Translate this page into:
Arterio-venous malformation masquerading as lymphangioma circumscriptum managed with embolization
*Corresponding author: Biju Vasudevan,Department of Dermatology, Armed Forces Medical College, Pune, Maharashtra, India. bijuvasudevan1975@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhatt S, Pandey S, Vasudevan B, Paliwal G, Bhanu KU, Priya S. Arterio-venous malformation masquerading as lymphangioma circumscriptum managed with embolization. J Cutan Aesthet Surg. doi: 10.25259/jcas_52_23
Abstract
Lymphangioma circumscriptum and peripheral arteriovenous malformations (AVM) are both conditions that commonly present during adolescence as an enlarging lesion with occasional oozing and bleeding. Lymphangioma circumscriptum though is unlikely to cause any serious life-threatening complication whereas an expanding AVM can lead to complications like high output cardiac failure. Furthermore, while lymphangioma circumscriptum can be treated easily with sclerotherapy or excision, AVM requires a multi-modality treatment including a combination of endovascular approaches, surgery, and sclerotherapy. Here, we discuss the case of a boy who presented to us with such lesions over the left inguinal region of two months duration. Clinically and dermoscopically, the lesions were indistinguishable from that of lymphangioma circumscriptum but histopathology and radiology revealed an underlying AVM from the circumflex femoral vessels. The patient was subsequently managed with glue embolization.
Keywords
Arterio-venous malformation
Lymphangioma circumscriptum
Glue embolization
INTRODUCTION
Lymphangioma circumscriptum and peripheral arteriovenous malformations (AVMs) are both disorders that present during adolescence with an expanding lesion and can create diagnostic confusion, especially in the early stages, due to clinical and dermoscopic similarities. Appropriate radiological investigation helps to clinch the diagnosis in such patients and prevents unnecessary surgical mishaps of unplanned operative blood loss.
CASE REPORT
A 12-year-old boy with no known comorbidities presented with complaints of developing multiple asymptomatic skin-colored to erythematous papules coalescing to form plaques over the left inguinal region for the past 2 months [Figure 1a and 1b]. The local temperature over the lesion was increased. No palpable thrill was noted. Dermoscopy revealed multiple lacunae with pale septa suggestive of lymphatic proliferation [Figure 2]. Based on the clinical and dermoscopic examination, a working diagnosis of lymphangioma circumscriptum was reached, and he was further investigated along those lines.
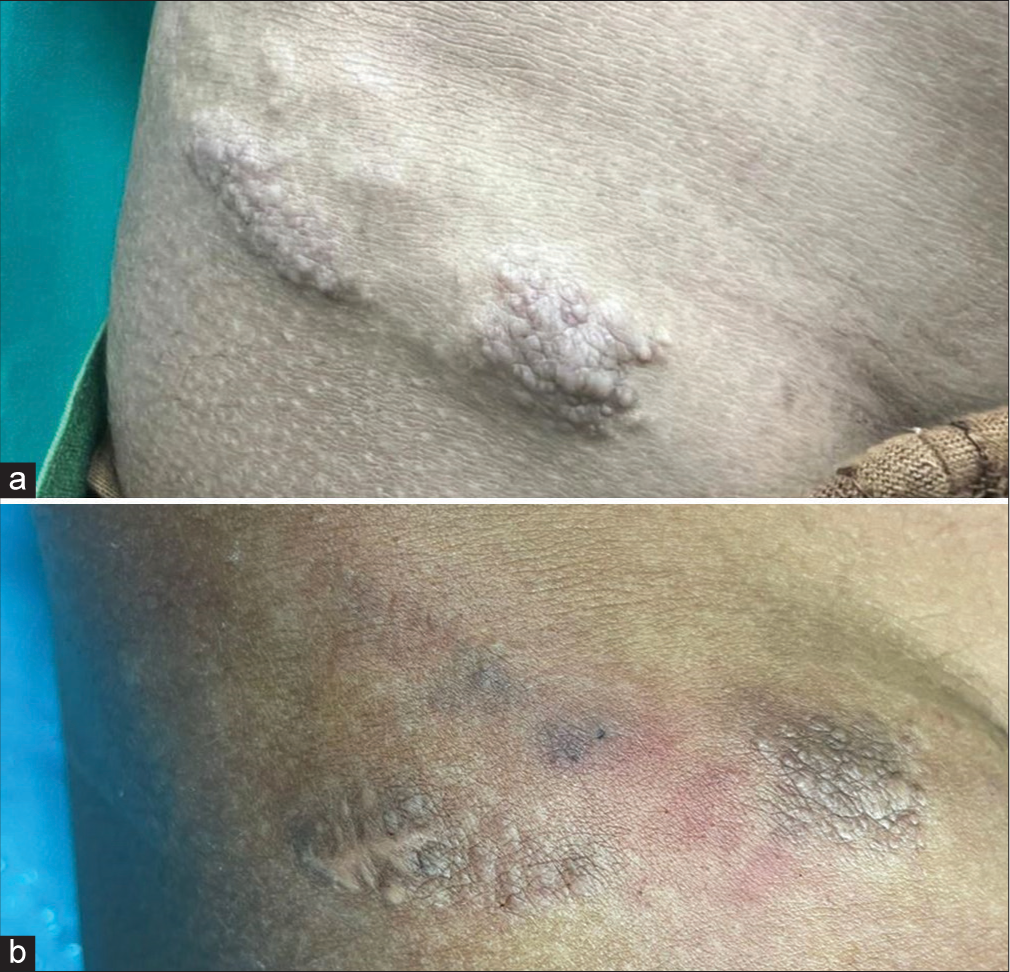
- (a) Multiple skin-colored to erythematous papules coalescing to form plaques over the right inguinal region. (b) Patient follow-up image after the second session of embolization therapy.
