Translate this page into:
Acne scars impact on the quality of life and the willingness to pay for treatments among adults in Riyadh, Saudi Arabia: A cross-sectional study
*Corresponding author: Khalid Alosaimi, College of Medicine, King Saud University, Riyadh, Saudi Arabia. alosaimi.kr@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Alkeraye S, Alosaimi K, Alrabiah HF, Alkahtani R, Alshehri NA, Alharbi BA. Acne scars impact on the quality of life and the willingness to pay for treatments among adults in Riyadh, Saudi Arabia: A cross-sectional study. J Cutan Aesthet Surg. 2024;17:205-13. doi: 10.25259/jcas_154_23
Abstract
Objectives:
Acne scarring occurs from skin damage following acne healing. Treatments such as chemical peels, dermabrasion, and laser therapy can effectively enhance scars’ appearance but could be expensive. This study aimed to reflect participants’ awareness of treatment options and their willingness to pay (WTP), evaluating their association with sociodemographics, severity, and quality of life (QoL).
Material and Methods:
A cross-sectional study was conducted in Riyadh, Saudi Arabia, from June to July of 2023. Study participants were chosen using a non-probability sampling technique. Participants were aged 18 or older, had acne scarring, and resided in Riyadh. Data analysis was performed using RStudio, with P < 0.05 indicating statistical significance.
Results:
A total of 401 adult participants were included in the study. The prevalence of acne scarring among the participants was 63.4%. About 45.8% of the participants expressed a WTP of <1000 Saudi Riyals (SAR), while 42.2% were willing to pay 1000–6000 SAR. The most well-recognized acne scar management modalities were laser resurfacing (66.3%) and chemical peels (64.1%), while the least recognized were collagen/fat filler injections (23.9%) and radiofrequency microneedling (27.7%).
Conclusion:
The most recognized acne scar treatment modalities were laser resurfacing and chemical peels. Participants were willing to pay for reasons such as psychological impact, income levels, and awareness of treatment modalities. The findings could influence dermatologists to start awareness campaigns to debunk misconceptions about acne scar treatment modalities and their efficacy in improving QoL.
Keywords
Acne scars
Quality of life
Willingness to pay
Saudi Arabia
INTRODUCTION
Acne vulgaris is a long-lasting inflammatory condition of the pilosebaceous unit of the skin brought on by androgen-induced increased sebum production, altered keratinization, inflammation, and Cutibacterium acnes bacterial colonization, and characterized by open and closed comedones. Furthermore, papules, pustules, and nodules can be present. The face, neck, chest, and back are the most commonly affected areas.1,2
Acne vulgaris is considered the eighth most frequent condition globally and is one of the most prevalent skin disorders.3 Adolescents typically experience peak incidence between 14 and 19.4 The prevalence of acne vulgaris in Saudi Arabia is high, sitting at a percentage of 78% of adolescents between 15 and 30 years old.5
Although not life-threatening, acne has psychological effects. Even though active acne might only last several years, acne scars can last a lifetime, predisposing patients to depression, and anxiety.6,7
According to research done in the US, the yearly direct and indirect cost of management is more than $3 billion.8
Scars are skin lesions formed after healed traumas or inflammation, such as a sequela of acne.9,10 Depending on whether there is a net loss or growth of collagen, there are two fundamental types of scars (atrophic and hypertrophic scars, respectively). The scars can also be post-inflammatory macules, erythematous, hyperpigmented, or hypopigmented.9,10
Prevention is the best way to avoid post-acne scars; however, numerous effective procedures can be used to treat atrophic scars, most notably chemical peels, laser therapy, radiofrequency microneedling, subcision, filler injections, and microneedling.10,11
Although there are compelling and well-documented treatments for acne scars, our literature review could not appreciate Saudi patients’ knowledge, perception, and willingness to pay (WTP) for acne scar treatments. The objective of this study is to reflect acne scarring patients’ awareness of treatment options and their WTP for treatments also to evaluate the WTP’s association with patients’ sociodemographics, scar severity, and effect on the quality of life (QoL).
MATERIAL AND METHODS
Study design
This cross-sectional study was conducted in Riyadh, Saudi Arabia, from June to July of 2023. Approximately 8,591,748 people are living in the capital of Saudi Arabia, Riyadh, according to the most recent summary statistics report from the Saudi Census.12 Riyadh was chosen as the research location due to its representativeness of the target demographic. The study participants were chosen using a non-probability sampling technique. The technique was implemented for its feasibility and accessibility to potential participants. Furthermore, when considering that the majority of patients with acne scars seek private clinics for therapy, adopting randomization can be very challenging.
The participants were recruited from various online platforms and in person at the outpatient clinic at a tertiary Hospital through quick response (QR) codes that contained the link. The data were collected through an online questionnaire using Google Forms. The inclusion criteria for the participants were being aged 18 or above, having acne scarring, and residing in Riyadh, Saudi Arabia. Any participants who had scars due to other reasons than acne were excluded from the study.
Ethical consideration
This study adhered to the ethical guidelines outlined in the Declaration of Helsinki. Consent was obtained before starting the questionnaire. No information revealing the identity of the participants was collected. Approval was granted by the Institutional Review Board in Riyadh, Saudi Arabia, on June 7, 2023.
The questionnaire
An online-administered questionnaire comprising four sections was designed and translated to Arabic then back-translated to ensure the overall quality.
