Translate this page into:
An Innovative Approach for Nasal Reshaping using Hyaluronic Acid Intradermal Injections
Address for correspondence: Francesco Romeo, Studio Romeo, Corso Vittorio Emanuele II, 18, Rome, Italy. E-mail: fran.romeo@libero.it
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Nasal reshaping using hyaluronic acid (HA) filler has become a widespread technique and injections are usually performed in deep layers. As an alternative, we propose an innovative approach where HA is injected into the dermis, the so called MesoRhinoFiller.
Aims and Objectives:
The aim of this study was to describe our injection technique using a smooth, cohesive, and slightly viscous HA filler injected in the dermis.
Materials and Methods:
A retrospective review of the author’s clinical experience from March 2017 to March 2020 was presented. A total of 280 consecutive patients were treated with HA injections to improve their nasal appearance. The mean volume was 0.5 cc HA filler/treatment.
Results:
An average increase of 4.9 ± 3.4° was obtained for the nasofrontal angle, and of 7.0 ± 4.5° for the columella labial angle. Asymmetries in the nasal profile and alar rim were also corrected. All the patients were satisfied with the results and no complications occurred.
Conclusion:
Injecting HA fillers in the dermal plane is a versatile approach that provides very satisfactory results. This technique allows one to better correct aesthetical, post-traumatic, and post-surgical defects compared with the usual injection rhinoplasty procedures where the filler is injected deep onto the bone/cartilage in the midline of the nose.
Keywords
Hyaluronic acid filler
intradermal injections
nasal reshaping
rhinofiller
INTRODUCTION
Nasal reshaping using injectable fillers is becoming an increasingly used approach to smooth out or correct contour irregularities in Caucasian patients without having to resort to surgery.[12345] It is possible to harmonize the dorsum, project the tip forward, narrow the nostrils, and lower the columella, thus changing the shape and projection of the nose. Injection rhinoplasty can be used also to correct irregularities and asymmetries following surgical rhinoplasty or traumatic events.
The skin of the nose is peculiar due to its anatomic location, and it is thinner and more mobile proximally, and becomes thicker and more immobile distally.[678] In the literature, the presence of five soft-tissue layers overlying the osteocartilaginous framework has been highlighted.[9] In particular, there is the skin envelope, the superficial fibrofatty areolar layer, the middle fibromuscular layer, the deep areolar layer, and the periosteum or perichondrium. Usually, the filler is injected in the midline of the nose and deeply onto the bone or periosteum itself, or on the dorsal edge of the cartilaginous septum. Over the nose, the arterial supply is paired on either side with an alar, columellar, and dorsal nasal artery on each side. The midline of the nose is a vascular watershed and the safest way to deliver deep injections of filler material to the nose is to stay on the midline thus avoiding any of the major blood vessel. This approach allows limited corrections and when the filler is injected deep to the bone/cartilage onto the periosteum and perichondrium it passes through the superficial fibrofatty areolar layer, the fibromuscular layer, and the deep areolar layer. As the vascular network of the nose lies on the surface of the fibromuscular layer, with this approach the filler material could be inadvertently injected into a nasal blood vessel causing serious complications and visual compromise.[10]
As an innovative procedure, we propose to inject the filler in the dermal layer of the nose where the blood vessels are thinner, and the paradoxical embolism does not occur. This approach is more versatile as compared to the usual injection rhinoplasty procedures and it allows a better correction of aesthetical, post-traumatic, and post-surgical defects.
Here, the author presents his clinical experience of nasal treatments using hyaluronic acid (HA), with case descriptions to illustrate the proposed injection technique and the treatment outcomes evaluated using anthropometric measurements and the Global Aesthetic Improvement Scale (GAIS) [Table S1].
| Rating | Description |
|---|---|
| Very much improved | Optimal cosmetic result in this patient |
| Much improved | Marked improvement in appearance from the initial condition, but not completely optimal for this patient. A touch-up would slightly improve the result |
| Improved | Obvious improvement in appearance from the initial condition, but a touch-up or retreatment is indicated |
| No change | The appearance is essentially the same as the original condition |
| Worse | The appearance is worse than the original condition |
MATERIALS AND METHODS
Patients
A total of 280 patients (245 Caucasian females and 35 Caucasian males) were enrolled in this study from March 2017 to March 2020. The patients were divided into three groups for each gender based on their clinical history: patients needing a nasal reshaping aged between 18 and 65 years (Group NR), post-rhinoplasty patients aged between 25 and 54 years (Group PR), and post-trauma patients aged between 20 and 45 years (Group PT) (Table S2, Graph S1). Exclusion criteria were a history of medical filler procedures in the nose using undefined materials, immunological, metabolic, hematological and dermatological diseases, unrealistic expectations of treatment results, pronounced scars in the treatment area, bleeding disorder/anticoagulant therapy, abnormal skin thickness. Written informed consent and signed picture and photograph release agreement were obtained from every patient included. This study was exempt from institutional review board approval. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000. Follow-up clinical examinations were carried out after 3 weeks, 3, and 6 months for all the patients and 2 years for more than 50% of them.
| Age (year-old) | ||||
|---|---|---|---|---|
| dN (%) | Min | Max | Mean ± SD | |
| Group NRa | ||||
| Female | 195 (70) | 18 | 65 | 40.2 ± 9.1 |
| Male | 11 (4) | 20 | 60 | 38.4 ± 8.5 |
| Group PRb | ||||
| Female | 28(10) | 25 | 52 | 37.1 ± 8.1 |
| Male | 6 (2) | 26 | 54 | 38.3 ± 8.5 |
| Group PTc | ||||
| Female | 22 (8) | 20 | 45 | 32.7 ± 8.1 |
| Male | 18 (6) | 24 | 43 | 33.2 ± 8.1 |
| Total | 280 (100) | 18 | 65 | 38.8 ± 8.8 |
aGroup NR comprises the patients that underwent a nasal reshape. bGroup PR comprises the patients treated after a rhinoplasty. cGroup PT comprises the patients treated after a nasal trauma. dNumber of patients.
