Translate this page into:
A split-face study comparing the efficacy and tolerability of erbium YAG laser and 70% trichloroacetic acid in facial seborrheic keratosis
Address for correspondence: Dr. Aakanksha Arora, Department of Dermatology, Venereology and Leprology, Sardar Patel Medical College, Bikaner 334001, Rajasthan, India. E-mail: akarora357@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Introduction:
Seborrheic keratosis (SK) are benign lesions with cosmetic concerns. Role of TCA and erbium YAG laser has already been described individually in the literature. However, there is a scarcity of data on the comparative evaluation of these two modalities in SK.
Aim:
The aim of this study was to compare the efficacy and safety profile of Erbium YAG laser ablation with 70% TCA for the treatment of facial SK.
Materials and Methods:
A total of 50 cases of facial SK were included in the study. Group A included SK lesions on the right side of face treated with Erbium YAG laser ablation while Group B included SK lesions on the left side of face treated with topical 70% trichloroacetic acid. Repeated sessions of laser and TCA application were given at 2-week intervals till cure was achieved or up to a maximum of three sessions. Grading of response to treatment was assessed as complete response (100% clearance), partial response (>50 to 99% improvement), and inadequate or no response (<50% improvement).
Results:
Complete clearance was observed in 40 (80%) and 29 (58%) cases in Groups A and B, respectively. There was a statistically significant difference in clearance rates between the two groups (P = 0.019). Number of sessions was significantly lesser in laser group (mean ± SD = 1.24 ± 0.43) than in the 70% TCA group (mean ± SD = 1.88 ± 0.79) (P = 0.001). Statistically significant lesser downtime was observed in group A (P = 0.001). Patient satisfaction rate was much higher in group A. Hyperpigmentation was more common in group B (TCA).
Conclusion:
Although both the treatment modalities achieved good results, erbium YAG laser ablation showed superior results than 70% TCA with better patient satisfaction rates but more downtime. Also, no major adverse effects were observed in the two groups.
Keywords
Erbium YAG laser
seborrheic keratosis
trichloroacetic acid
INTRODUCTION
Seborrheic keratoses (SKs) are commonly encountered benign epidermal tumors characterized by proliferation of immature keratinocytes. These typically appear as well-demarcated, skin colored to brown or black colored, slightly elevated papules or plaques. The common site of involvement is usually the trunk, specifically the back, neck, arm, and face.[1] Facial involvement is often associated with cosmetic concerns in patients. The choice of treatment depends on the number, location, thickness of lesions, and overall aesthetic considerations.[12]
The aim of this study was to compare the efficacy and safety profile of Erbium YAG laser ablation with 70% trichloroacetic acid (TCA) for the treatment of facial SK.
MATERIALS AND METHODS
A total of 50 cases of facial SK were included in this single-center, evaluator-blinded, prospective, intra-individual split-face comparative study. The study was conducted in the dermatology department of tertiary care center over a period of 6 months. A formal ethical committee approval and informed consent from patients was taken. Patients above 18 years of age with lesions of SK of similar size, thickness, and type on both sides of face and without any history of concurrent or past treatment were included in the study. Exclusion criteria were active pregnancy and lactation, clinical lesions suspicious of malignancy (atypical, rapidly growing or eruptive SK lesions), history of oral or topical retinoid use in past 1 month, active skin infections at the site of lesion, bleeding disorders, history of keloid or hypertrophic scar formation, recurrent herpes simplex infection, connective tissue disease and those who were not willing or available for a follow-up period of at least 3 months. To be considered eligible, a patient had to have SKs of similar size and thickness on both sides of the face. Two groups were formed by matching four similar lesions on each side of face in the patients. A maximum of four pairs of SK lesions on each patient were allowed in the study. The response was assessed based on the improvement in these four pairs of SK. Group A included SK lesions on the right side of face treated with Erbium YAG laser ablation while Group B included SK lesions on the left side of face treated with topical 70% TCA.
