Translate this page into:
A rare case of superficial vulvar angiomyxoma
*Corresponding author: Anushka Y. Mahadik, Department of Dermatology, Dr. D.Y. Patil Hospital School of Medicine, Nerul, Navi Mumbai, Maharashtra, India. anushkamahadik96@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharmila P, Nitin N, Mahadik AY, Parag C. A rare case of superficial vulvar angiomyxoma. J Cutan Aesthet Surg. doi: 10.4103/JCAS.JCAS_100_23
Abstract
Angiomyxoma is a rare, slow growing mesenchymal neoplasm that occurs almost exclusively in the genital, perineal and pelvic regions of adult women of reproductive age. We present the case of a 52-year-old female with an asymptomatic lesions over the vulva for 6 months which gradually increased in size. On examination a single, well circumscribed, erythematous to skin coloured, pedunculated mass was seen over the right side of the vulva measuring approximately 10 x 5cms. On palpation it was mobile, soft to firm in consistency with a smooth surface. Complete Excision under aseptic precaution was done and sent for histopathological examination which showed features suggestive of Angiomyxoma, a very rare gynecological tumor and classified as “tumors of uncertain differentiation “with estrogen and progesterone receptors. We present this case to highlight the importance of Histopathology in dermatology to diagnose rare cases and improve patient care.
Keywords
Angiomyxoma
Mesenchymal tumor
Vulvar tumor
INTRODUCTION
Angiomyxoma is a rare, slow growing mesenchymal neoplasm that occurs almost exclusively in the genital, perineal and pelvic regions of adult women of reproductive age. We present the case of a 52-year-old female with asymptomatic lesion over the vulva since 6 months which gradually increased in size.
CASE REPORT
A 52-year-old female presented to the dermatology department with complaints of a slow-growing mass over the right labia majora for 7 months. She presented due to the discomfort caused by the friction over the mass, which was otherwise asymptomatic. Initially, the lesion was small pea-sized. Local examination showed a well- circumscribed pedunculated polypoidal mass measuring 10 cm × 5 cm. The mass was nontender, soft in consistency. The overlying skin was smooth in texture and pink in color [Figure 1a].
The inguinal lymph nodes were not enlarged. A diagnosis of fibroepithelial polyp, a vulvar fibroma, or a giant acrochordon was considered. Local excision of the tumor with ligation of the stalk was done [Figure 1b].
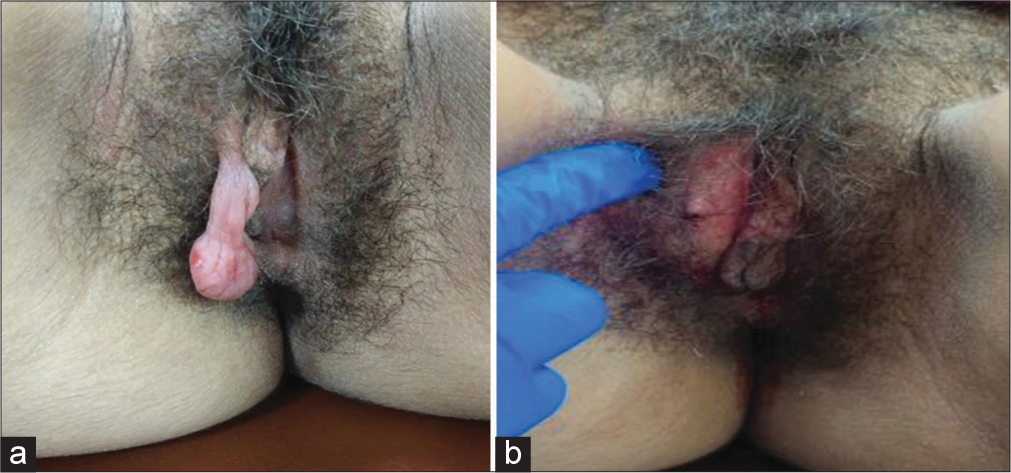
- (a) Pedunculated polypoidal mass over right labia majora (left) and (b) excision of tumor with stalk ligation (right).
The lesion was surgically removed and sent to the pathology department for histopathological examination. Hematoxylin–eosin staining revealed basketweave hyperkeratosis with acanthotic epidermis. Alternative hypocellular and hypercellular areas were seen in the dermis with myxoid matrix and fibrous ground substance along with thin-walled cystically dilated blood vessels and bland multinucleate cells seen [Figure 2]. On 1-year follow-up, there is no local recurrence noted.