The first section included sociodemographic data as described in Table 1.
| Characteristic | Overall, n=401 (%) | SCARS | FASQoL | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Clear/almost clear, n=50 (%) | Mild, n=130 (%) | Moderate, n=127 (%) | Severe/very severe, n=94 (%) | P-value | Mild, n=245 (%) | Moderate, n=72 (%) | Severe, n=84 (%) | P-value | ||
| Gender | ||||||||||
| Male | 143 (35.7) | 14 (28.0) | 53 (40.8) | 44 (34.6) | 32 (34.0) | 0.404 | 96 (39.2) | 29 (40.3) | 18 (21.4) | 0.009 |
| Female | 258 (64.3) | 36 (72.0) | 77 (59.2) | 83 (65.4) | 62 (66.0) | 149 (60.8) | 43 (59.7) | 66 (78.6) | ||
| Age (year) | ||||||||||
| 18–29 | 295 (73.6) | 39 (78.0) | 101 (77.7) | 97 (76.4) | 58 (61.7) | 0.172 | 186 (75.9) | 55 (76.4) | 54 (64.3) | 0.235 |
| 30–39 | 76 (19.0) | 7 (14.0) | 19 (14.6) | 24 (18.9) | 26 (27.7) | 40 (16.3) | 15 (20.8 ) | 21 (25.0) | ||
| 40–49 | 25 (6.2) | 3 (6.0) | 8 (6.2) | 5 (3.9) | 9 (9.6) | 15 (6.1) | 2 (2.8) | 8 (9.5) | ||
| 50 or more | 5 (1.2) | 1 (2.0) | 2 (1.5) | 1 (0.8) | 1 (1.1) | 4 (1.6) | 0 (0.0) | 1 (1.2) | ||
| Marital status | ||||||||||
| Single | 309 (77.1) | 44 (88.0) | 107 (82.3) | 102 (80.3) | 56 (59.6) | <0.001 | 203 (82.9) | 58 (80.6) | 48 (57.1) | <0.001 |
| Married | 78 (19.5) | 6 (12.0) | 20 (15.4) | 19 (15.0) | 33 (35.1) | 36 (14.7) | 13 (18.1) | 29 (34.5) | ||
| Widowed | 1 (0.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (1.1) | 0 (0.0) | 1 (1.4) | 0 (0.0) | ||
| Divorced | 13 (3.2) | 0 (0.0) | 3 (2.3) | 6 (4.7) | 4 (4.3) | 6 (2.4) | 0 (0.0) | 7 (8.3) | ||
| Nationality | ||||||||||
| Saudi | 342 (85.3) | 45 (90.0) | 108 (83.1) | 107 (84.3) | 82 (87.2) | 0.619 | 207 (84.5) | 62 (86.1) | 73 (86.9) | 0.844 |
| Non-Saudi | 59 (14.7) | 5 (10.0) | 22 (16.9) | 20 (15.7) | 12 (12.8) | 38 (15.5) | 10 (13.9) | 11 (13.1) | ||
| Educational level | ||||||||||
| Illiterate | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.172 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.325 |
| Primary | 1 (0.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (1.1) | 0 (0.0) | 0 (0.0) | 1 (1.2) | ||
| Intermediate | 2 (0.5) | 1 (2.0) | 0 (0.0) | 0 (0.0) | 1 (1.1) | 1 (0.4) | 1 (1.4) | 0 (0.0) | ||
| Secondary | 67 (16.7) | 4 (8.0) | 22 (16.9) | 20 (15.7) | 21 (22.3) | 40 (16.3) | 9 (12.5) | 18 (21.4) | ||
| Diploma | 29 (7.2) | 4 (8.0) | 6 (4.6) | 11 (8.7) | 8 (8.5) | 16 (6.5) | 5 (6.9) | 8 (9.5) | ||
| University or postgraduate studies | 302 (75.3) | 41 (82.0) | 102 (78.5) | 96 (75.6) | 63 (67.0) | 188 (76.7) | 57 (79.2) | 57 (67.9) | ||
| Occupation | ||||||||||
| Businessperson | 11 (2.7) | 1 (2.0) | 1 (0.8) | 6 (4.7) | 3 (3.2) | 0.015 | 6 (2.4) | 3 (4.2) | 2 (2.4) | 0.138 |
| Healthcare worker | 57 (14.2) | 10 (20.0) | 16 (12.3) | 16 (12.6) | 15 (16.0) | 34 (13.9) | 8 (11.1) | 15 (17.9) | ||
| Housewife | 30 (7.5) | 3 (6.0) | 7 (5.4) | 7 (5.5) | 13 (13.8) | 14 (5.7) | 5 (6.9) | 11 (13.1) | ||
| Military | 5 (1.2) | 0 (0.0) | 0 (0.0) | 4 (3.1) | 1 (1.1) | 3 (1.2) | 1 (1.4) | 1 (1.2) | ||
| Office work | 63 (15.7) | 5 (10.0) | 25 (19.2) | 15 (11.8) | 18 (19.1) | 40 (16.3) | 11 (15.3) | 12 (14.3) | ||
| Retired | 2 (0.5) | 1 (2.0) | 0 (0.0) | 0 (0.0) | 1 (1.1) | 1 (0.4) | 0 (0.0) | 1 (1.2) | ||
| Student | 175 (43.6) | 23 (46.0) | 65 (50.0) | 61 (48.0) | 26 (27.7) | 118 (48.2) | 34 (47.2) | 23 (27.4) | ||
| Teacher | 19 (4.7) | 2 (4.0) | 2 (1.5) | 8 (6.3) | 7 (7.4) | 9 (3.7) | 4 (5.6) | 6 (7.1) | ||
| Unemployed | 39 (9.7) | 5 (10.0) | 14 (10.8) | 10 (7.9) | 10 (10.6) | 20 (8.2) | 6 (8.3) | 13 (15.5) | ||
| Household income (SAR) | ||||||||||
| <5,000 | 82 (20.4) | 13 (26.0) | 24 (18.5) | 20 (15.7) | 25 (26.6) | 0.022 | 49 (20.0) | 9 (12.5) | 24 (28.6) | <0.001 |
| 5,000– <10,000 | 62 (15.5) | 3 (6.0) | 16 (12.3) | 19 (15.0) | 24 (25.5) | 29 (11.8) | 9 (12.5) | 24 (28.6) | ||
| 10,000–<15,000 | 60 (15.0) | 4 (8.0) | 24 (18.5) | 19 (15.0) | 13 (13.8) | 39 (15.9) | 9 (12.5) | 12 (14.3) | ||
| 15,000–<20,000 | 45 (11.2) | 6 (12.0) | 14 (10.8) | 16 (12.6) | 9 (9.6) | 26 (10.6) | 13 (18.1) | 6 (7.1) | ||
| 20,000 or more | 152 (37.9) | 24 (48.0) | 52 (40.0) | 53 (41.7) | 23 (24.5) | 102 (41.6) | 32 (44.4) | 18 (21.4) | ||
| SCARS | ||||||||||
| Clear/almost clear | NA | NA | NA | NA | NA | NA | 45 (18.4) | 4 (5.6) | 1 (1.2) | <0.001 |
| Mild | NA | NA | NA | NA | NA | 118 (48.2) | 7 (9.7) | 5 (6.0) | ||
| Moderate | NA | NA | NA | NA | NA | 65 (26.5) | 38 (52.8) | 24 (28.6) | ||
| Severe/very severe | NA | NA | NA | NA | NA | 17 (6.9) | 23 (31.9) | 54 (64.3) | ||
SCARS: Self-assessment of clinical acne-related scars, FASQoL: Facial acne scar quality of life, , NA: Not applicable, SAR: Saudi Riyals
