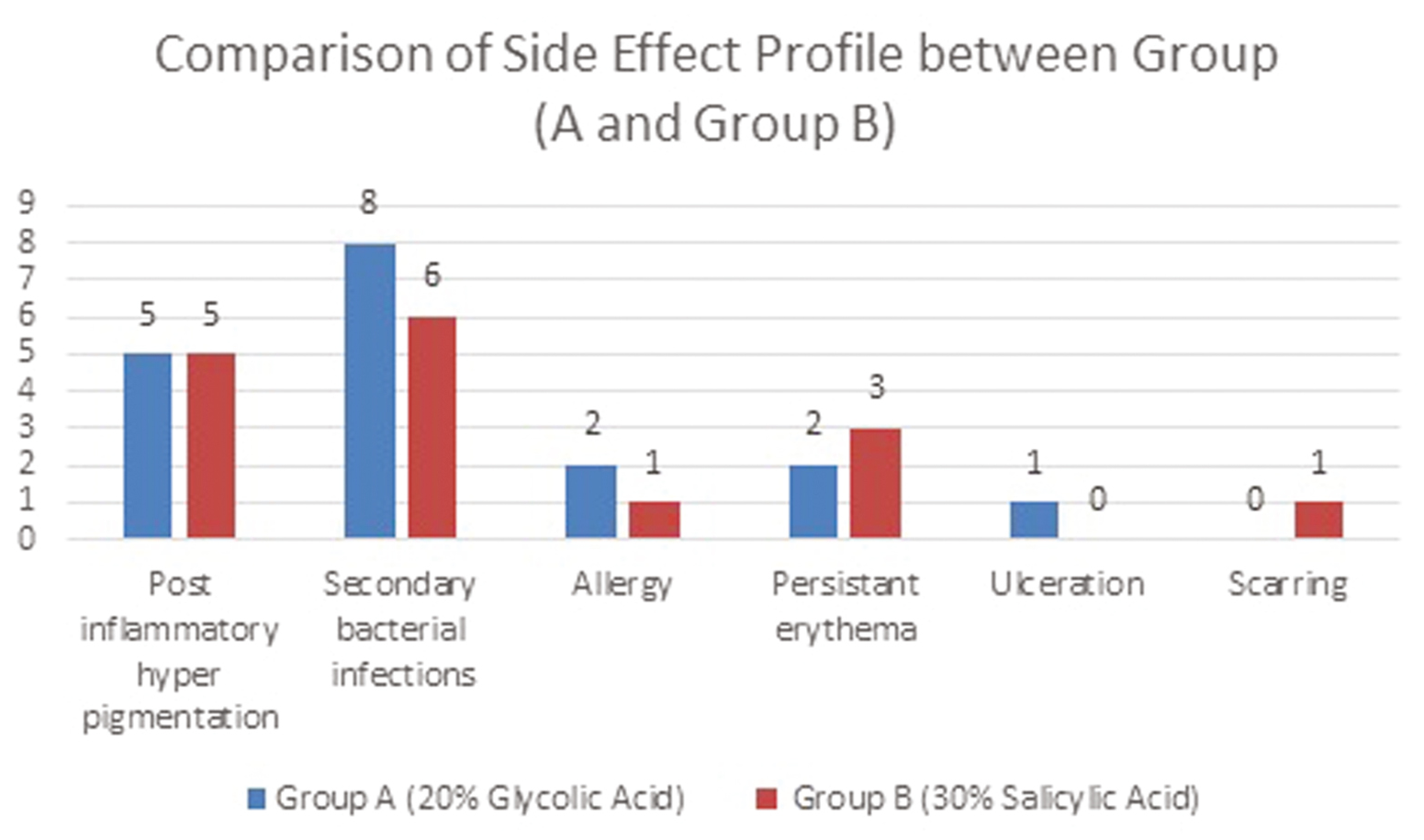
- Comparison of the side effect profile between group A and group B
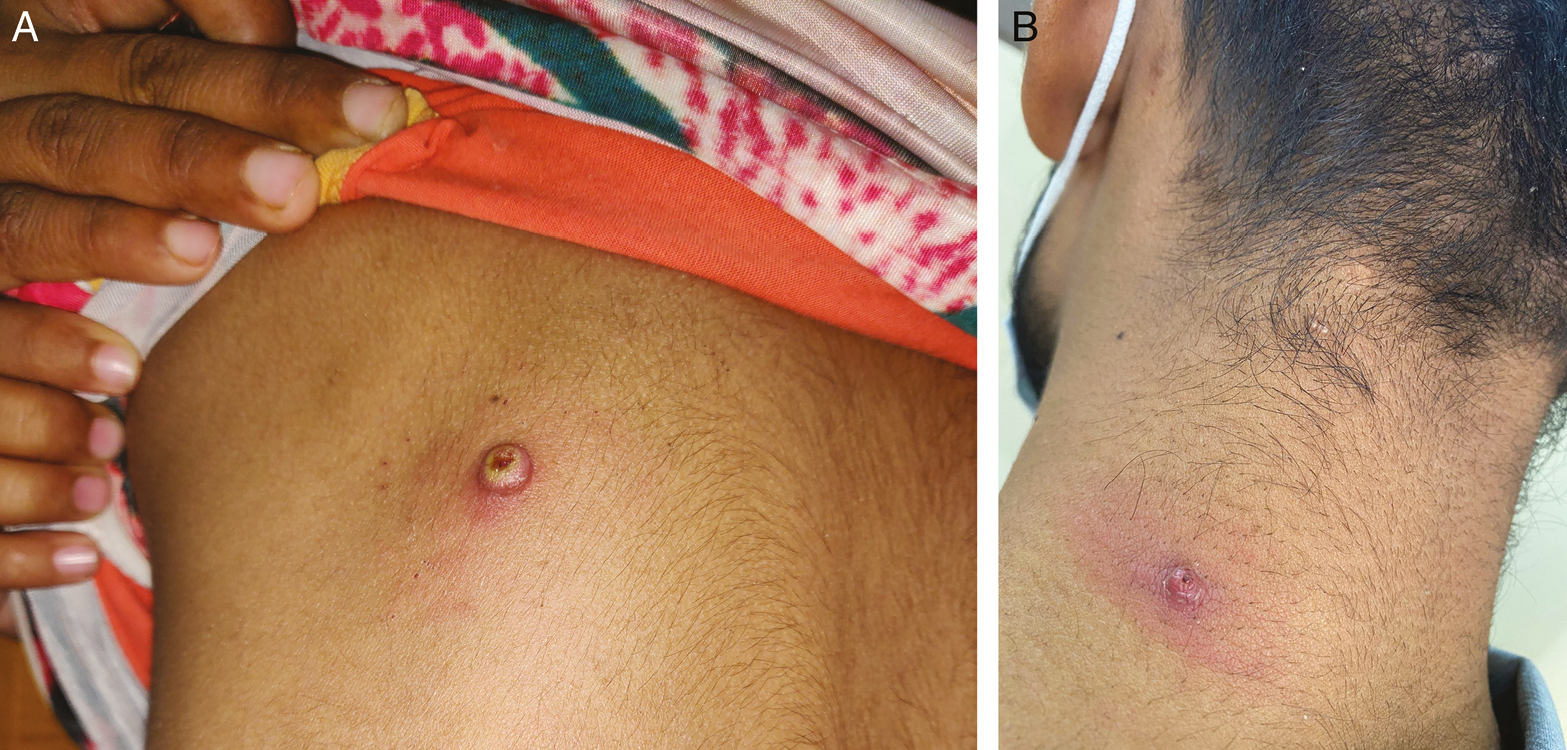
- (A) Secondary bacterial infection in MC, which was treated with 20% GA, and (B) allergic reaction to 30% SA in the lesion of MC
DISCUSSION
There are scarce data in the literature about the use of GA in the treatment of MC. A study conducted by Dave and Abdelmaksoud7 had treated nine patients (seven males and two females), with Fitzpatrick type III skin type, aged between 3 and 24 years with GA cream at two concentrations: 6% and 12%. On the other hand, in our study, 60 patients were treated with 20% GA applied weekly.
In Dave and Abdelmaksoud’s study, GA was applied by the patients or guardians at home, once/day at bedtime. They had instructed the patients to keep the topical formulation on lesions for the whole night for a maximum 3-month course or until the complete resolution of the lesions. On the other hand, in our study, the patient/relatives were instructed to apply medication once daily at night, for 1 h, over the lesions only. Although Dave and Abdelmaksoud had increased the frequency according to the tolerance, the degree of the initial response, and the anatomical location of the lesions, we kept our formulation’s concentration constant. Dave and Abdelmaksoud discontinued the application when the lesion showed erythema or crushing.
On the other hand, in our research, secondary bacterial infection (44.4%) was the most common side effect. Dave and Abdelmaksoud experienced an excellent response (the complete resolution of the lesions) to the treatment with no dropout in all patients within 4–12 weeks. However, they had a very small sample size and concluded that further studies, including a comparative study on a larger number of patients with different ethnic groups, are required to further validate the results. Our study overcame this limitation by recruiting children from diverse ethnicities with a larger sample size.
A study conducted by Ohkuma had compared the efficacy of 10% povidone-iodine paste against 50% SA paint for the management of molluscum. They had found both the modalities to be equally effective for MC.[8] But in our study, 30% of SA was used and 63.3% of patients had a complete clearance. Just like their study, even in our research, we found SA to have minimal adverse events.