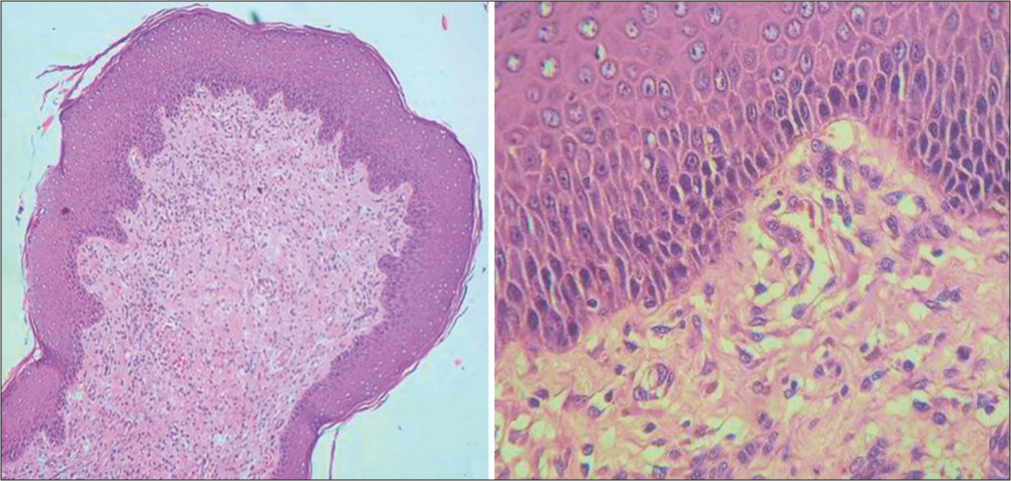
- (H and E) staining revealed basket weave hyperkeratosis with acanthotic epidermis. In dermis alternative hypo/hypercellular areas with myxoid matrix, fibrous ground substance, cystically dilated blood vessels (H and E, ×10—left, ×40—right) H &E: Hematoxylin–eosin.
DISCUSSION
Angiomyxomas are classified either as superficial (also called cutaneous myxoma) or aggressive. Superficial angiomyxomas are rare and usually present in middle-aged adults as a single nodule or a polypoidal lesion in the head and neck region that may be clinically confused with skin tag or neurofibroma. The stroma is made up of mostly edema with little myxoid material. On the other hand, aggressive angiomyxomas occur almost exclusively in the pelvic and perineal regions of women of reproductive age. “Aggressive” denotes its propensity for local aggression and recurrences after excision. Usually, this tumor is non metastasizing, but there are reports of multiple metastases in women treated initially by excision and who later succumbed to metastatic disease.1 This hormonally responsive tumor is believed to arise from specialized mesenchymal cells of the pelvic–perineal region or from the multipotent perivascular progenitor cells, which often display variable myofibroblastic and fibroblastic features. Vulvar Angiomyxoma may be clinically misdiagnosed as Bartholin cyst, Lipoma, Labial cyst, Gartner duct cyst, Levator hernia or Sarcoma. Fibroepithelial stromal polyp, superficial angiomyxoma, AMFB, cellular angiofibroma, and smooth muscle tumors also need to be considered in the differential diagnoses of a polypoidal mass in the perineum.2
Late age of onset (postmenopausal), size greater than 5 cm, onset less than a year, and on pathology presence of myxoid matrix, small to medium-sized vessels, mostly thick-walled or hyalinized with low cellularity and no signs of infiltration, metastasis, and local recurrence on follow-up after 1 year are what differentiates superficial angiomyxomas from aggressive angiomyxomas, and AMFB is a benign mesenchymal tumor most commonly found in the female genital tract of premenopausal women.3
Wide surgical excision is the traditional treatment of choice.
CONCLUSION
The case highlights the importance of Histopathology in dermatology to diagnose rare cases and improve patient care.
Authors’ Contributions
All the authors contributed to the research study. Patil Sharmila, Nadkarni Nitin, Anushka Y. Mahadik: Concepts, Design, Definition of Intellectual Content, Literature search, Clinical Studies, Manuscript preparation, Manuscript review, Manuscript editing and Guarantor. Chaudhari Parag: Concepts, Design, Definition of Intellectual Content, Literature search, Clinical Studies, Manuscript preparation, Manuscript review, Manuscript editing.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Aggressive angiomyxoma of the vulva: An uncommon entity. Indian Dermatol Online J. 2012;3:128-30.
- [Google Scholar]
- Pedunculated angiomyxofibroma of vulva: A rare entity case report. J Genit Syst Disor. 2014;3:1.
- [Google Scholar]
- Vaginal angiomyofibroblastoma: A case report and review of diagnostic imaging. Case Rep Obstet Gynecol. 2018;2018:7397121.
- [Google Scholar]