Anthropometric measurements and clinical photographs
All patients were subjected to an accurate analysis of the nasal shape using photographs taken at rest position: frontal, profile (left and right), oblique (left and right), “birds-eye,” above and below views. A proper nasal reshaping planning should be based on anthropometric measurements and the optimal values depend on the gender, ethnic and racial characteristics.[111213] We measured the nasal frontal angle (aNF) that is the projection of the nasion on the soft tissue, it is defined by two lines drawn from the radix, the former parallel to the glabella, the latter parallel to the nasal back [Figure S1A], and the optimal value is 134.0 ± 7.4°;[111213] the rhinion angle (RA) defined by Youn and Seo[13] that is the angle between the nasal dorsum line and the rhinion-to-nasal tip line [Figure S1B], it is used to assess the severity of nasal humps and it should be close to zero; the columella labial angle (aCL) that is defined by the intersection of a tangent line of the columella and a line from the subnasal area toward the labial limb [Figure S1C] and the optimal value is 100.1 ± 8.8° in women and 95.0 ± 5.0° in men; the nasal tip angle (aNT) is calculated through the angle of the lobe toward the nasal wings and it is generally 60.0 ± 10.0° in Caucasians [Figure S1D].[111213] These angular values were measured before and after treatment to assess the validity of the procedure.
Injection procedure
Four soft-tissue areas are monitored: Nasion (P1), Nasal dorsum (P2), Nasal tip (P3), and Subnasal (P4). For the P1, P2, and P3 regions usually two injections are performed at each side of the nose for a total of seven points [Figure 1]. Additional injections in the midline of the nose can be performed in the P1, P2, and P3 regions to harmonize the projection obtained by the lateral injections. Topic local anesthesia (0.1 cc of Mepivacain with 1:100.000 of adrenaline) is administrated at each side of the labial frenulum for the infraorbital nerve block only to correct the P4 region. The HA filler is injected intradermally using a sharp 30-27 G-4 mm needle that slows down the flow of injection and reduces rapid delivery under high pressure. Minute amounts of HA filler should be injected, while gradually evaluating the change in shape. Small volumes of filler are usually sufficient to obtain the desired effect when superficial injections are carried out.
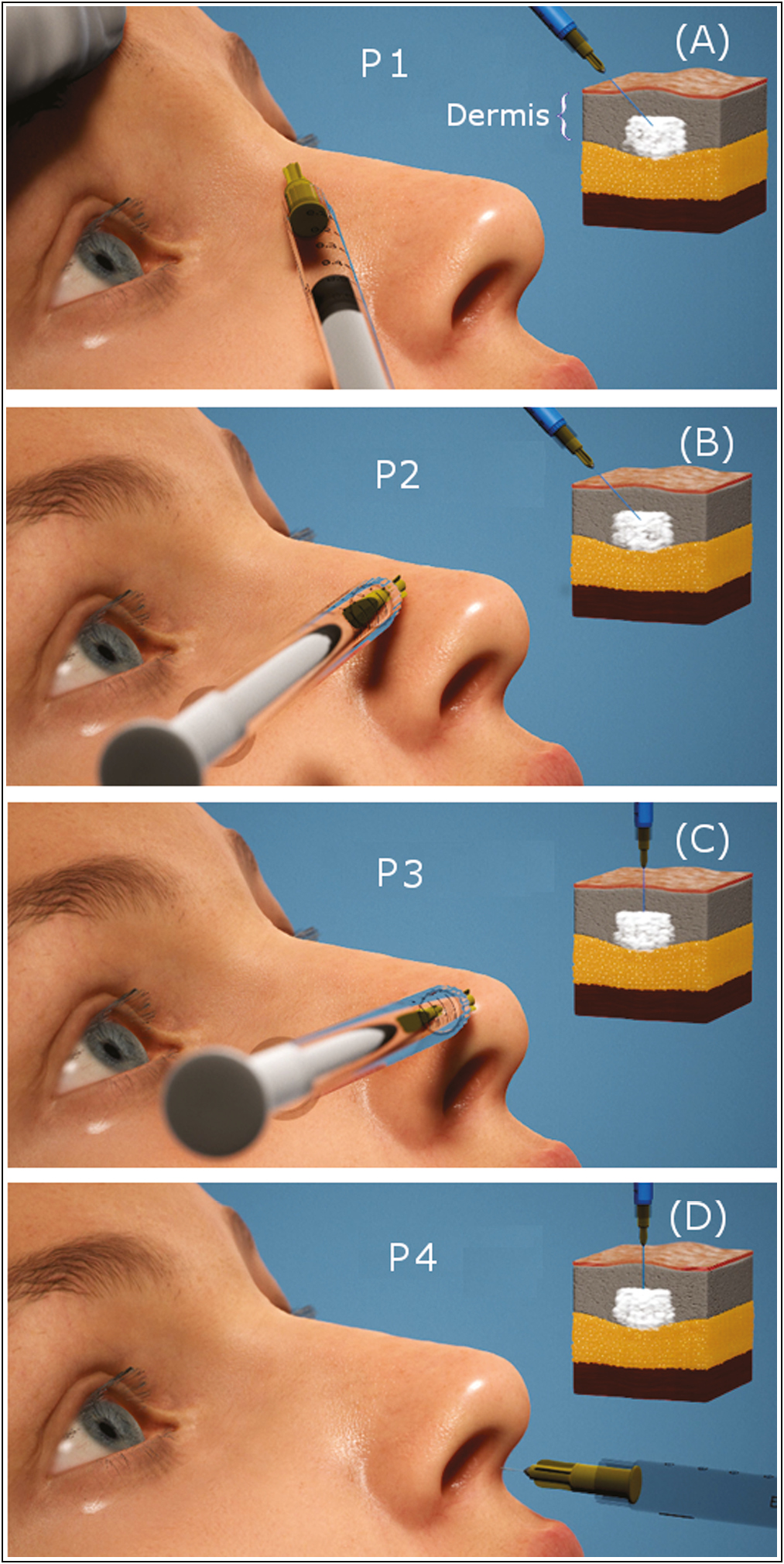
- Main points, namely nasion (P1), nasal dorsum (P2), nasal tip (P3), and subnasal (P4) used in the injection technique and corresponding dermis plane where the injection is carried out
In Figure S2, the thickness of the dermal layer and the location of the blood vessels are clearly visible and confirm that injections on the dermis can be safely carried out. To be sure to be in the dermis in the case of the P1, P2, and P3 regions the needle is inserted at a less than 10° angle and its trajectory must be almost parallel to the skin surface [Figure S3A]. By tilting the needle its tip can be seen [Figure S3B] and during and after the injection a white area appears for few seconds [Figure S3C].
