Translate this page into:
A Translucent Yellow-brown Papule on the Nose
Address for correspondence: Prof. Dr. Arun C. Inamadar, Department of Dermatology, Venereology and Leprosy, Shri B. M. Patil Medical College, Hospital and Research Center, BLDE (Deemed to be University), Vijayapur 586103, Karnataka, India. E-mail: aruninamadar@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
The adult counterpart of juvenile xanthogranuloma is a relatively uncommon and although benign, the condition is not self-regressing as the juvenile form. Hence, surgical management becomes necessary. Herein we describe the characteristic clinical, dermoscopic and histological features of a solitary xanthogranuloma in a 35 year old male that was effectively managed surgically and present to the readers as a quiz.
Keywords
Dermoscopy
Touton giant cells
xanthogranuloma
Case Report
A 35-year-old man presented with a 6-month-old asymptomatic lesion on his nose. Examination revealed a solitary, circumscribed, dome-shaped papule, measuring 5 × 5 mm, with a brownish-yellow tinge, prominent blood vessels, and a smooth translucent surface situated near the bridge of the nose [Figure 1A]. Non-contact dermoscopy using DermLite DL3 (3Gen, San Juan Capistrano, California, USA) under polarized mode revealed yellowish-orange areas, brown structureless areas, dilated vessels in linear and branching patterns extending from the margin towards the center, a peripheral faint erythematous border, and a superficial minimal white scaling [Figure 1B]. The lesion was completely excised under local anesthesia with a horizontal elliptical incision, and the wound was closed primarily with a 6-0 non-absorbable suture [Figure 2]. Histopathological analysis of the lesion revealed an attenuated epidermis and a dense diffuse dermal infiltrate of mononuclear cells [Figure 3A] with some of them showing foamy change [Figure 3B]. Touton giant cells were observed interspersed with the mononuclear cells [Figure 3B].
