Translate this page into:
An Uncommon Cause of Pincer Nail
Address for correspondence: Dr. Chander Grover, Department of Dermatology and STD, University College of Medical Sciences and GTB Hospital, Dilshad Garden, Delhi-110095, India. E-mail: chandergroverkubba76@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Pincer nail is a deformity characterized by excessive transverse curvature of nail, progressively increasing along its longitudinal axis. The curvature is greatest at the distal end, leading to an ingrown nail, producing pain, discomfort, and significant cosmetic alteration. It is a severe variant of ingrown nail, often attributed to causes such as anatomical variation of nail plate axis, tight footwear, gait abnormalities, and so on. Correspondingly, its management involves the removal of the lateral ingrowing nail plate or the lateral hypertrophic nail folds. We report a young male who presented with symptomatic pincer nail deformity. However, on exploration there was a midline onychomatricoma, leading to the thickening of the central part of the nail plate, causing incurving of the lateral nail plate and discomfort. The report serves to highlight the need for a comprehensive evaluation of pincer nails, to assess for matrix disease as well, because the surgical approach will differ accordingly.
Keywords
Central nail plate
lateral nail plate
onychomatricoma
onychoscopy
INTRODUCTION
Pincer nail is a term used for an excessively curved nail plate, impinging on both the lateral nail folds. This excessive curvature is much more pronounced at the distal end,[1] causing a pinching up of the distal nail bed which can be very symptomatic. Depending on the type of distal curvature, three types of pincer nails have been identified. Omega nail is an arched nail, which is almost trumpet-shaped.[1] A plicated nail is characterized by the ingrowing of one nail plate end more than the other, while a tile-shaped nail has sharply bent lateral ends.
The excessive curvature of the distal nail plate has been attributed to hereditary as well as acquired causes.[2] It has been proposed that an imbalance between an upward mechanical force on the nail plate due to walking and a downward force due to automatic curvature of the growing nail plate results in the pincer nail. However, a nail matrix tumor as a cause of pincer nail has not been reported previously, to the best of our knowledge. We report an interesting case of onychomatricoma-induced pincer nail deformity to highlight the need for an alternative surgical management approach.
CASE REPORT
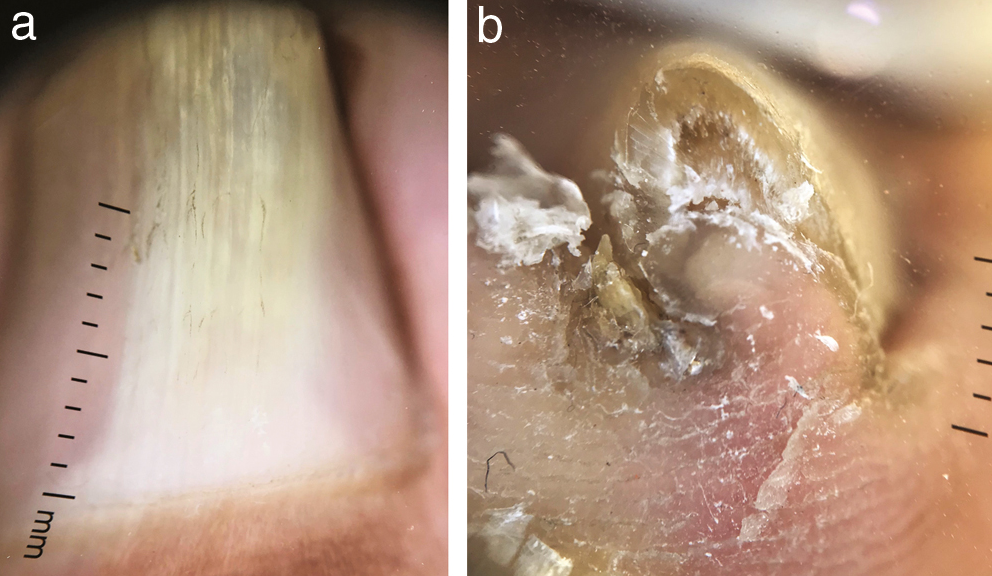
A 29-year-old male presented with a painful left great toenail. There was no history of preceding trauma, drug intake, diabetes, or peripheral loss of sensation. On examination, the toenail was excessively curved distally and painful on pressing at the distal end, where there was fissuring as well. Distally, a plicated morphology was seen, with a pinched-up nail bed and a fissure in the lateral nail fold [Figure 1a]. The lateral edges of the nail plate were translucent and normal in thickness but were embedded into the surrounding soft tissue (lateral folds) causing tenderness over nail folds. However, the central part of the nail plate was thickened, whitish, and opaque. This broad central zone of leukonychia was accompanied by subungual hyperkeratosis at the distal end [Figure 1b].