In the presence of a round tip, with aNT > 60° (in Caucasians), the filler is injected into the domes and in the midline of the tip to improve the projection. In the case of a thin tip with aNT < 60°, the HA filler is injected laterally at both sides of the nasal tip area. Injections in the nasal-labial area (P4) are performed to correct the columella retraction or when the nasal wings are suspended (hanging wings). In the P4 region, the needle is inserted perpendicularly along the bisector of the columella labial angle. In most cases, it is not necessary to correct all the seven points but only those responsible for asymmetries and irregularities [Table S3]. In all cases, an LG Chem Ltd., Korea medium density (2.0%–2.2% of HA) cross-linked gel filler with or without lidocaine with tan δ in the range 0.39–0.28 is used.
| P1 (%) | P2 (%) | P3 (%) | P4(%) | |
|---|---|---|---|---|
| Group NRa | ||||
| Female | 132 (68) | 120 (62) | 155 (80) | 80 (41) |
| Male | 11 (100) | 11 (100) | 8 (79) | 9 (82) |
| Group PRb | ||||
| Female | 0 (0) | 28 (100) | 5 (18) | 2 (1) |
| Male | 1 (17) | 6 (100) | 3 (50) | 1 (17) |
| Group PTc | ||||
| Female | 8 (37) | 22 (100) | 18 (82) | 8 (36) |
| Male | 3 (17) | 18 (100) | 5 (28) | 8 (44) |
aGroup NR comprises the patients that underwent a nasal reshape. bGroup PR comprises the patients treated after a rhinoplasty. cGroup PT comprises the patients treated after a nasal trauma.
RESULTS
A total of 280 patients were enrolled in the study and 12% of the patients were affected by cosmetic imperfections due to previous rhinoplasty, while 88% had no history of surgery or medical procedure at the level of the nose. Table S3 shows the treatment frequency related to the nasal areas divided by groups of patients [Graph S2]. The nasion treatment was performed in 55% of patients and it was more frequent in Group NR while it was almost never carried out to correct postsurgical defects (Group PR). The nasal dorsum and tip were corrected in 73% and 69% of patients, respectively. Note that dorsum correction was performed in 100% of male patients. The subnasal correction was performed in 38% of patients [Table S3 and Graph S2].
The amount of HA filler injected is different for the three Groups [Table S4 and Graph S3]. The average injection volume was 0.62 ± 0.20 cc for nasal reshape (Group NR), 0.50 ± 0.20 cc for correction of minor postsurgical defects (Group PR) and 0.62 ± 0.20 cc for post-trauma patients (Group PT). By specific sites of injections, the average injected volume was 0.20 ± 0.09 cc for the P1 area, 0.23 ± 0.10 cc for the P2 area, 0.17 ± 0.10 cc for the P3 area and 0.20 ± 0.09 cc for the P4 area [Table S4]. The HA quantity used was systematically higher for man as compared to women.
| P1d (cc + SD) | P2d (cc + SD) | P3d (cc + SD) | P4 (cc + SD) | Total (cc + SD) | |
|---|---|---|---|---|---|
| Group NRa | |||||
| Female | 0.20 ± 0.10 | 0.20 ± 0.10 | 0.15 ± 0.10 | 0.20 ± 0.10 | 0.60 ± 0.20 |
| Male | 0.25 ± 0.10 | 0.25 ± 0.10 | 0.20 ± 0.10 | 0.25 ± 0.10 | 0.65 ± 0.20 |
| Group PRb | |||||
| Female | - | 0.20 ± 0.10 | 0.15 ± 0.10 | 0.10 ± 0.10 | 0.40 ± 0.10 |
| Male | 0.15 ± 0.10 | 0.25 ± 0.10 | 0.20 ± 0.10 | 0.20 ± 0.10 | 0.60 ± 0.10 |
| Group PTc | |||||
| Female | 0.20 ± 0.10 | 0.25 ± 0.10 | 0.15 ± 0.10 | 0.20 ± 0.10 | 0.60 ± 0.20 |
| Male | 0.20 ± 0.10 | 0.25 ± 0.10 | 0.20 ± 0.10 | 0.25 ± 0.10 | 0.65 ± 0.20 |
aGroup NR comprises the patients that underwent a nasal reshape. bGroup PR comprises the patients treated after a rhinoplasty. cGroup PT comprises the patients treated after a nasal trauma. dThe reported value is the total HA amount injected e.g. half in each side.