In group A, patients were subjected to erbium YAG laser with wavelength 2,940 nm, short pulse, fluence ranging from 4 to 8 J/cm2, 3 Hz, spot size of 5–9 mm, and multiple passes according to lesion size and thickness. End point of treatment was determined either by the ablation of the lesion or by the appearance of pinpoint bleeding [Figure 1A]. Subsequent sessions of laser ablation were given at 2 weeks of intervals till the removal of any residual tissue or to a maximum of three sessions. In Group B, cotton tipped applicator was moistened with 70% TCA & applied to the lesion. The area surrounding the lesion was protected with petroleum jelly before TCA application. The endpoint was solid frosting [Figure 1B]. Repeated sessions of TCA application were given at 2 weeks of intervals till cure was achieved or up to a maximum of three sessions. Evaluation criteria included an overall lesion improvement in terms of lesion pigmentation, texture, and thickness, score ranged from zero (unchanged) to 100% (normal-appearing skin) as assessed by same independent dermatologist at baseline and after treatment. Grading of response to treatment was assessed as complete response (100% clearance of lesion), partial response (>50%–99% improvement in lesion characteristics), and inadequate or no response (<50% improvement).
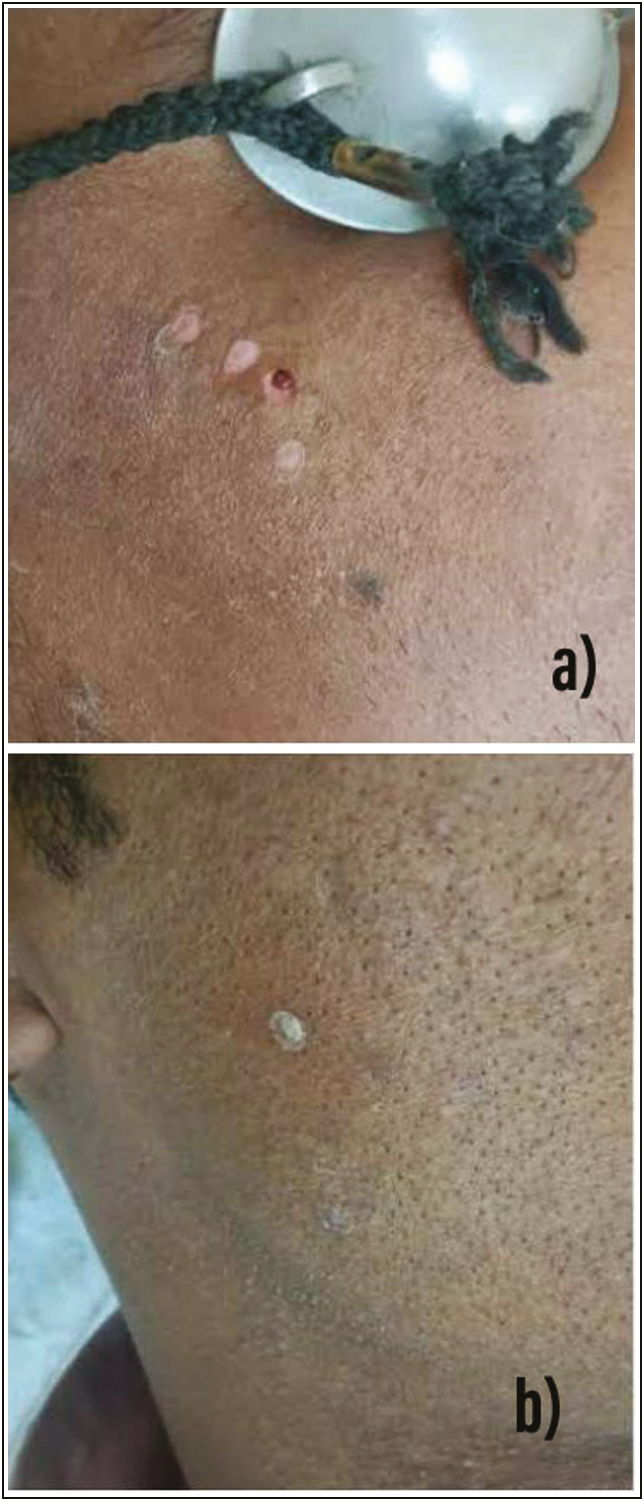
- (A) Pinpoint bleeding as clinical end point of erbium YAG laser ablation. (B) Solid frosting as clinical end point of TCA application
Patient satisfaction was measured at three months following the completion of the treatment using a three-point scale (one = minimally satisfied, two = mostly satisfied, three = completely satisfied).