- (a,b) Thickened nail plate distally showing a plicated nail morphology with a fissure in the lateral nail fold. Dorsally, the nail plate shows a broad central zone of leukonychia with a distal increase in transverse curvature
Onychoscopic examination revealed a linear broad band of leukonychia with whitish-grey channels running through the nail plate [Figure 2a]. There was no evidence of any splinter hemorrhages. The distal edge of the thickened nail plate showed compact subungual hyperkeratosis, with a few cavities identified [Figure 2b].
- (a,b) Linear broad band of leukonychia with whitish-grey channels running through the nail plate. The distal edge of the thickened nail plate shows compact subungual hyperkeratosis, thickened nail plate, with few cavities identified dorsally (Dermlite DL4×x10 polarized)
Direct microscopy and fungal culture from distal nail plate clippings were negative for any fungal elements. Digital X-ray revealed a thickened nail plate, with a normal underlying phalanx, while MRI revealed mild thickening of the nail bed, subungual swelling, and absence of any nail plate deformity. Due to a suspected matrix growth, surgical management was planned with central hemiavulsion of the nail plate rather than lateral partial nail avulsion. This revealed a tumor with papillary projections underneath the affected part of the nail plate. Intraoperative onychoscopy revealed regularly arranged hyperbolic crypts with a few filiform projections in the proximal part of the ventral aspect of the nail plate [Figure 3]. Histopathologic examination of the removed matrix