The aesthetic results were evaluated using both a quantitative approach based on angular values [Table S5] and on the self-assessment GAIS scale [Table S6].
| aNFd | aCLd | aNTd | RAd | |||||
|---|---|---|---|---|---|---|---|---|
| Pre (°) | Post (°) | Pre (°) | Post (°) | Pre (°) | Post (°) | Pre (°) | Post (°) | |
| Group NRa | ||||||||
| Female | 128.9 ± 6.3 | 134.1 ± 4.2 | 88.9 ± 9.7 | 100.1 ± 8.2 | 75.1 ± 9.1 | 62.1 ± 5.1 | 11.0 ± 3.2 | 2.0 ± 2.0 |
| Male | 129.5 ± 6.2 | 134.2 ± 5.0 | 87.2 ± 8.5 | 94.8 ± 7.2 | 77.2 ± 8.9 | 65.3 ± 4.2 | 12.1 ± 3.1 | 3.0 ± 2.1 |
| Group PRb | ||||||||
| Female | 133.8 ± 3.1 | 133.8 ± 3.1 | 97.4 ± 5.1 | 101.0 ± 4.1 | 52.4 ± 5.1 | 61.2 ± 4.2 | -2.0 ± 1.5 | 0.3 ± 1.2 |
| Male | 132.1 ± 5.1 | 133.8 ± 3.5 | 89.3 ± 3.2 | 92.4 ± 3.0 | 59.1 ± 3.2 | 63.4 ± 2.1 | 7.4 ± 2.5 | 3.1 ± 2.0 |
| Group PTc | ||||||||
| Female | 129.5 ± 6.1 | 134.0 ± 4.1 | 93.1 ± 5.2 | 99.2 ± 4.0 | 78.3 ± 8.2 | 63.3 ± 4.8 | 8.3 ± 3.1 | 2.5 ± 2.1 |
| Male | 129.8 ± 6.1 | 134.2 ± 5.3 | 87.5 ± 8.5 | 95.1 ± 6.1 | 86.2 ± 6.1 | 72.1 ± 5.1 | 8.2 ± 3.0 | 3.0 ± 2.1 |
aGroup NR comprises the patients that underwent a nasal reshape. bGroup PR comprises the patients treated after a rhinoplasty. cGroup PT comprises the patients treated after a nasal trauma. daNF is the nasal frontal angle, aCL is the columella labial angle, aNT is the nasal tip angle and RA is the rhinion angle.
| Group NRa | Group PRb | Group PTc | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Week 3 N(%) | Month 3 N(%) | Month 6 N(%) | Week 3 N(%) | Month 3 N(%) | Month 6 N(%) | Week 3 N(%) | Month 3 N(%) | Month 6 N(%) | |
| GAIS score (patients) | |||||||||
| Very much improved | 56 (27) | 60 (29) | 58 (28) | 6 (18) | 8 (23) | 7 (21) | 9 (22) | 10 (24) | 10 (24) |
| Much improved | 105 (51) | 113 (55) | 109 (53) | 23 (67) | 22 (65) | 22 (65) | 25 (63) | 25 (63) | 25 (63) |
| Improved | 45 (22) | 33 (16) | 39 (19) | 5 (15) | 4 (12) | 5 (14) | 6 (15) | 5 (13) | 5 (13) |
| No change | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Worse | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| GAIS score (practitioner) | |||||||||
| Very much improved | 41 (20) | 45 (22) | 41 (20) | 6 (17) | 6 (17) | 6 (17) | 8 (20) | 9(22) | 8 (20) |
| Much improved | 134 (65) | 136 (66) | 140 (68) | 19 (56) | 20 (59) | 20 (59) | 26 (65) | 26 (65) | 26 (65) |
| Improved | 31 (15) | 25 (12) | 25 (12) | 9 (27) | 8 (24) | 8 (24) | 6 (15) | 5 (13) | 6 (15) |
| No change | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Worse | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| GAIS score (independent practitioner) | |||||||||
| Very much improved | 35 (17) | 39 (19) | 37 (18) | 5 (14) | 5 (14) | 5 (14) | 6 (15) | 6 (15) | 5 (13) |
| Much improved | 144 (70) | 142 (69) | 144 (70) | 22 (65) | 23 (67) | 23 (67) | 27 (68) | 27 (68) | 26 (65) |
| Improved | 27 (13) | 25 (12) | 25 (12) | 7 (21) | 6 (19) | 6 (19) | 7 (17) | 7 (17) | 9 (22) |
| No change | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Worse | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
aGroup NR comprises the patients that underwent a nasal reshape. bGroup PR comprises the patients treated after a rhinoplasty. cGroup PT comprises the patients treated after a nasal trauma.