The second section adopted a validated tool (self-assessment of clinical acne-related scars [SCARS] Questionnaire) comprising a set of seven items.13
The SCARS tool employed in our research comprises two integral parts, each designed to provide a nuanced evaluation of different aspects of skin health. The first part includes two specific questions to assess the current state of participants’ skin: Participants were first asked to identify current signs of active acne, such as zits, breakouts, pimples, whiteheads, or blackheads. This aimed to assess the current presence of active acne and gauge its severity. In addition, participants were prompted to inspect their faces for indents or holes resulting from past acne. This assessed the current presence of acne scarring and focused on discerning the severity of any observed scarring from previous acne. In addition, the second part of the SCARS tool comprises five inquiries that assess severity in terms of coverage, size, amount, depth, and visibility, each offering five potential responses on a scale from 0 to 4. Higher scores on this scale correspond to more severe scarring. The interpretation of SCARS scores is as follows: Scores ranging from 0 to 2 signify a state of clear/nearly clear scarring, scores from 3 to 6 indicate mild scarring, scores from 7 to 10 suggest moderate scarring, while scores falling within the range of 11–20 denote severe to very severe scarring.13,14 In the present study, the SCARS responses showed an excellent level of reliability (Cronbach’s alpha = 0.901).
The third section contains the Facial Acne Scar QoL (FASQoL) validated tool (FASQoL Questionnaire), which is a 10-item instrument with three domains assessing the impact of scars on emotions, social functioning, and work/school. Each question in the tool offers five potential responses and scoring options ranging from 0 to 4. The cumulative score ranged from 0 to 40, where higher scores indicated a more pronounced impairment in Health-Related QoL.13 Reliability analysis showed an excellent level of internal consistency (Cronbach’s alpha = 0.955). The aforementioned tools have open access to the Creative Commons Attribution-Noncommercial 4.0 International License, which permits noncommercial use.
The Fourth section consists of a set of questions to assess the WTP for acne scar treatment. The questions were selected and adopted from a previous study, and permission to use them was granted by the authors.15 The first question assessed awareness of treatment modalities, identified by their common names. Experts in the field assisted with the revision process to make sure that the proper modalities for treatment used in our community were included in the study.
The subsequent questions inquired of the participants about the cost of previous treatments, their WTP for future treatment, and how much they were willing to pay.
Statistical analysis
Data analysis was performed using RStudio (R version 4.3.0). A multiple-response analysis was used to assess participants’ awareness regarding modalities used for acne scar management. The association between sociodemographics and different outcomes, such as the categories of SCARS and FASQoL scales as well as the WTP for acne scar management, was examined using either Pearson’s Chi-squared test or Fisher’s exact test. A multivariable logistic regression analysis was conducted to assess the predictors of participants’ WTP for acne scar management using the significantly associated variables in the univariable analysis as independent variables. Variables that altered the model’s violation or influenced model fit were excluded from the study. The outcomes were expressed as odds ratios (ORs) and their respective 95% confidence intervals (CIs). P < 0.05 indicates statistical significance.
RESULTS
Sociodemographic characteristics
In the present study, we received a total of 633 responses. However, excluded were records of 79 respondents who had no acne lesions and 153 responses from those with active current acne lesions without scars [Figure 1]. Therefore, a total of 401 adult participants were included in the study. The majority of the participants were female (64.3%), and most were in the age range of 18–29 years (73.6%). Regarding nationality, the majority were Saudi (85.3%). The highest educational level attained by most participants was university or postgraduate studies (75.3%). In terms of occupation, the largest proportion of participants were students (43.6%), followed by office workers (15.7%). Concerning household income, the most common category was “20,000 Saudi Riyals (SAR) or more,” accounting for 37.9% of the participants [Table 1].