growth revealed both epithelial and stromal components with epithelial strands originating from the nail matrix, penetrating vertically into the stroma. Features were suggestive of an onychomatricoma [Figure 4]. Sagittal sections through the nail plate did not reveal epithelium-lined cavities.
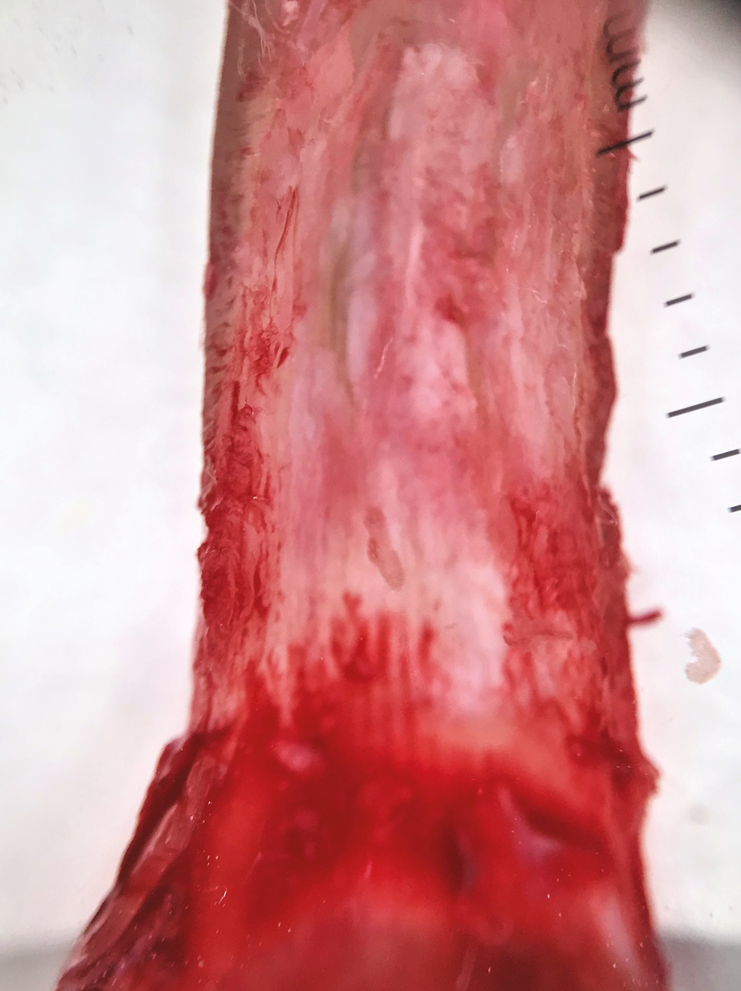
- Intraoperative onychoscopy revealed regularly arranged hyperbolic crypts with few filiform projections, seen in the proximal part of the ventral aspect of the nail plate (Dermlite DL4 × 10 polarized)
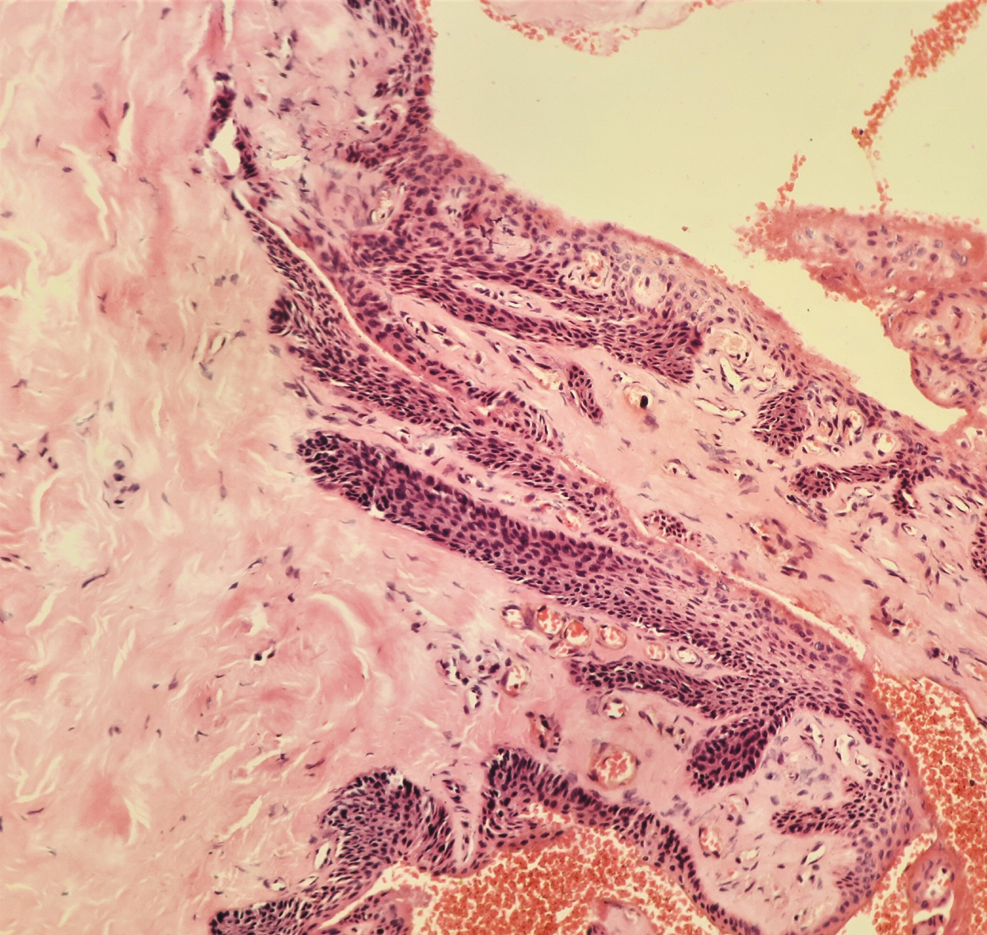
- H&E showed both epithelial and stromal components. Epithelial strands originating from the nail matrix were seen to be penetrating vertically into the stroma, suggestive of an onychomatricoma (H&E 400×)
DISCUSSION
The pincer nail is a relatively common nail deformity, characterized by a thickened, excessively curved nail plate impinging on both lateral nail folds. With an incidence of around 0.9%, it commonly affects the great toenails.[3] Occasionally, fingernails may be affected. The transversally over-curved nail plate impinges into the lateral nail folds causing severe pain, chronic infections, and hampering day-to-day activities. Hence, surgical management of pincer nail involves lateral partial avulsion of the impinging nail plate combined with lateral partial matricectomy.[4] We describe this interesting case where the central part of the nail plate was causing the pincer nail deformity, and was dealt with accordingly. This report highlights the need for pre-planning surgical management of pincer nail.
