Translate this page into:
An Unusual Case of Neonatal Perianal Lesion and Its Management
Address for correspondence: Dr. Jayalaxmi Shripati Aihole, Department of Pediatric Surgery, Indira Gandhi Institute of Child Health, Bengaluru 560029, Karnataka, India E-mail: jaihole4@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Infantile hemangiomas (IHs) are common vascular tumors occurring in infants. The IHs have a characteristic natural course. Most of the uncomplicated IHs undergo spontaneous involution, with a small proportion of cases requiring intervention. Perianal hemangiomas are rarely reported in infants.
Keywords
Capillary hemangiomas
excision
perianal
INTRODUCTION
The IHs have the unique ability to involute after proliferation, often leading primary care providers to assume that they will resolve without intervention or consequence. A few of the IHs rapidly develop complications, resulting in pain, functional impairment, or permanent disfigurement. Perianal hemangiomas, as such, are rare and their management is also varied.
CASE REPORT
A two-month-old male baby born to primigravida, by a full-term cesarean section without any antenatal issues and having a birth weight of 3kg, was brought to us with a history of perianal ulcerative lesion that was noticed after one week of his birth. The lesion was initially tiny and then gradually progressed to its present size of 2 cm x 1 cm on the right side of the perianal region at the 7oo clock position [Figure 1A]. The baby was clinically stable, had an oval shaped 2 cm x 1 cm non-bleeding, non-infected, ulcerative lesion having pale pink granular mucosa over it, situated on the right side of the perianal region close to the anal canal [Figure 1A]. The baby had undergone normal endocrinological and genetical evaluation, normal sonolography, and 2D echocardiography. The baby had also undergone an uneventful yet complete excision of the perianal lesion under general anesthesia, and it resulted in a wound of 2 cm x 1 cm that was closed primarily [Figures 1B–D, and 2E]. The histopathology examination revealed it to be a capillary hemangioma exhibiting capillary proliferation in a lobular pattern with chronic inflammatory cell infiltrates [Figure 2F,G] The wound healed well, and the baby was doing well for a year of follow-up [Figure 2H].
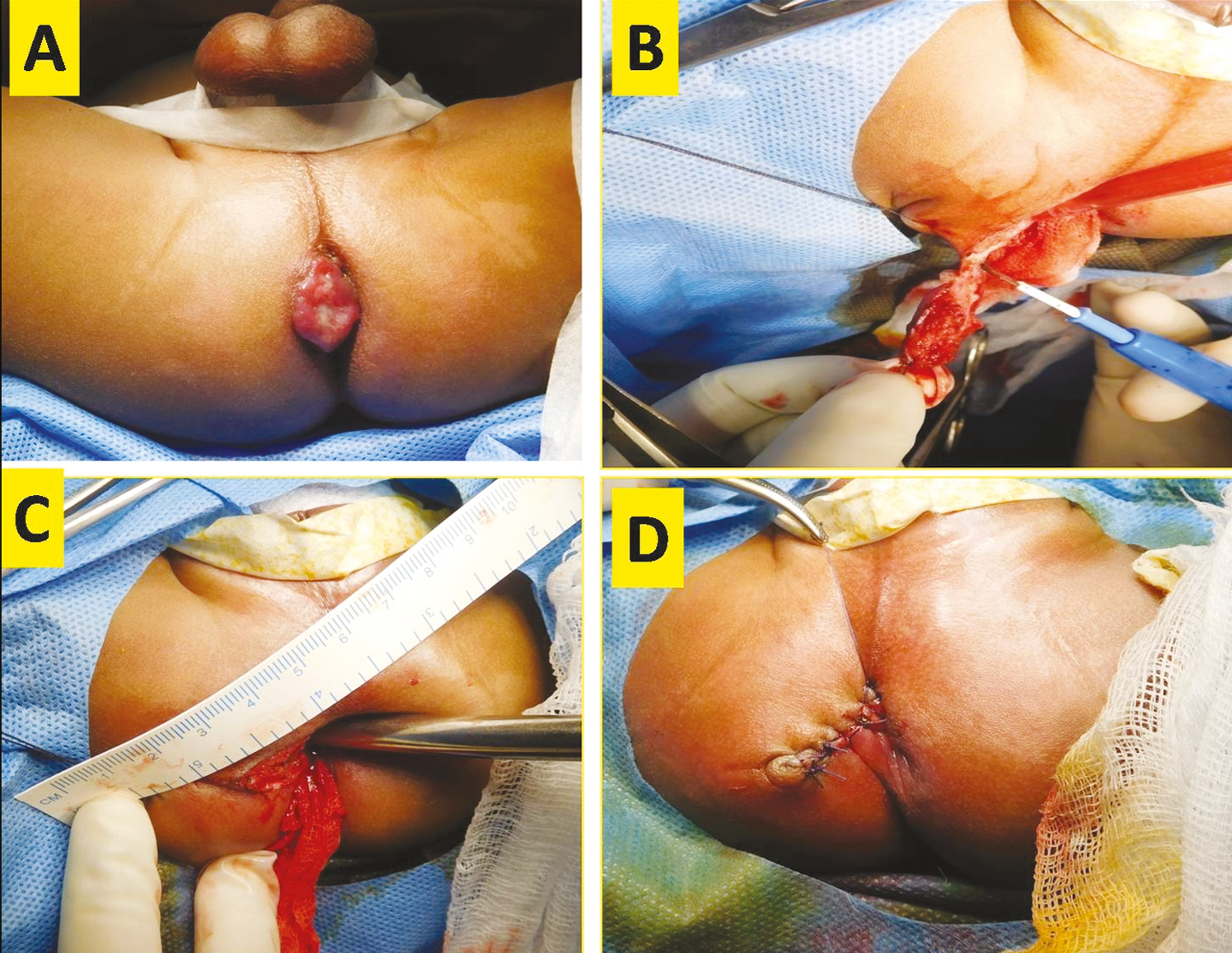
- (A) Clinical appearance of right-sided perianal ulcerative oval lesion. (B and C) Intraoperative picture showing excision of perianal lesion. (D) Wound closed after excision

- (E) Excised lesion of size 2 cm × 1 cm. (F and G) Histopathological images. (F) Low power field (10×) and (G) high power view (40×) capillary proliferation in lobular pattern with chronic inflammatory infiltrates. (H) Postoperative follow-up picture
DISCUSSION
Originally described by Mulliken and Glowacki in 1982, capillary hemangiomas most commonly occur in the head and neck region (60%); however, they can occur anywhere in the body. The IHs are lesions that are characterized by abnormal proliferation of endothelial cells and aberrant blood vessel architecture. The various risk factors suggested include female gender, prematurity, low birth weight, multiple pregnancies, advanced maternal age, and in vitro fertilization.[123]