Statistical analysis was done using unpaired t test and chi-square test. P Values less than 0.05 were considered significant.
RESULTS
Out of 50 patients, 27 patients were male and 23 were female. The age ranged from 24 to 73 years. The mean age of patients was 45.14 years. Duration of lesion varied from 1 month to 8 years.
In group A (Erbium YAG laser ablation on the right side), 40 (80%) patients showed complete clearance, 8 (16%) showed partial clearance and 2 (4%) showed inadequate or no response. Similarly, in group B (70% TCA on left side), 29 (58%) cases showed complete clearance, 12 (24%) showed partial clearance and 10 (20%) showed inadequate or no response. Thus, there was a statistically significant difference in clearance rates between the two groups (P = 0.019) with more significant results on right side of face with erbium YAG laser ablation [Figure 2]. There was no significant correlation between the lesion duration and the improvement rate of lesions in both groups (P > 0.05).
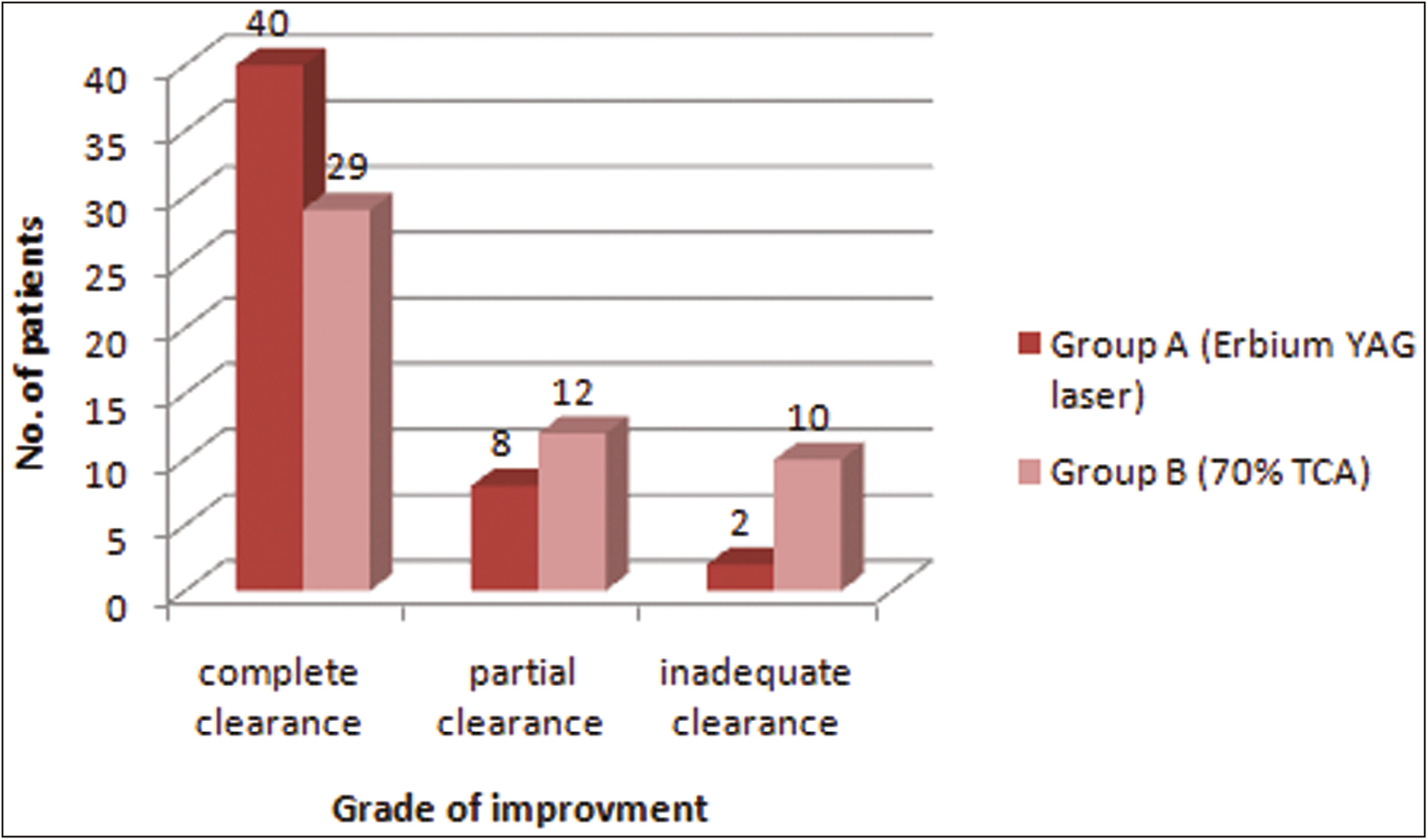
- Graphical representation of comparison of grade of improvement using erbium laser ablation and 70% TCA application in Seborrheic keratosis
Number of sessions was significantly lesser in the laser group (mean ± SD = 1.24 ± 0.43) than in 70% TCA group (mean ± SD = 1.88 ± 0.79) (P = 0.012). The downtime was 10.24 ± 1.48 days and 7.98 ± 1.25 days in Goups A and B, respectively. Statistically significant lesser downtime was observed in group B (P = 0.001).