Pincer nail is a clinical diagnosis. Hereditary pincer nails exhibit symmetry and autosomal dominant inheritance,[5] whereas acquired cases are usually asymmetrical. Known causes of the acquired pincer nail include ill-fitting shoes, nail psoriasis, repeated trauma, nail avulsion, developmental abnormalities, infections such as onychomycosis, medications such as beta-blockers, protease inhibitors, retinoids, and subungual exostosis. Systemic disorders such as renal failure, gastrointestinal malignancies, systemic lupus erythematosus, and Kawasaki disease are also known to be associated.[678] However, to the best of our knowledge, nail matrix tumors including onychomatricoma have not been attributed as a cause of pincer nail deformity. Onychomatricoma is a rare neoplasm of the nail matrix producing a localized or diffuse thickening of the nail plate with yellowish discoloration, splinter hemorrhages, transverse overcurvature of the nail plate with perforations consisting of multiple longitudinal channels, creating “woodworm” cavities containing tumor digitations. Such an outcome can be explained by an increased volume of the proximal tissue produced by the nail matrix filiform growth, reducing the proximal overcurvature.[910] This correspondingly causes an increased distal curvature. The thickening of the central nail plate leads to the lateral edges being pulled, resulting in soft tissue embedding.
Diagnosis of the pincer nail is clinical and the dermatologist needs to carefully examine all the parts of the nail unit, including the matrix. In our patient, an augmented examination with onychoscopy revealed features suggestive of onychomatricoma. Histopathological features of onychomatricoma are distinctive consisting of two distinct zones: a fibroepithelial tumor composed of a proximal pedunculated base and a distal zone with multiple projections. The stroma also has two zones in the form of a collagenous and fibroblastic superficial coat and a deeper coat with less cellularity and thickened collagen. Immunohistochemistry for cytokeratins 5 and 14 is positive along with K6, K16, K17, K75, and CD34.[910] Though radiological investigations have been reported to be diagnostic, showing the tumoral core in the matrix (low-intensity signals) with invaginations into the funnel-shaped nail plate, in our case, the diagnosis could not be confirmed on MRI, probably because this was an early lesion with less well-defined nail plate invasion. Surgical hemiavulsion of the central nail plate revealing a filiform matrix tumor confirmed our diagnosis.
Management of the pincer nail is largely conservative. However, for symptomatic nails, treatment of the primary cause, surgical correction of the curved nail plate, or a combination of both approaches is recommended.[15] In our case, since a centrally placed onychomatricoma was causing the deformity, an in-toto removal of the tumor was performed relieving the symptoms with no intervention being implemented for the lateral ingrowing nail plate edges. Onychomatricoma once surgically removed in toto has least chances of recurrence.[910]
This report serves to highlight onychomatricoma as an unusual cause of pincer nail deformity. The need for planning surgical treatment keeping in mind whether the lateral nail or the central nail is responsible for pincer deformity is reinforced.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Author Contributions
CG contributed to the concept, definition of intellectual content, data acquisition, patient management, and data analysis. SY prepared the first draft of the article and contributed to the definition of intellectual content and patient management. RG contributed toward clinicopathological correlation and histopathological diagnosis. All authors edited and reviewed the article. CG act as guarantor.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
None of the authors report any form of support and financial involvement.
There are no non-financial relationships (personal, political, or professional) that may potentially influence the writing of the manuscript.
REFERENCES
- Surgical pearl: Nail plate separation and splint fixation--A new non-invasive treatment for pincer nails. J Am Acad Dermatol. 2003;48:791-2.
- [Google Scholar]
- Surgical treatments for ingrowing toenails. Cochrane Database Syst Rev. 2005;2:CD001541.
- [Google Scholar]
- Pincer nail deformity: Clinical characteristics, causes, and managements. Biomed Res Int 2020:2939850.
- [Google Scholar]
- Pincer nails in a patient with systemic lupus erythematosus and lupus nephritis: A case report. JAAD Case Reports. 2016;2:233-5.
- [Google Scholar]
- Clinical evidence for the relationship between nail configuration and mechanical forces. Plast Reconst Surg. 2014;2
- [Google Scholar]
- Onychomatricoma: A rare tumor of nail matrix. Annals of dermatology. 2016;28:237-41.
- [Google Scholar]
- Onychomatricoma: New clinical and histological features. A review of 19 tumors. Am J Dermatopathol. 2010;32:1-8.
- [Google Scholar]