Most hemangiomas begin their proliferative (growth) phase shortly after birth. This phase usually lasts for four to six months; however, phases can be either longer or shorter. The involutive phase is much slower; it can last as long as 10 years and it is difficult to predict how long this phase of the shrinkage process will last. In some children, those hemangiomas that do shrink completely may leave residual fatty tissue and telangiectasias (tiny dilated blood vessels) of the skin.[345]
Hemangiomas can have associated pain, bleeding, ulceration, and infection if left untreated or even on medical treatment. Specific locations at a higher risk of ulceration include the head, neck, perioral and perineal/perianal regions, and intertriginous sites. The neck and anogenital regions can sustain maceration and friction, which may contribute to the development of ulceration.[345]
Various treatment options have been suggested, which include close monitoring, compression garments, medications, surgery, laser therapy, sclerotherapy, embolization, or a combination of therapies.[45]
The other possible treatment modes adopted are interferon, vincristine, and cyclophosphamide reserved for life-threatening hemangiomas that are unresponsive to conventional therapy; apart from topical b-blockers, steroids, immune modulators, as well as pulsed dye laser have been adopted, especially in perianal hemangiomas.[345]
Though various treatment options have been suggested for perianal hemangioma, their response to a particular mode of treatment and their duration have been unpredictable; even after response, they leave behind unacceptable cutaneous marks.
This slowly growing infantile perianal lesion noticed since 1 week of life, presented with one episode of bleeding from the lesion, causing anxiety amongst parents as well as relatives, making it difficult to maintain perianal hygiene; hence author planned primary surgical excision of the lesion for its definitive management with valid consent.
The author would like to suggest an option of primary surgical excision for well localised hemangiomas in a tertiary care paediatric center by a pediatric surgeon, which can yield excellent results, along with cosmesis [Figure 2H], hence avoiding a lengthy unpredictable and sometimes unfavourable responses to medical management on the overall growth of children.
As per the author’s literature search, surgical excision as a primary mode of treatment for infantile perianal capillary hemangioma has not been published; in view of its rarity, the case has been reported here.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Hemangiomas and vascular malformations in infants and children: A classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69:412-22.
- [Google Scholar]
- Management of hemangioma of infancy: Review of 245 patients. Plast Reconstr Surg. 1997;99:1301-8.
- [Google Scholar]
- Clinical practice guideline for the management of infantile hemangiomas. Pediatrics. 2019;143:e20183475.
- [Google Scholar]
- Ulcerated hemangiomas: Clinical characteristics and response to therapy. J Am Acad Dermatol. 2001;44:962-72.
- [Google Scholar]