Another such study carried out by Sau et al.[9] had compared the effectiveness of potassium hydroxide (KOH) versus SA for MC. According to them, KOH was superior to SA. Although Sau et al. had observed a complete clearance in 22.6% of patients after 8 weeks of management, in our study, 63% of patients had a complete clearance after 4 weeks of therapy. The concentration of SA used by them was 10%. Unlike them, the concentration of SA used by us was 30%, which could explain higher rates of response.
A similar study was conducted by Leslie et al.[10] to compare the topical SA against topical phenol in a placebo-controlled set-up. After 24 weeks of treatment, 87.5% treated with SA, 56.3% with phenol, and 59% treated with vehicle had a complete clearance. Unlike theirs, our study’s duration was only 4 weeks. However, our results were comparable with Leslie et al.’s. It could, therefore, suggest that even short-term SA therapy is at par with long-term SA therapy for effectively treating MC.
MC infection is thought to be more common in patients with eczema, which is supported by Leslie et al.’s observations. In their study, a large proportion of patients had a personal and family history of atopy. The atopic children also have a significantly greater number of MC lesions. Even in our research, we encountered 21% patients with atopic dermatitis.
Sau et al.9 had observed side effects in patients treated with SA including burning in 19.4%, redness in 14%, and desquamation in 19.3%. But in our study, in group B (treated with 30% SA), out of 60 patients, only 16 (26.6%) patients showed adverse events with secondary bacterial infection being the most common adverse reaction.
In our study, the duration and frequency of application of both the agents were kept constant as per the initial protocol, regardless of the site of involvement. However, if any of the patients experienced the clearance of MC before 4 weeks of treatment, the drug was withdrawn.
It is prudent to keep in mind that the application of GA and SA on facial or periorbital lesions, especially in younger children, can lead to postinflammatory hyperpigmentation or contact dermatitis. In fact, in our study as well, the most common site of postinflammatory hyperpigmentation was the face. However, none of our patients had periorbital MC.
Our study, however, had various limitations such as the development of pseudofrosting with SA, short treatment duration, and short follow-up period.
CONCLUSION
Both GA and SA have an excellent safety profile with minimal adverse events. Both the agents can effectively treat MC with just 1 month of therapy; however, SA has slightly superior results. We also noted a higher prevalence of MC in atopic patients and a higher degree of pseudokoebnerization in such cases. This observation is supported by the fact that because children affected with atopic dermatitis have a high tendency to scratch their skin, this repeated scratching could lead to the inoculation of MCV into previously unaffected skin. Thus, there is an obviously greater degree of pseudokoebnerization in such cases.
Our study’s statistical analysis, however, concluded that 30% SA has a slightly better efficacy and safety profile in comparison to 20% GA. However, we suggest both of these agents to be utilized as firstline agents among the available armamentarium for managing MC in pediatric patients.
Limitation
Pseudofrosting was noted with SA, which was cosmetically unacceptable by a few patients. Another limitation was a lack of histopathology correlation of clearance.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Molluscum contagiosum: An update and review of new perspectives in etiology, diagnosis, and treatment. Clin Cosmet Investig Dermatol. 2019;12:373-81.
- [Google Scholar]
- Epidemiology and impact of childhood molluscum contagiosum: A case series and critical review of the literature. Pediatr Dermatol. 2005;22:287-94.
- [Google Scholar]
- Dermoscopy of molluscum contagiosum: A useful tool for clinical diagnosis in adulthood. J Eur Acad Dermatol Venereol. 2006;20:482-3.
- [Google Scholar]
- Epidemiology and impact of childhood molluscum contagiosum: A case series and critical review of the literature. Pediatr Dermatol. 2005;22:287-94.
- [Google Scholar]
- A prospective randomized trial comparing the efficacy and adverse effects of four recognized treatments of molluscum contagiosum in children. Pediatr Dermatol. 2006;23:574-9.
- [Google Scholar]
- Glycolic acid cream for treatment of molluscum contagiosum. Dermatol Ther. 2018;31:e12630.
- [Google Scholar]
- Molluscum contagiosum treated with iodine solution and salicylic acid plaster. Int J Dermatol. 1990;29:443-5.
- [Google Scholar]
- Efficacy of 10% potassium hydroxide solution versus 10% salicylic acid ointment in treatment of molluscum contagiosum—The low-cost dermatologic therapy in Vietnam. Open Access Maced J Med Sci. 2019;7:269-71.
- [Google Scholar]
- Topical salicylic acid gel as a treatment for molluscum contagiosum in children. J Dermatolog Treat. 2005;16:336-40.
- [Google Scholar]