Based on our results after treatment the aNF angle value increased on an average by 4.9 ± 3.4° in females and by 3.6 ± 2.4° in males, the aCL value increased on an average by 7.0 ± 4.5° in females and by 6.1 ± 4.2° in males, the aNT value changed on an average by 12.3 ± 5.1° in females and by 10.1 ± 5.0° in males, and the RA value changed on an average by 5.7 ± 1.2° in females and by 6.2 ± 1.8° in males [Table S5]. In all cases an RA value very close to the ideal one was obtained, even if the RA angle was never equal to 0°.
The treatment results were also assessed by two practitioners and patients based on the GAIS score. For Group NR the highest satisfaction levels were reported by the patients, the practitioner, and the independent practitioner in 78%, 85%, and 87% of the cases after three weeks, respectively, and three and sixth months after the treatment they remained unchanged. The lowest satisfaction levels were never reported thus meaning that in 100% of the cases an improvement of the nasal appearance was obtained. A very similar result has been obtained for Group PS and PT.
A first follow-up is done at 3 weeks and after possible corrections in one or more points the result is stable up to 6 months in 100% of the cases. In most patients, the duration effect was more than one year after treatment with good satisfaction of both the patient and the practitioner, and in 38% of patients the duration was longer than 2 years.
No major complications such as vascular occlusion, infections or granulomas were observed. No cases of skin necrosis or skin loss were observed. However, mild persistent tip erythema occurred in 5% of patients all belonging to phototype I and II, and all cases resolved after 20 days using each night a zinc oxide-based cream.