The post-treatment side effects in group A were erythema in 23 cases (46%), post-inflammatory hyperpigmentation in 4 cases (8%), and mild scar formation in 7 cases (14%). The major side effects noted in group B were burning sensation and erythema in 18 (36%) cases. None of the patients reported erosion and scarring. However, post-inflammatory hyperpigmentation was noted in 12 (24%) patients [Figure 3]. There was no statistically significant difference in adverse effects of both groups (P = 0.41).
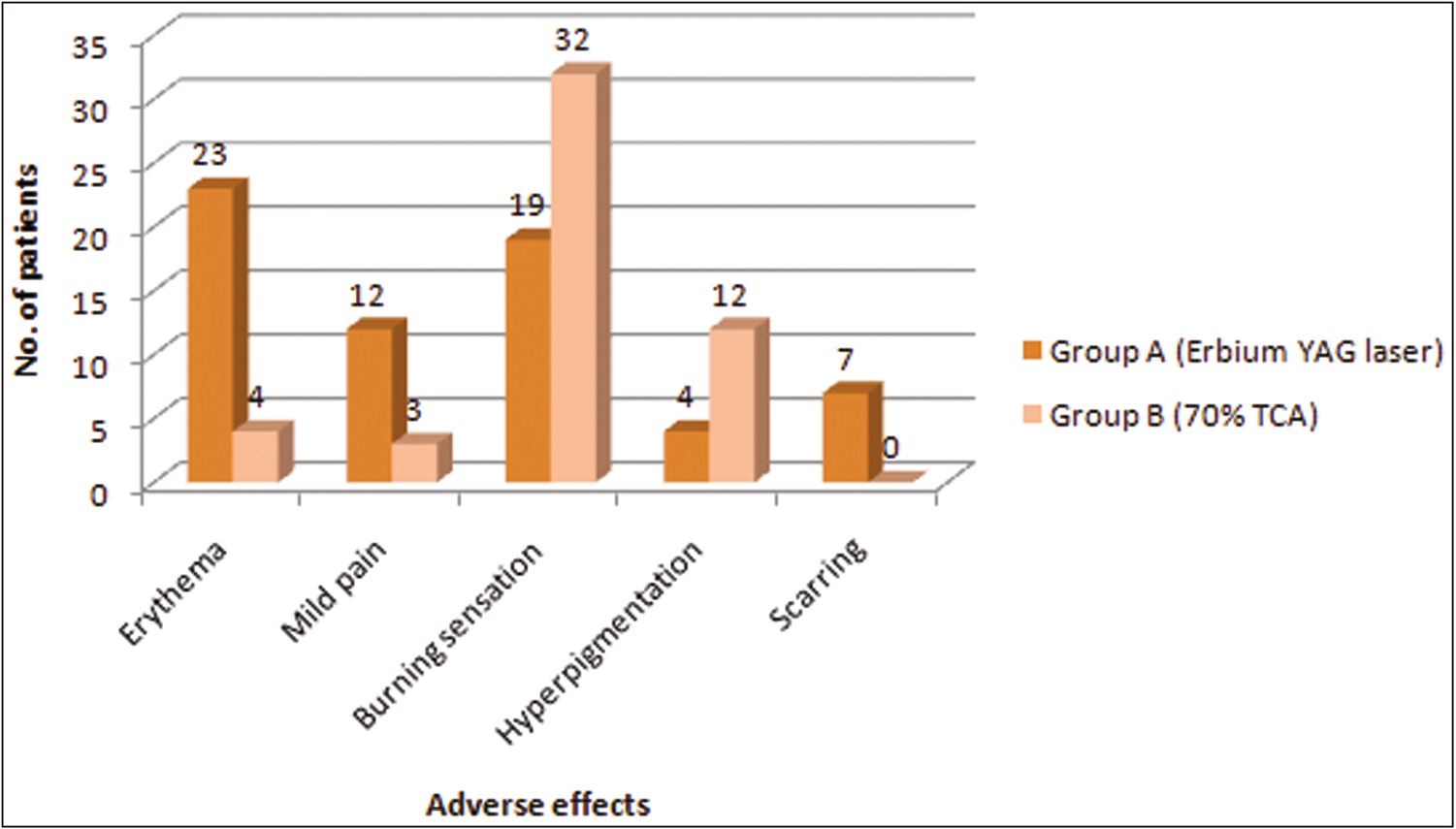
- Graphical representation of comparison of adverse effects using erbium laser ablation and 70% TCA application in Seborrheic keratosis
In group A, 32 patients (64%) were completely satisfied, followed by 11 patients (22%) who were mostly satisfied and 7 patients (14%) who were minimally satisfied. In group B, 25 patients (50%) were completely satisfied, followed by 14 patients (28%) who were mostly satisfied and 11 patients (22%) who were minimally satisfied. Thus, the patient satisfaction rate was much higher in group A, however, statistically insignificant (P = 0.3).
DISCUSSION