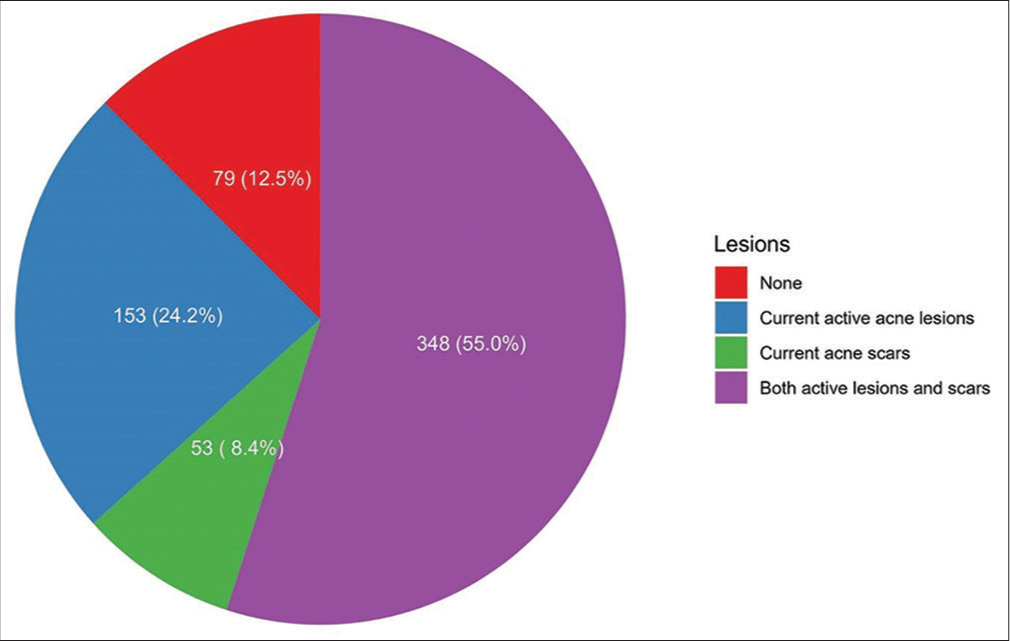
- Proportions of acne lesions among all the participants of the study.
Description of the SCARS and FASQoL results and their association with the sociodemographic characteristics
Out of the included participants, mild, moderate, and severe SCARS categories were prevalent among 32.4%, 31.7%, and 23.4%, respectively, whereas mild, moderate, and severe FASQoL categories were reported among 61.1%, 18.0%, and 20.9% of them, respectively [Figure 2]. Based on the inferential analyses, significant differences in the severity of scars are based on marital status (P < 0.001), occupation (P = 0.015), and household income (P = 0.022). In addition, there were significant differences in the FASQoL categories in terms of participants’ gender (P = 0.009), marital status (P < 0.001), and household income (P < 0.001). Furthermore, the categories of severity on the SCARS questionnaire differed significantly according to the QoL of participants (P < 0.0001, [Table 1]).
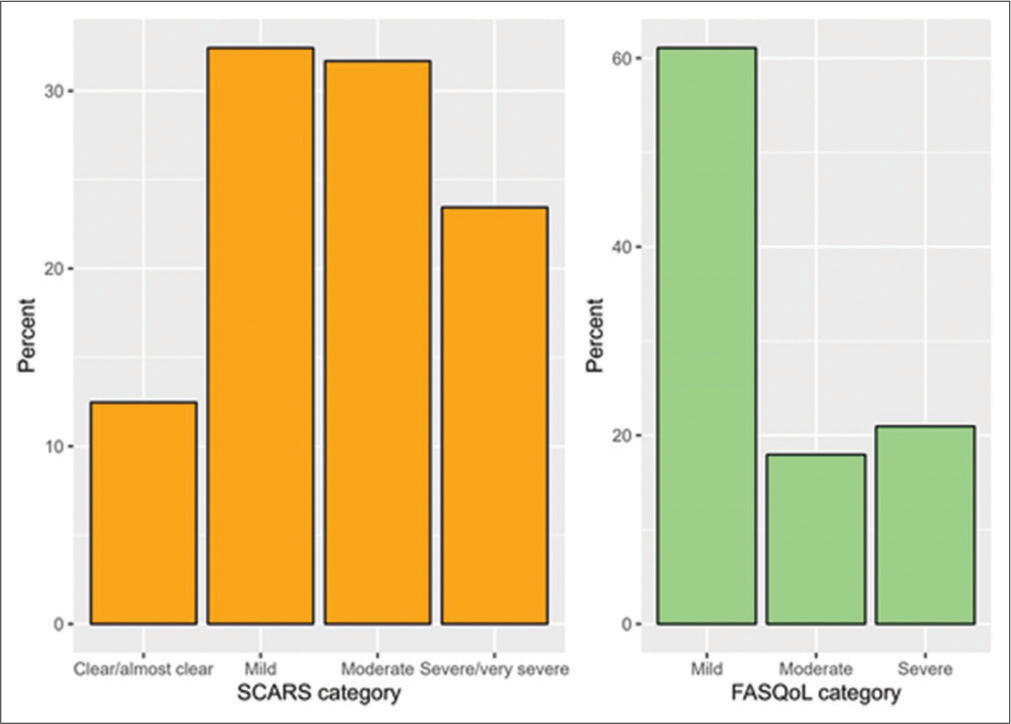
- Proportions of Each Self-Assessment of Clinical Acne-Related Scars (SCARS) and Facial Acne Scar Quality of Life (FASQoL) Category among study participants.
Awareness regarding the modalities used for acne scar treatment
Based on participants’ responses, the most commonly identified modalities for acne scar management were laser resurfacing (66.3%) and chemical peels (64.1%), whereas the least perceived modalities were collagen/fat filler injections (23.9%) and radiofrequency microneedling (27.7%, [Figure 3]).