In the presence of low dorsum and underprojected tip the HA filler is usually injected in the P1, P2 and P3 areas [Figure 2] even if in some cases all the four regions are corrected [Figure 3]. In the presence of a short nose the P3 area is treated, and a larger amount of HA (up to 0.5 cc) can be necessary. Patients that underwent surgical rhinoplasty usually need to improve imperfections in the nasal dorsum (for example V deformity) and in this case the P2 area is corrected. In post-traumatic patients, nasal deviations are usually present and the P2 area is treated to reach a symmetric nose in frontal vision [Figure 4]. In some patients, many injections are delivered in several points to correct nasal asymmetries and deviations [Figure 5]. In the presence of a nose with hanging wings or/and retracted columella an improvement is obtained by injecting the filler in the columella.
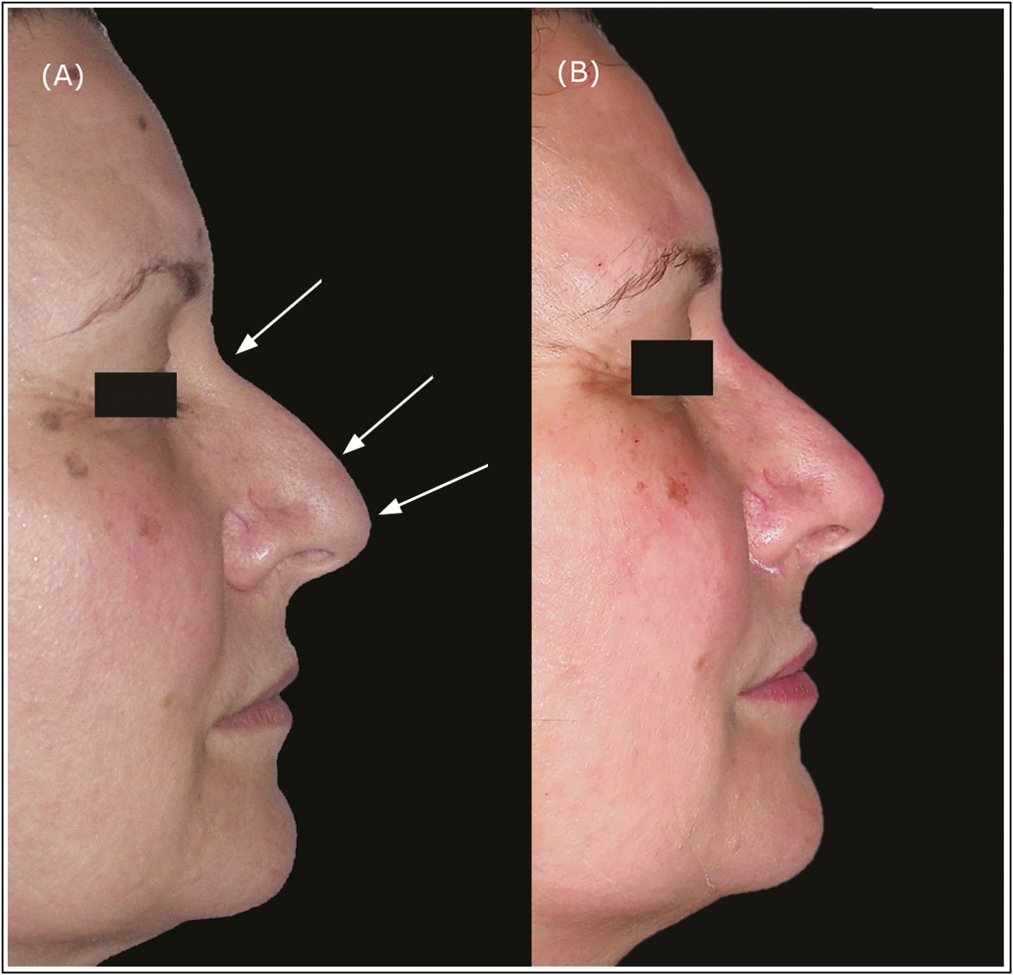
- A 52-year-old woman. Lateral view of hook nose (A) before and (B) immediately after injection of 0.2 cc of HA in P1, 0.1 cc in P2, and 0.25 cc in P3. After filler reshaping the hook nasal profile has improved
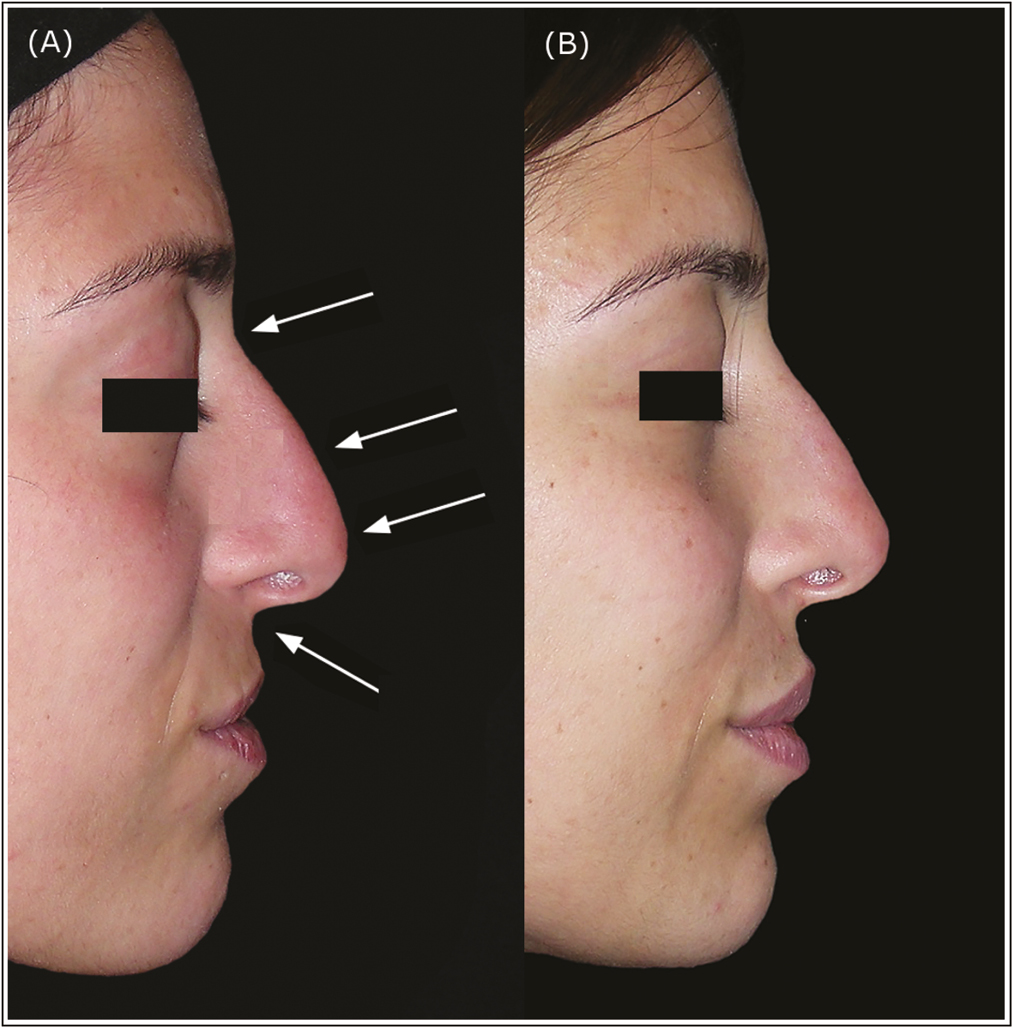
- A 29-year-old woman. Lateral view of hook nose (A) before and (B) 6 months after injection of 0.15 cc of HA in P1, 0.1 cc in P2, 0.20 cc in P3, and 0.1 cc in P4. After filler injections the nasal profile has improved. Also the upper lip has been corrected
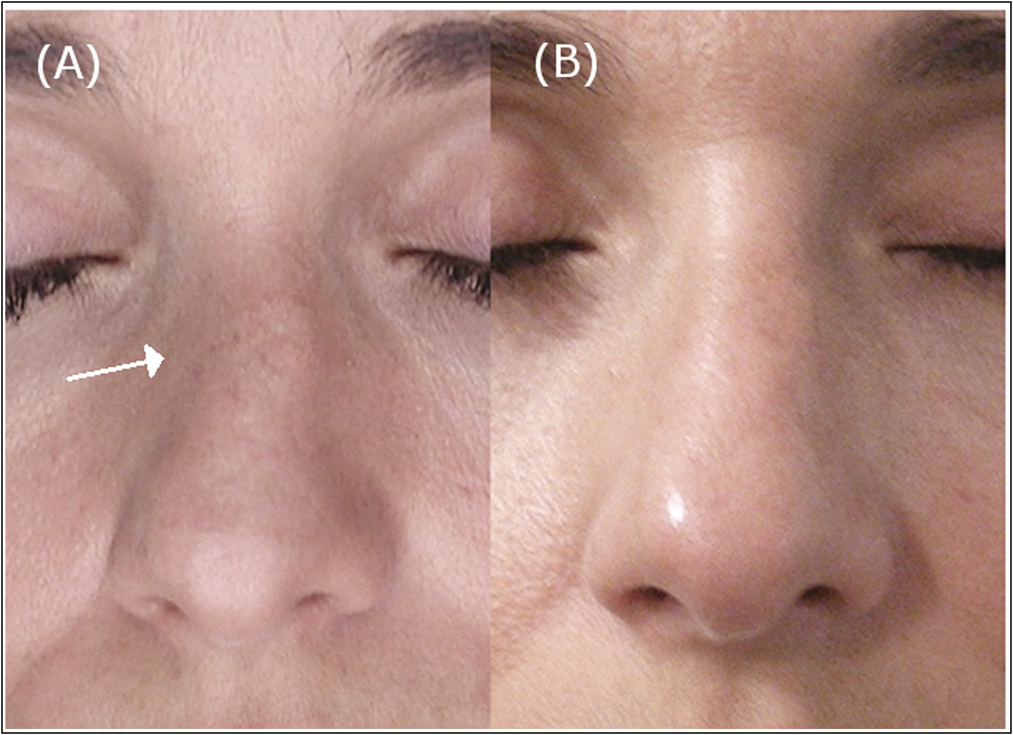
- A 40-year-old woman. Frontal view of (A) pre-operative and (B) post-operative situation 6 months after injecting 0.4 cc of HA in P2 in the right side and 0.1 cc of HA in P2 in the left side . The nasal axial deviation has been improved
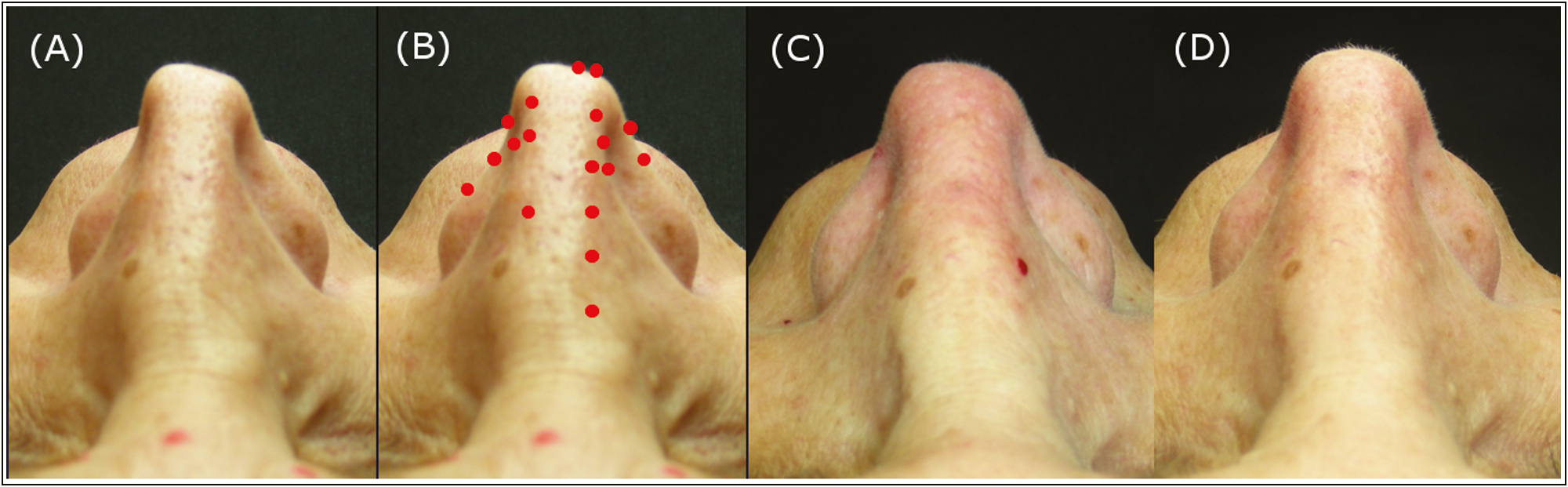
- A 51-year-old woman. Above view of pre-operative situation (25 years after surgical rhinoplasty (A), injection points (B), immediately after injection (C) and post-operative situation 6 months after injecting 0.6 cc of HA in total. There is an improvement of the pinched tip due to the previous rhinoplasty and a reshaping of the alar rim