SK are benign lesions with cosmetic concerns. Many modalities like shave or surgical excision, curettage, cryosurgery, electrosurgery, ablative lasers like CO2 and erbium YAG laser, chemical ablation with trichloroacetic acid, and hydrogen peroxide have been proposed. Radiofrequency ablation is a commonly performed procedure for the management of SK. This is typically performed multiple times to ensure the adequate removal of the affected tissue. Electrodessication and electrofulguration provide efficient results. However, possible complications include infection, scarring, and hyperpigmentation. Still, there is paucity of literature on the uniform guidelines to treat SK, especially on aesthetically important areas like face.[34] Role of TCA and erbium YAG laser has already been described individually in the literature. However, there is a scarcity of data on the comparative evaluation of these two modalities in SK.
Thus, we evaluated the effectiveness of erbium YAG laser ablation and chemical ablation with 70% TCA in facial SK in the same individual by conducting a split face study.
Role of laser ablation and chemical ablation using TCA has already been described in the literature individually. Gruel et al.. conducted a study comparing the effectiveness of erbium:YAG laser and cryosurgery in seborrheic keratoses and observed complete healing in all of the lesions treated with Er:YAG lasers, while 68% of lesions healed in the cryotherapy group.[5] Similarly, in our study, 80% of cases showed complete clearance by erbium YAG laser ablation [Figure 4A and 5A].