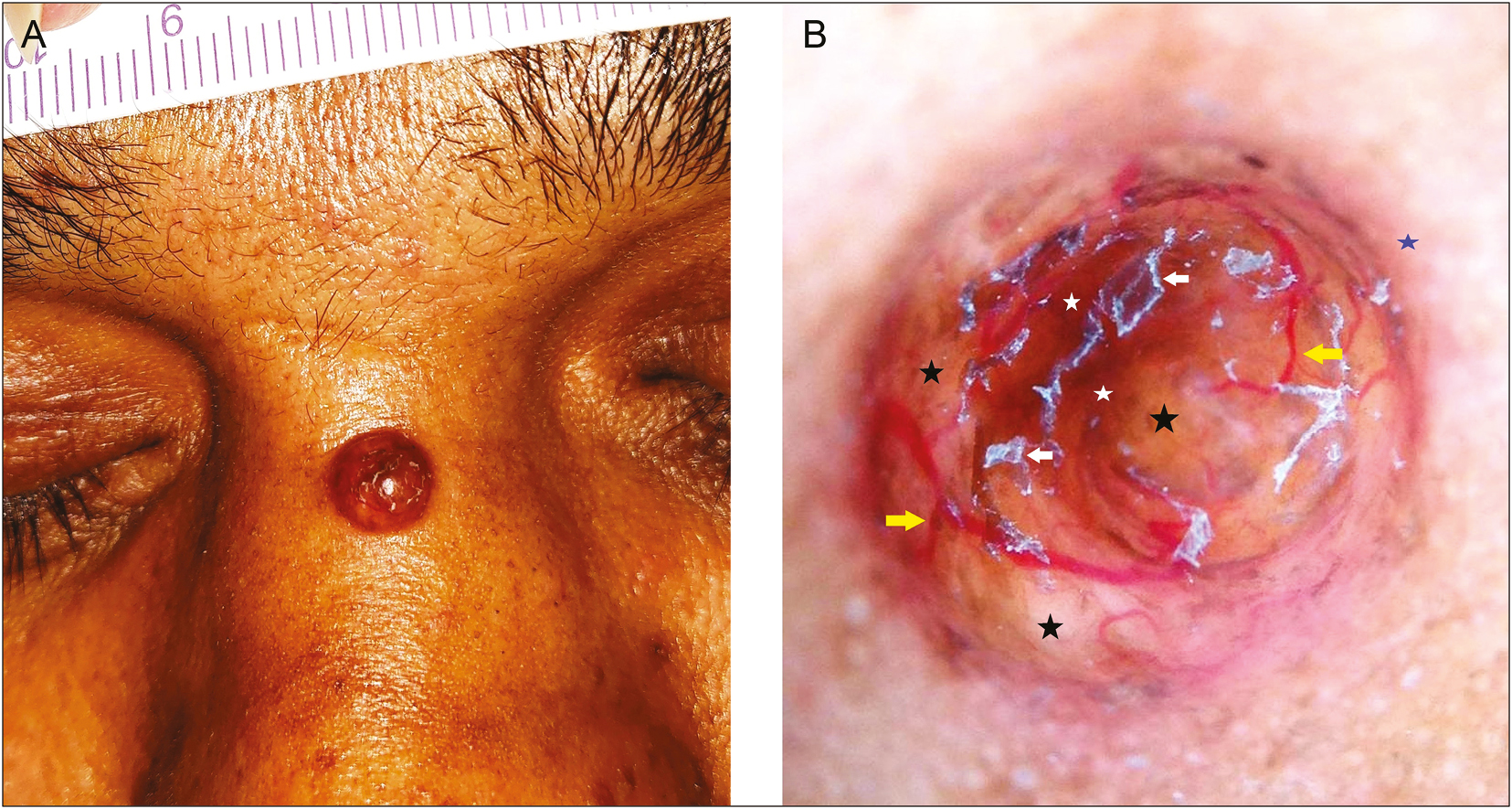
- A well-circumscribed dome-shaped yellow-brown translucent papule near the bridge of the nose (A). Non-contract dermoscopy under polarized mode reveals yellowish-orange areas (black stars), brown structureless areas (white stars), dilated linear and branching vessels extending from the margin towards the center (yellow arrows), a faint erythematous border (blue star), and superficial white scales (white arrows) (B) (original magnification, ×10)
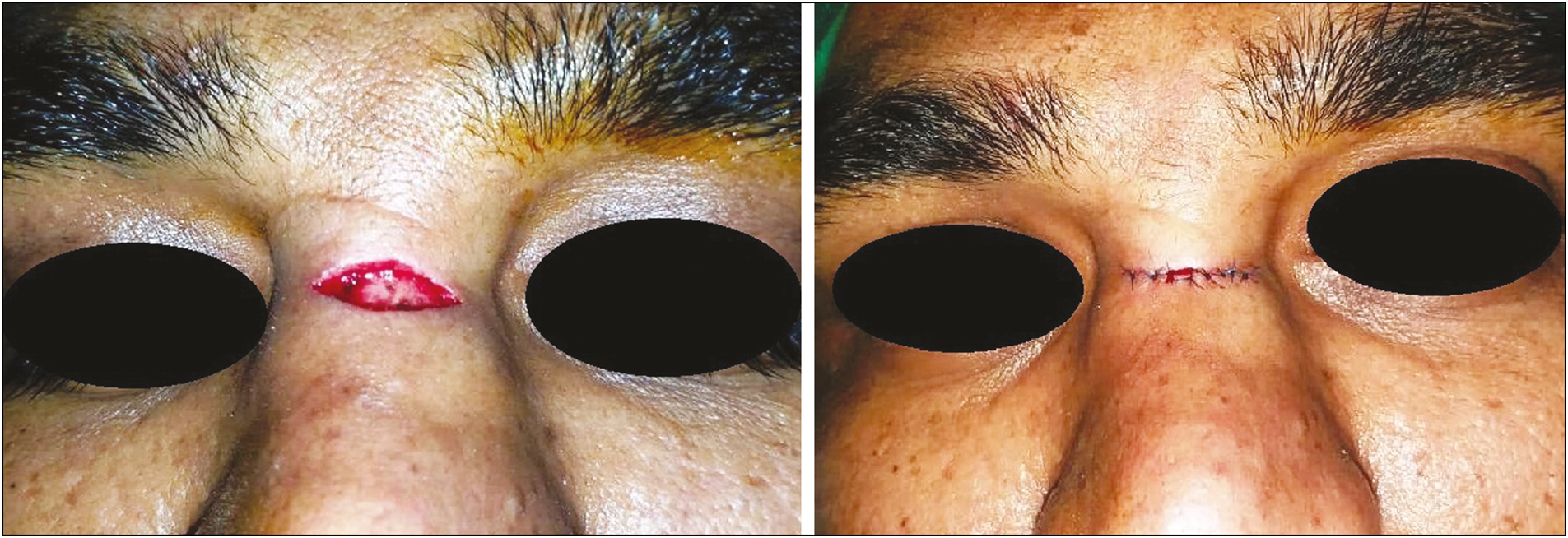
- Lesion was excised with a horizontal elliptical incision (left) with primary closure of the wound (right)
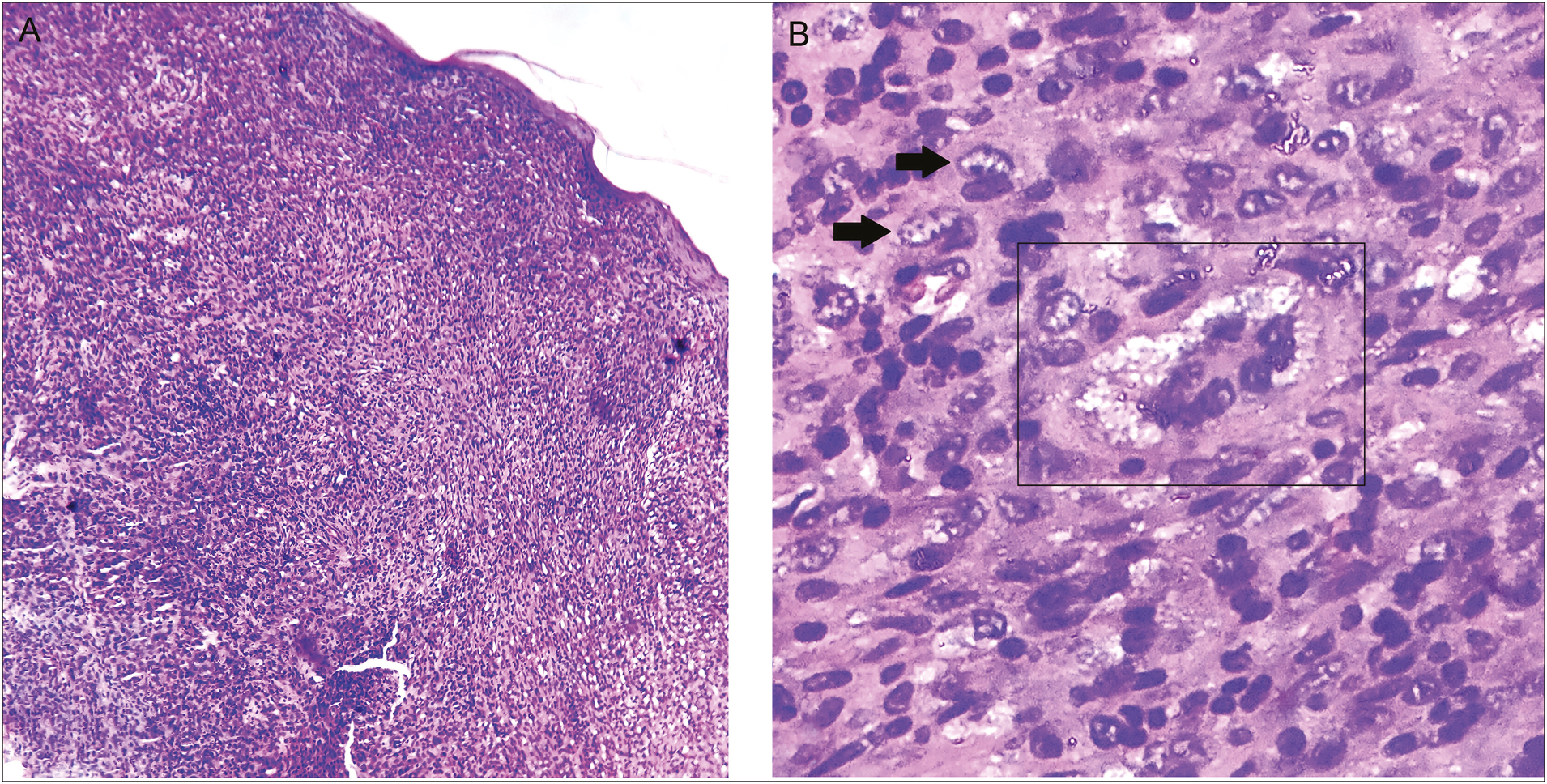
- Photomicrograph showing a diffuse and dense dermal mononuclear infiltrate with an overlying attenuated epidermis (A) (H-E, original magnification, x10). Higher magnification showing xanthomatized cells (black arrows) and Touton giant cell (black rectangle) (B) (H–E, original magnification ×40)
Question
What is your diagnosis?