DISCUSSION
Nonsurgical rhinoplasty is used worldwide to improve the appearance of the nose and in the usual approach the nasal reshaping is carried out by injecting the HA filler directly onto the bone[1] and this procedure may give rise to several complications including vascular embolism and necrosis, ocular ischemia, vision loss, and infection.[14151617] According to Park and Kim the nose is the third most common site for filler-induced blindness (23% of all cases).[15] The vasculature of the nose is peculiar as it is derived from both the internal and carotid artery system and any filler material that is inadvertently injected into a nasal blood vessel can be propelled retrogradely into the orbit and occlude the ophthalmic artery causing visual compromise.
In this study, the author demonstrates the efficacy of an innovative approach that is carried out by injecting HA into the dermis. In the author’s experience, this is a safer and more versatile approach that enables the practitioner to carry out a more precise nasal reshaping. This is a seven-point injection technique that allows one to deliver targeted interventions ensuring a satisfactory result. This is confirmed by the improvement of the aNF, aCL, aNT, and RS angles after filling, and by the significantly high satisfaction scores obtained in all cases based on the GAIS scale.
In this work, only cases of Caucasian patients are presented, but the proposed procedure can be extended to Asian subjects following the same procedure. Usually, Asian patients have noses with bulbous tips that can be effectively projected into two points in correspondence with the domal crura in such a way to obtain a better tip projection. In the case of low dorsum, which is typical of Asian patients, it can be redefined in the lateral dorsal lines by connecting the nasion with the nasal tip.