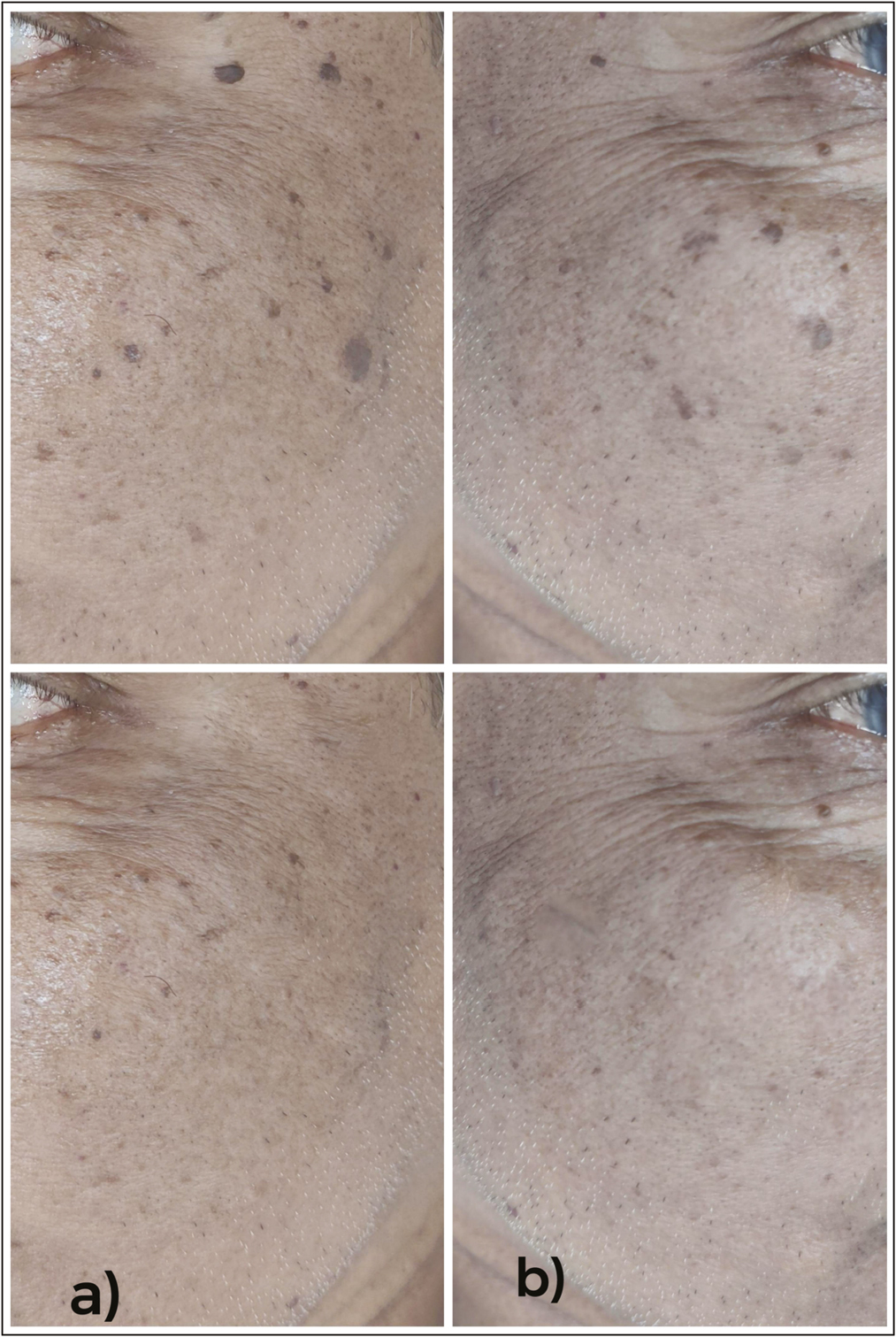
- (A) Pre- and posttreatment images of patient with seborrheic keratosis after treatment with Erbium YAG laser showing complete clearance without any adverse effects. (B) Pre- and posttreatment images of patient with seborrheic keratosis after treatment with 70% TCA showing complete clearance without any adverse effects
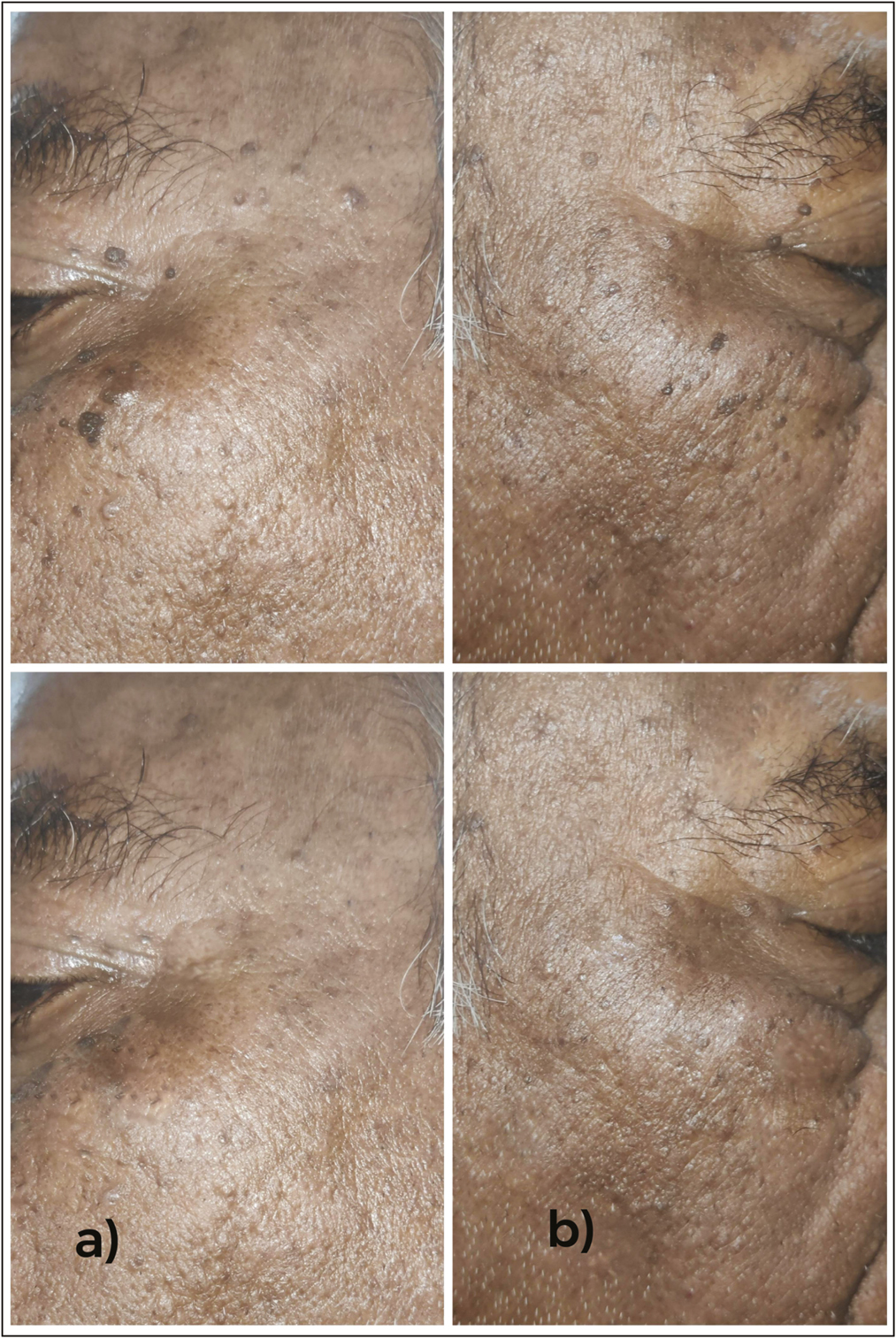
- (A) Pre- and posttreatment images of patient with seborrheic keratosis after treatment with Erbium YAG laser showing complete clearance without any adverse effects. (B) Pre- and posttreatment images of patient with seborrheic keratosis after treatment with 70% TCA showing complete clearance without any adverse effects
Chun et al. evaluated the clinical effects of focal TCA peel on pigmented lesions in dark-skinned patients. SK was treated with 65% focal TCA peel and 19 of 23 (83%) patients experienced a good clinical response and high satisfaction rates with no significant complications.[6] In the present study, 58% and 12% of cases showed complete and partial response, respectively [Figure 4B and 5B]. Post-inflammatory hyperpigmentation was one of the most significant adverse effects observed.
Our study also demonstrated that the number of sessions was significantly lesser for laser group. However, the downtime was much higher in the laser group as compared to TCA.