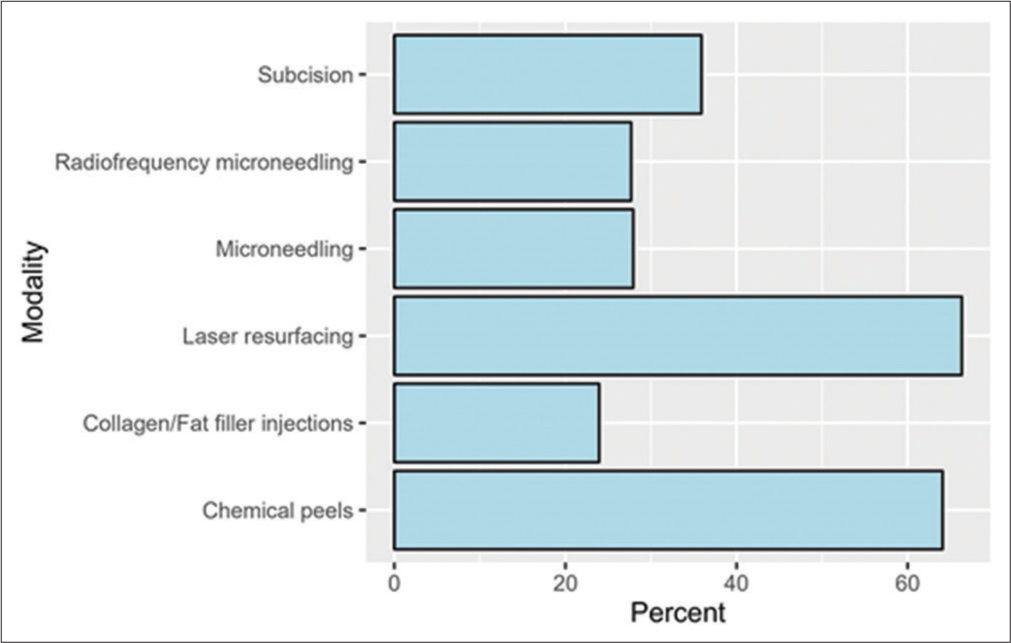
- Proportions of awareness regarding acne scar treatment modalities among the included participants of the study.
Participants’ responses regarding their payment for acne scar treatment
Table 2 presents the participants’ responses regarding their payment and WTP for acne scar treatment. Among the respondents, 43.4% reported that they had never undergone any scar treatment in the past. A total of 277 participants (69.1%) were willing to pay for acne scar treatment, of whom the majority (45.8%) expressed a WTP of <1000 SAR and 42.2% were willing to pay 1000–6000 SAR for treatment.
| Characteristic | N (%) |
|---|---|
| How much did you previously pay for acne scar treatment? | |
| Never done any scar treatment | 174 (43.4) |
| <1000 SAR | 109 (27.2) |
| 1000–6000 SAR | 74 (18.5) |
| >6000 SAR | 44 (11.0) |
| Willing to pay for acne scars treatment | |
| No | 124 (30.9) |
| Yes | 277 (69.1) |
| If yes, how much are you willing to pay for acne scar treatment?* | |
| <1000 SAR | 127 (45.8) |
| 1000–6000 SAR | 117 (42.2) |
| >6000 SAR | 33 (11.9) |
Factors associated with the WTP for acne scar treatment
The WTP for acne scar treatment was examined with several demographic and clinical variables. Among the variables analyzed, nationality, educational level, household income, QoL categories, and awareness of selected acne scar modalities showed significant associations with participants’ WTP for treatment (P < 0.05). Significantly higher proportions of those who were willing to pay were Saudi (90.3% vs. 74.2%, P < 0.001), had a university degree or higher (79.1% vs. 66.9%, P = 0.030), had a high household income (45.5% vs. 21.0%, P < 0.001), and had a moderate FASQoL category (21.3% vs. 10.5%, P = 0.030). Moreover, the proportions of participants who were willing to pay for acne scar treatment were significantly higher than their peers without the WTP in terms of their awareness levels regarding the following modalities: Chemical peels (69.0% vs. 53.2%, P = 0.002), laser resurfacing (69.7% vs. 58.9%, P = 0.034), microneedling (32.5% vs. 17.7%, P = 0.002), and radiofrequency microneedling (32.1% vs. 17.7%, P = 0.003, [Table 3]).