No serious complications have occurred in the 280 patients treated by the author. Overfilling should be avoided because of the risk of serious complications and if vascular compromise is suspected the physician should always be prepared to treat with hyaluronidase following the protocol suggested by DeLorenzi.[16]
The duration of the effect is longer in the nose than in the nasolabial folds and this may be due to the minimal muscular activity of the nose and to a different metabolic activity as compared to nasolabial folds and lips. In the case of an extremely thin dermis and in the presence of a subdermal cartilaginous spur it is possible to improve the dermis thickness using an intradermal injection [Figure S4]. In this case only the tip of a short and thin needle must be inserted with the tip opening facing upwards, but the rheology of the filler used is always the same.
The advantages of using fillers in the nose are the ability to correct a deformity without anesthesiological risk, the reduction of costs and downtime as compared with surgical rhinoplasty. Disadvantages include potential damage of the nasal skin envelope and the need for serial treatments to maintain correction. Moreover, corrections that aim to reduce bone, cartilaginous or soft tissue structures are not possible with this method.
CONCLUSIONS
Injecting HA fillers in the dermal layer is a versatile approach that provides very satisfactory results. This technique allows one to better correct aesthetical, post-traumatic, and post-surgical defects compared with the usual injection rhinoplasty procedures where the filler is injected deep onto the bone/cartilage in the midline of the nose. According to us, this a safer procedure that could become the method of choice for nose reshaping when functional problems need not to be corrected.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Graph S1
Graph S1 Number of patients based on patient’s gender and groupGraph S2
Graph S2 Percentage of treatments in the three Groups for each nasal region, nasion (P1), nasal dorsum (P2), nasal tip (P3), and subnasal (P4) and patient’s genderGraph S3
Graph S3 Average amount of HA filler (cc) in the three Groups for each nasal region, nasion (P1), nasal dorsum (P2), nasal tip (P3), and subnasal (P4) and patient’s genderFigure S1
Figure S1 Definition of the nasal frontal angle aNF (A), of the rhinion angle RA (B), of the columella labial angle aCL (C), and of the nasal tip angle aNT (D) used for pre and post treatment evaluationFigure S2
Figure S2 View of the nose skin layers during oncoplastic surgery of the nasal pyramid. The thickness of the dermis and the location of two blood vessels are clearly detectable (A). The thickness of the dermal layer is of few millimeters (B)Figure S3
Figure S3 Injection technique: the needle is inserted at less than a 10 degree angle and its trajectory is almost parallel to the skin surface (A). By tilting the needle its tip can be seen (B) and during and after the injection a white area appears for few seconds (C)Figure S4
Figure S4 A 58-year-old woman with an extremely thin dermis and a subdermal cartilaginous spur in the left side of the nose. Above view of pre-operative situation (A) pre-operative and (B) post-operative situation 6 months after injecting 0.2 cc of HA in P3 in the left side. Frontal view of pre-operative situation (C) preoperative and (D) postoperative situation. The nasal axial deviation has been improvedREFERENCES
- Update on injectables in the nose. Curr Opin Otolaryngol Head Neck Surg. 2017;25:307-13.
- [Google Scholar]
- Profiloplasty in one session versus single treatment areas. Dermatol Surg. 2021;47:953-8.
- [Google Scholar]
- Injection rhinoplasty using filler. Facial Plast Surg Clin North Am. 2018;26:323-30.
- [Google Scholar]
- Nasal reshaping with hyaluronic acid: An alternative or complement to surgery. Plast Reconstr Surg Glob Open. 2016;4:e1120.
- [Google Scholar]
- Restoration of the face covering by means of selected skin in regional aesthetic units. Br J Plast Surg. 1956;9:212-21.
- [Google Scholar]
- The paramedian forehead flap: A dynamic anatomical vascular study verifying safety and clinical implications. Plast Reconstr Surg. 2008;121:1956-63.
- [Google Scholar]
- Oriental nose: An anatomical basis for surgery. Ann Acad Med Singa. 1992;21:176-89.
- [Google Scholar]
- Safe planes for injection rhinoplasty: A histological analysis of midline longitudinal sections of the Asian nose. Aesthetic Plast Surg. 2016;40:236-44.
- [Google Scholar]
- Evaluation and proportion in nasal filling with hyaluronic acid. J Clin Aesthet Dermatol. 2018;11:36-40.
- [Google Scholar]
- Early changes in facial profile following structured filler rhinoplasty: An anthropometric analysis using a 3-dimensional imaging system. Dermatol Surg. 2017;43:255-63.
- [Google Scholar]
- Filler rhinoplasty evaluated by anthropometric analysis. Dermatol Surg. 2016;42:1071-81.
- [Google Scholar]
- Delayed paleness after hyaluronic acid filler injection: A warning sign of vascular compromise. Dermatol Surg. 2018;44:590-2.
- [Google Scholar]
- Iatrogenic occlusion of the ophthalmic artery after cosmetic facial filler injections: A national survey by the Korean Retina society. JAMA Ophthalmol. 2014;132:714-23.
- [Google Scholar]
- Complications of injectable fillers, part 2: Vascular complications. Aesthet Surg J. 2014;34:584-600.
- [Google Scholar]
- Nonsurgical rhinoplasty using injectable fillers: A safety review of 2488 procedures. Facial Plast Surg Aesthet Med. 2021;23:6-11.
- [Google Scholar]