The erbium: YAG laser offers an advantage of lesser residual thermal damage of less than about 50 µm with a penetration depth of 10 to 30µm despite multiple passes. Role of erbium YAG laser in SK is attributed to the extription of epidermis layer by layer with minimum collateral damage resulting in precise ablation with remarkable depth control.[7-9] This provides favorable cosmetic results specifically in delicate areas specifically pertaining to lesser rate of hyperpigmentation. However, scarring have been reported in few cases owing to repeated irradiation of tissue at the same site by the laser.[10] In the present study, erythema and pain were most commonly reported minor side effects in both the groups. However, scarring and post-therapy hyperpigmentation were cosmetically significant adverse effects observed in Groups A and B, respectively [Figure 6A and B]. Gruel et al.[5] reported erythema as major side effect in the Er:YAG laser-treated cases of SK with significantly lesser hyperpigmentation than in the cryotherapy group.

- (A) Pre- and post-treatment images of patient with seborrheic keratosis showing scarring after treatment with erbium YAG laser. (B) Pre- and posttreatment images of patient with seborrheic keratosis after treatment with TCA 70% showing partial response and post inflammatory hyperpigmentation
Although both treatment modalities achieved good results, erbium YAG laser ablation was better than TCA 70% with better patient satisfaction rates but more downtime. However, erbium YAG lasers may not be available at all centers while TCA is an easily available option.[1112] No study has yet been conducted doing a head to head comparison between chemical ablation (TCA) and laser ablation in facial SK using a split face study design. Since, there are currently no standardized guidelines for the treatment of SK, new treatment modalities are being tested. The present study is first of its kind to compare erbium YAG laser and 70% TCA in SK.
CONCLUSION
Although both treatment modalities achieved good results, erbium YAG laser ablation showed superior results than 70% TCA with better patient satisfaction rates but more downtime. Scarring and post-inflammatory hyperpigmentation were the two cosmetically significant adverse effects observed in laser and 70% TCA group, respectively. Thus, Er:YAG is a one-step procedure for SK in patients with high cosmetic expectations. However, the easy accessibility and cost-effectiveness of TCA are few advantages over erbium YAG laser.
Declaration of patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Current understanding of seborrheic keratosis: Prevalence, etiology, clinical presentation, diagnosis, and management. J Drugs Dermatol. 2015;14:1119-25.
- [Google Scholar]
- Seborrheic keratoses: A study comparing the standard cryosurgery with topical calcipotriene, topical tazarotene, and topical imiquimod. Int J Dermatol. 2004;43:300-2.
- [Google Scholar]
- Efficacy and safety of topical treatments for seborrheic keratoses: A systematic review. J Dermatolog Treat. 2022;34:1-12.
- [Google Scholar]
- Effectiveness of cryosurgery vs curettage in the treatment of seborrheic keratoses. JAMA Dermatol. 2013;149:108-9.
- [Google Scholar]
- Effectiveness of erbium:YAG laser and cryosurgery in seborrheic keratoses: Randomized, prospective intraindividual comparison study. J Dermatolog Treat. 2015;26:477-80.
- [Google Scholar]
- Focal trichloroacetic acid peel method for benign pigmented lesions in dark-skinned patients. Dermatol Surg. 2004;30:512-6; discussion 516.
- [Google Scholar]
- Efficacy and safety of cryotherapy, electrodesiccation, CO2 laser, and Er:YAG laser in the treatment of seborrheic keratosis. Dermatol Ther. 2021;34:e15083.
- [Google Scholar]
- 2940-nm erbium:YAG laser versus 980-nm diode laser in the treatment of multiple seborrheic keratoses: A prospective comparative randomized study. J Cosmet Dermatol. 2022;21:5628-35.
- [Google Scholar]
- Ablation of cutaneous lesions using an erbium:YAG laser. J Cosmet Laser Ther. 2003;5:150-3.
- [Google Scholar]
- Is topical 70% Trichloroacetic acid effective in treating patients with seborrhoeic keratosis? Int J Res Health Allied Sci. 2019;5:112-4.
- [Google Scholar]
- Topical trichloroacetic acid versus cryotherapy in the treatment of seborrheic keratoses: A prospective comparative study. J Pak Assoc Dermatol. 2022;32:1-8.
- [Google Scholar]