| Characteristic | Willing to pay for acne scar treatment | ||||
|---|---|---|---|---|---|
| No, n=124 (%) | Yes, n=277 (%) | P-value | |||
| Gender | |||||
| Male | 47 (37.9) | 96 (34.7) | 0.531 | ||
| Female | 77 (62.1) | 181 (65.3) | |||
| Age (year) | |||||
| 18–29 | 95 (76.6) | 200 (72.2) | 0.312 | ||
| 30–39 | 20 (16.1) | 56 (20.2) | |||
| 40–49 | 6 (4.8) | 19 (6.9) | |||
| 50 or more | 3 (2.4) | 2 (0.7) | |||
| Marital status | |||||
| Single | 97 (78.2) | 212 (76.5) | 0.774 | ||
| Married | 22 (17.7) | 56 (20.2) | |||
| Widowed | 0 (0.0) | 1 (0.4) | |||
| Divorced | 5 (4.0) | 8 (2.9) | |||
| Nationality | |||||
| Saudi | 92 (74.2) | 250 (90.3) | <0.001 | ||
| Non-Saudi | 32 (25.8) | 27 (9.7) | |||
| Educational level | |||||
| Illiterate | 0 (0.0) | 0 (0.0) | 0.030 | ||
| Primary | 0 (0.0) | 1 (0.4) | |||
| Intermediate | 1 (0.8) | 1 (0.4) | |||
| Secondary | 30 (24.2) | 37 (13.4) | |||
| Diploma | 10 (8.1) | 19 (6.9) | |||
| University or postgraduate studies | 83 (66.9) | 219 (79.1) | |||
| Occupation | |||||
| Businessperson | 2 (1.6) | 9 (3.2) | 0.080 | ||
| Healthcare worker | 13 (10.5) | 44 (15.9) | |||
| Housewife | 13 (10.5) | 17 (6.1) | |||
| Military | 2 (1.6) | 3 (1.1) | |||
| Office work | 15 (12.1) | 48 (17.3) | |||
| Retired | 1 (0.8) | 1 (0.4) | |||
| Student | 55 (44.4) | 120 (43.3) | |||
| Teacher | 4 (3.2) | 15 (5.4) | |||
| Unemployed | 19 (15.3) | 20 (7.2) | |||
| Household income (SAR) | |||||
| <5000 | 37 (29.8) | 45 (16.2) | <0.001 | ||
| 5000–<10,000 | 27 (21.8) | 35 (12.6) | |||
| 10,000–<15,000 | 19 (15.3) | 41 (14.8) | |||
| 15,000–<20,000 | 15 (12.1) | 30 (10.8) | |||
| 20,000 or more | 26 (21.0) | 126 (45.5) | |||
| Aware of acne scar modalities | |||||
| Chemical peels | 66 (53.2) | 191 (69.0) | 0.002 | ||
| Collagen/Fat filler injections | 24 (19.4) | 72 (26.0) | 0.150 | ||
| Laser resurfacing | 73 (58.9) | 193 (69.7) | 0.034 | ||
| Subcision | 40 (32.3) | 104 (37.5) | 0.308 | ||
| Microneedling | 22 (17.7) | 90 (32.5) | 0.002 | ||
| Radiofrequency microneedling | 22 (17.7) | 89 (32.1) | 0.003 | ||
| SCARS categories | |||||
| Clear/almost clear | 14 (11.3) | 36 (13.0) | 0.409 | ||
| Mild | 47 (37.9) | 83 (30.0) | |||
| Moderate | 34 (27.4) | 93 (33.6) | |||
| Severe/very severe | 29 (23.4) | 65 (23.5) | |||
| FASQoL categories | |||||
| Mild | 81 (65.3) | 164 (59.2) | 0.030 | ||
| Moderate | 13 (10.5) | 59 (21.3) | |||
| Severe | 30 (24.2) | 54 (19.5) | |||
FASQoL: Facial acne scar quality of life, SCARS: Self-Assessment of Clinical Acne- Related Scars, SAR: Saudi Riyals
In the regression analysis, we sought to include the significantly associated variables with participants’ WTP in the inferential analysis as independent variables in the multivariable regression model. However, the educational level variable was excluded because it did not allow proper fitting of the model. Results revealed that participants who were Saudi nationals (OR = 3.41, 95% CI: 1.83–6.44, P < 0.001), those with a household income of 20,000 SAR or more (OR = 2.69, 95% CI: 1.38–5.29, P = 0.004), and those categorized as “Moderate” on the FASQoL scale (OR = 2.17, 95% CI: 1.09– 4.56, P = 0.033) had a higher OR for being willing to pay for acne management. In terms of awareness regarding acne scar treatment modalities, participants who were aware of chemical peels demonstrated a higher OR (OR = 1.82, 95% CI: 1.13– 2.96, P = 0.014) for being willing to pay for acne management compared to those who were unaware [Table 4].
| Characteristic | OR | 95%CI | P-value |
|---|---|---|---|
| Nationality | |||
| Non-Saudi | — | — | |
| Saudi | 3.41 | 1.83, 6.44 | <0.001 |
| Household income (SAR) | |||
| <5000 | — | — | |
| 5,000–<10,000 | 0.91 | 0.45, 1.83 | 0.782 |
| 10,000–<15,000 | 1.55 | 0.74, 3.29 | 0.245 |
| 15,000–<20,000 | 0.92 | 0.40, 2.11 | 0.836 |
| 20,000 or more | 2.69 | 1.38, 5.29 | 0.004 |
| Awareness regarding acne scar treatment modalities | |||
| Microneedling | 1.66 | 0.94, 3.01 | 0.086 |
| Chemical peels | 1.82 | 1.13, 2.96 | 0.014 |
| Laser resurfacing | 1.15 | 0.69, 1.90 | 0.589 |
| Radiofrequency microneedling | 1.24 | 0.68, 2.28 | 0.489 |
| FASQoL category | |||
| Mild | — | — | |
| Moderate | 2.17 | 1.09, 4.56 | 0.033 |
| Severe | 1.13 | 0.64, 2.02 | 0.686 |
OR: Odds ratio, CI: Confidence interval, FASQoL: Facial acne scar quality of life, SAR: Saudi Riyals
DISCUSSION
Acne vulgaris is one of the most common skin conditions.3 It frequently leaves the affected individuals with scarring that predisposes them to numerous psychological conditions.16,17 Due to the significant impact on the QoL, the results highlight acne scar prevalence, severity, QoL impact, awareness of treatment options, and WTP. In the present study, the prevalence of acne scarring was found to be 63.4% [Figure 1], which was broadly in line with a past study,18 in which 73% of the participants complained of acne scarring. However, our findings differed significantly from other studies conducted in Brazil, USA, Morocco, and Japan, where acne scars occurred in 22%,19 43%,20 84%,21 and 91%22 respectively. This could be due to ethnicity-specific scarring response variation, with some more likely than others.23
The present study describes the results of sociodemographics and SCAR severity and their associations with QoL, indicating that severe acne scars and female gender are independent factors for decreased psychosocial well-being, which concurs with earlier research.14,24 The severe SCARS category was associated with an increased score of FASQoL. Yet, 9.8% of the participants with a moderate and lower SCARS score displayed severe effects on FASQoL, highlighting the negative impact on self-image even with minor scarring.