Answer
Xanthogranuloma.
Discussion
Xanthogranuloma is the most common form of the non-Langerhans cell histiocytoses. It is commonly known as juvenile xanthogranuloma as the disorder is frequent in children, with 70% of the lesions diagnosed within the first year of life and approximately 35% of the cases being congenital. Late-onset lesions in adolescents and adults account for around 10%–30% of the cases and are designated as xanthogranuloma or adult xanthogranuloma. The juvenile form shows a male preponderance, whereas the sex distribution is equal in the late-onset form.[12]
Clinically, the lesions are either solitary or multiple, asymptomatic, circumscribed firm to rubbery papules, and nodules measuring 5–10 mm in diameter. Initial lesions are yellowish-orange in appearance and develop a tan to brown tinge as they age. The head and neck region is frequently involved, followed by the trunk and proximal extremities. As opposed to the self-regressing nature of the juvenile xanthogranuloma, the lesions in adults are persistent. Atypical clinical forms (hyperkeratotic nodules, plaques, grouped, and linear lesions) as well as involvement of atypical sites (palms, soles, digits, and genitalia) have also been described. Extracutaneous lesions account for an overall 5%–10% of the cases and are also known to regress spontaneously. Eyes, lungs, liver, and the testes are the frequent extracutaneous sites affected, and others such as the central nervous system, spleen, and the retroperitoneum may be rarely affected as well. The juvenile form is known to be associated with neurofibromatosis, juvenile myelomonocytic leukemia, and other hematological malignancies.[12]
Histologically, xanthogranulomas are characterized by an ill-defined nodular dense dermal infiltrate of polygonal or spindle-shaped plump histiocytes. Established lesions show prominent xanthomatization of the cells along with a varying numbers of Touton giant cells. Lymphocytes, neutrophils, and plasma cells are also found interspersed with the histiocytes, and the older lesions show interstitial fibrosis and fibroblast proliferation. The aforementioned dermoscopic features in our case are classical of xanthogranuloma with the yellowish areas corresponding to the xanthomatized nodular aggregates of histiocytes in the dermis. Immunohistochemically, the cells stain positively with factor XIIIa, HAM-56, HHF35, cathepsin B, vimentin, fascin, MS-1, and CD68, but not with CD1a and S-100.[12]
The clinical differentials include benign cephalic histiocytosis and papular xanthomata when lesions are multiple, and the solitary lesions need to be differentiated most commonly from mastocytoma and Spitz nevus in children.[1] The management in juvenile forms includes evaluation for visceral involvement or any associations. In purely cutaneous forms, observation is recommended as spontaneous regression generally occurs in 5–6 years. Localized cutaneous lesions in adults, which tend to be persistent can be managed surgically.[1]
As the lesion in our case showed a yellowish tinge with prominent blood vessels, xanthogranuloma or a benign sebaceous tumor was considered as differential diagnoses before performing dermoscopy. The features revealed by dermoscopy were reasonably characteristic of xanthogranuloma, especially in the context of the clinical picture, and the lesion was managed as described above. Histopathological analysis of the excised specimen further confirmed the clinico-dermoscopic diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Macrophage/monocyte disorders. In: James WD, Berger TG, Elston DM, Neuhaus IM, eds. Andrews’ diseases of the skin clinical dermatology (12th ed.). Philadelphia, PA: Elsevier Saunders; 2016. p. :699-725.
- [Google Scholar]
- Cutaneous infiltrates—non-lymphoid. In: Weedon D, ed. Weedon’s skin pathology (3rd ed.). Edinburgh, Scotland: Churchil Livingstone Elsevier; 2010. p. :937-70.
- [Google Scholar]