The majority of the participants had good awareness regarding acne scar treatment; nevertheless, 43.4% never underwent any treatment for their scars, and 30.9% were not willing to undergo any treatment. Reluctance to undergo treatment may stem from the lack of awareness, belief scars are untreatable, fear of side effects, and cost. When compared with participants from a study set in Nigeria, only 14% were not willing to pay for acne scars.15 Furthermore, of the 69.1% who were willing to pay for acne scar therapy in the present study, almost half were not willing to pay the amount for a good result, which is below 1000 SAR. The price to get satisfying results depends on the type of scar, its severity, and the procedure performed. This finding was also seen previously in the antecedent study, where the majority of the participants were willing to pay, but it was low compared to the cost of pleasing treatment.15 However, another study conducted in China showed that participants were more willing to pay for treatment.25 We speculate that this is due to cultural differences in skincare and economic differences.
The participants showed considerable awareness of some treatment modalities but not all. The awareness varied from only 23.9% being aware of collagen/fat filler injection to 66.3% being aware of laser resurfacing, as shown in Figure 3. This is significantly higher than that of the aforesaid Nigerian study.15 This could be because Saudi Arabia has a more established dermatology and cosmetics infrastructure. This speculation is supported by Alsharif et al.26 who concluded in his study that the Saudi population displayed good knowledge of skin care.
The findings reveal a significant correlation between a higher FASQoL score and subjectively increased WTP, whereas no significant link was observed between an elevated SCARS score and WTP. This suggests that individuals may subjectively express a greater WTP for psychological benefits compared to physical attractiveness, providing insight into this particular observation. Similarly, Reckers-Droog et al.27 reported in their study that participants are more willing to pay for higher QoL gains.
Awareness of acne scar modalities was associated with increased WTP, which is consistent with the previous literature.15 Participants who were aware of chemical peels, laser resurfacing, microneedling, and radiofrequency microneedling were more willing to pay. On the other hand, participants who were aware of collagen/fat filler injections and subcision were less willing to pay; this could be attributed to the invasiveness of these techniques and their fear of them. Furthermore, the regression analysis showed that being aware of chemical peels made participants 1.82 times more likely to pay, whereas awareness of other modalities did not affect WTP. This finding is similar to Xiao et al.’s,25 in which they described that desirable treatment effectiveness was strongly correlated with WTP for chemical peels. This finding can also be explained by the fact that the population is more familiar with the older chemical peels and, therefore, has more trust in them. A 2017 systematic review28 found that post-acne scarring improves by 10–100% following subcision, 31–62% improvement with microneedling and dermal fillers showing positive results. Trichloroacetic acid chemical reconstruction of skin scars showed 70% improvement in 73.3% of patients, while 20% glycolic acid had no effect in 25%. Each technique has its benefits and risks, and specific therapies should be used accordingly. Even though chemical peels are known, participants need to be familiar with the new techniques.
Multivariate regression analysis with confounding variables controlled demonstrated that Saudi locals were 3.41 times more likely to pay than non-Saudis. These results support prior studies and show a strong relationship between non-local income and WTP for healthcare services.29 Furthermore, locals could have better familiarity with the medical system and higher faith in the standard of care.
An additional income-related finding revealed that in the multivariate linear regression model as well as the univariate analysis, higher income substantially predicted WTP. Consistent with earlier research,25,30 multivariate analysis revealed that participants whose monthly family income was above 20,000 SAR (5331 USD) were 2.69 times more likely to make a payment. This finding is well proven in literature, in which the WTP and adjusted QoL both rise with subject wealth, as has been previously demonstrated.31,32
A noteworthy finding revealed that participants with moderate impact on FASQoL were 2.17 times more likely to pay, while those with mild and severe impairments showed no increase in WTP. We surmise that with a powerful impact on the QoL, this leads to an increase in psychological consequences that may discourage individuals from seeking treatment, hence explaining the above-mentioned result. For comparison, a study conducted in Iraq33 found that the more severe the lesion, the greater the impact it had on QoL, leading to an increase in psychological severity.
There were a few limitations encountered during our study. First, there was limited data in the literature regarding the QoL of patients suffering from acne scars and its relation to their WTP for acne scar treatment, which proved challenging when discussing our data with current available studies. Furthermore, the study may also be subject to selection and recall biases.
Although the present study offers insightful data about acne scars and their effects in the region, there is still room for development. Henceforth, we recommend future studies include a larger sample size, an in-depth exploration to assess how the degree of the participant’s knowledge of different acne scar treatment modalities will affect their WTP and each socioeconomic group to be associated with the percentage of participants willing to pay to get their acne scars adjusted for the effect on their QoL. This will help clinicians provide more cost-effective methods for patients struggling with the psychological consequences of acne scarring.
In addition, future research should carefully examine the causes behind treatment reluctance, taking into account elements such as cost, side effect concerns, perceptions of scar treatability, and awareness, to fill in the gaps in the existing literature and offer a more objective understanding.
CONCLUSION
Participants demonstrated good awareness of different acne scar treatment modalities, with laser resurfacing and chemical peels being the most recognized modalities. However, even with good knowledge regarding the modalities, a significant percentage of patients are reluctant to undergo any treatment. Furthermore, WTP for acne scar treatment was more influenced by psychological effects than physical severity. Moreover, other factors that influence WTP include income levels, awareness of treatment modalities, and being a resident. Ultimately, these findings could influence dermatologists to start awareness campaigns to shed light on acne scar treatment modalities and their efficacy in improving QoL.
Authors’ contributions
Salim Alkeraye: concept, design, definition of intellectual content, literature search, clinical studies, data acquisition, manuscript editing, and manuscript review. Khalid Alosaimi: concept, design, definition of intellectual content, literature search, clinical studies, experimental studies, manuscript editing, and manuscript review. Hamad F. Alrabiah: literature search, clinical studies, data analysis, statistical analysis, manuscript preparation, manuscript editing, and manuscript review. Rema Alkahtani: literature search, clinical studies, data analysis, statistical analysis, manuscript preparation, manuscript editing, and manuscript review. Naif Ahmed Alshehri: literature search, clinical studies, data analysis, statistical analysis, manuscript preparation, manuscript editing, and manuscript review. Bander Ahmed Alharbi: literature search, clinical studies, data analysis, statistical analysis, manuscript preparation, manuscript editing, and manuscript review.
Ethical approval
The study was approved by the Institutional Review Board in Riyadh, Saudi Arabia, number E-23-7839, dated 07-06-2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Guidelines of care for acne vulgaris management. J Am Acad Dermatol. 2007;56:651-63.
- [CrossRef] [PubMed] [Google Scholar]
- The global burden of skin disease in 2010: An analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014;134:1527-34.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of acne vulgaris in adolescence. Br J Dermatol. 1971;85:119-26.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of acne vulgaris, its contributing factors, and treatment satisfaction among the Saudi population in Riyadh, Saudi Arabia: A cross-sectional study. J Dermatol Dermatol Surg. 2020;24:33.
- [CrossRef] [Google Scholar]
- Laser resurfacing for facial acne scars In: Jordan R, ed. Cochrane database of systematic reviews. Chichester, UK: John Wiley and Sons. Ltd; 2001.
- [CrossRef] [Google Scholar]
- Methods for the improvement of acne scars used in dermatology and cosmetology: A review. J Clin Med. 2022;11:2744.
- [CrossRef] [PubMed] [Google Scholar]
- Acne scars: Pathogenesis, classification and treatment. Dermatol Res Pract. 2010;2010:893080.
- [CrossRef] [PubMed] [Google Scholar]
- Saudi census population summary report 2022 Riyadh. 2022. Available from: https://portal.saudicensus.sa/portal/public/reports [Last accessed on 2023 Aug 11]
- [Google Scholar]
- New patient-oriented tools for assessing atrophic acne scarring. Dermatol Ther (Heidelb). 2016;6:219-33.
- [CrossRef] [Google Scholar]
- Impact of facial atrophic acne scars on quality of life: A multi-country population-based survey. Am J Clin Dermatol. 2022;23:115-23.
- [CrossRef] [PubMed] [Google Scholar]
- Cross-sectional study of beliefs, perceptions, knowledge of treatment modalities and willingness to pay for acne scar treatment in acne patients. West Afr J Med. 2020;37:625-30.
- [Google Scholar]
- Fractional CO2 lasers for the treatment of atrophic acne scars: A review of the literature. J Cosmet Laser Ther. 2014;16:48-56.
- [CrossRef] [PubMed] [Google Scholar]
- Beyond the surface: A deeper look at the psychosocial impacts of acne scarring. Clin Cosmet Investig Dermatol. 2023;16:731-8.
- [CrossRef] [PubMed] [Google Scholar]
- Development and validation of a scale for acne scar severity (SCAR-S) of the face and trunk. J Cutan Med Surg. 2010;14:156-60.
- [CrossRef] [PubMed] [Google Scholar]
- Acne scars in 18-year-old male adolescents: A population-based study of prevalence and associated factors. An Bras Dermatol. 2016;91:291-5.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and risk factors of acne scarring among patients consulting dermatologists in the USA. J Drugs Dermatol. 2017;16:97-102.
- [Google Scholar]
- Acne scars: Prevalence and impact on quality of life in Moroccan patients. J Dermatol Res Ther. 2023;9:120.
- [CrossRef] [Google Scholar]
- Prevalence of scars and “mini-scars”, and their impact on quality of life in Japanese patients with acne. J Dermatol. 2015;42:690-6.
- [CrossRef] [PubMed] [Google Scholar]
- Racial differences in clinical characteristics, perceptions and behaviors, and psychosocial impact of adult female acne. J Clin Aesthet Dermatol. 2014;7:19-31.
- [Google Scholar]
- The individual health burden of acne. J Health Psychol. 2009;14:1105-18.
- [CrossRef] [PubMed] [Google Scholar]
- Willingness-to-pay and benefit-cost analysis of chemical peels for acne treatment in China. Patient Prefer Adherence. 2019;13:363-70.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge, attitudes, and practices regarding skin care in Saudi Arabia: A cross-sectional, survey-based study. Cureus. 2022;14:e32490.
- [CrossRef] [Google Scholar]
- Willingness to pay for health-related quality of life gains in relation to disease severity and the age of patients. Value Health. 2021;24:1182-92.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review of treatments for acne scarring. Part 1: Non-energy-based techniques. Scars Burn Health. 2017;3:2059513117695312.
- [CrossRef] [PubMed] [Google Scholar]
- Redressing the limitations of the affordable care act for Mexican immigrants through bi-national health insurance: A willingness to pay study in Los Angeles. J Immigr Minor Health. 2014;16:179-88.
- [CrossRef] [PubMed] [Google Scholar]
- A community-based study of acne-related health preferences in adolescents. Arch Dermatol. 2008;144:988-94.
- [CrossRef] [PubMed] [Google Scholar]
- Willingness to pay for a quality-adjusted life-year: The individual perspective. Value Health. 2010;13:1046-55.
- [CrossRef] [PubMed] [Google Scholar]
- Willingness to pay for a quality-adjusted life year: An evaluation of attitudes towards risk and preferences. BMC Health Serv Res. 2014;14:287.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life in patients with acne in Erbil city. Health Qual Life Outcomes. 2012;10:60.
- [CrossRef] [PubMed] [Google Scholar]