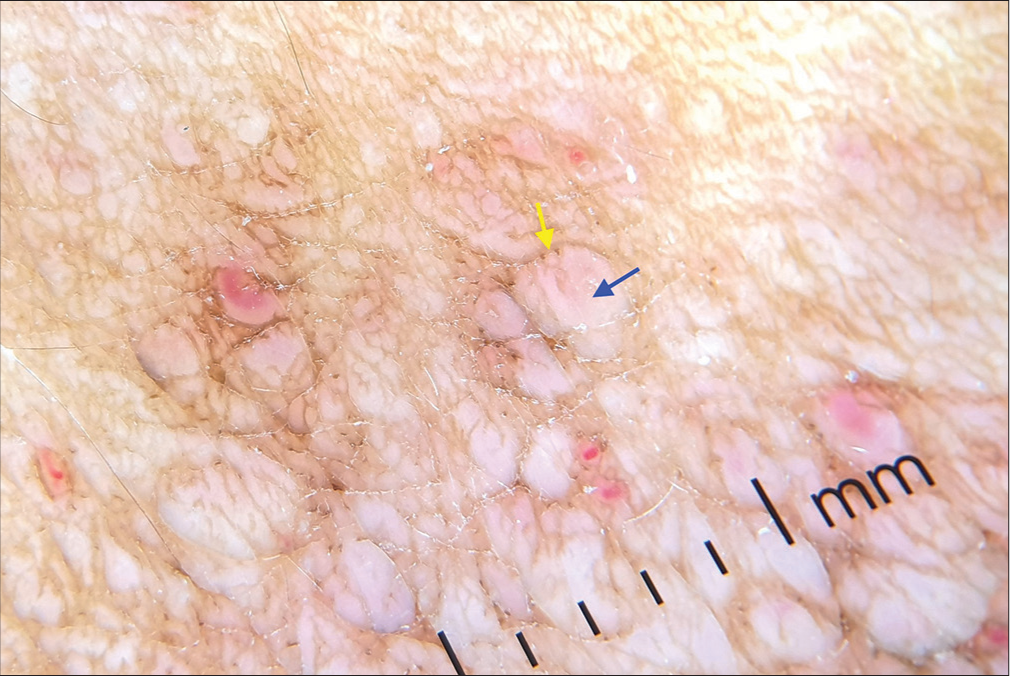
- Multiple lacunae (blue arrow) with pale septa (yellow arrow).
Histopathological examination revealed numerous proliferating convoluted blood vessels in a collagenous stroma with areas of hemorrhage over normal-looking dermal adnexa [Figure 3a and b]. Immunohistochemistry with CD 34 showed increased uptake, and D2-40 showed decreased uptake over the vascular channel [Figure 3c and d]. Ultrasonography revealed a lesion in the cutaneous plane with multiple tortuous serpiginous areas showing both arterial and venous waveforms suggestive of high-flow vascular malformation.
![(a) Hematoxylin and eosin [H&E], ×40): The epidermis and the adnexa show normal histomorphology with numerous proliferating blood vessels (yellow arrow) with areas of hemorrhage seen in the collagenous stroma of the dermis. (b) (H&E, ×400): The proliferating blood vessels show a single layer of endothelium in the collagenous stroma. (c) The immunohistochemistry with CD 34 showed increased uptake and (d) D2-40 showed decreased uptake over the vascular channels.](/content/173/2024/0/1/img/JCAS-52-23-g003.png)
- (a) Hematoxylin and eosin [H&E], ×40): The epidermis and the adnexa show normal histomorphology with numerous proliferating blood vessels (yellow arrow) with areas of hemorrhage seen in the collagenous stroma of the dermis. (b) (H&E, ×400): The proliferating blood vessels show a single layer of endothelium in the collagenous stroma. (c) The immunohistochemistry with CD 34 showed increased uptake and (d) D2-40 showed decreased uptake over the vascular channels.

- Contrast-enhanced computed tomography showing intensely enhancing lesion in the anterolateral aspect of the proximal thigh with arterial and venous drainage from the right circumflex femoral artery and vein.
Contrast-enhanced magnetic Resonance imaging (MRI) showed multiple serpiginous channels within the lesion that were hyperintense on T2W images and hypointense on T1W images. Computed tomographic angiography showed an avidly enhancing nidus in the anterolateral aspect of the proximal thigh. The feeding artery was seen arising from the superficial circumflex branch of the right femoral artery, and the venous drainage was into the right femoral vein [Figure 4]. Based on the clinical and investigative findings, a diagnosis of AVM was reached, and the patient was referred to an interventional radiologist for embolization therapy.
The patient was planned for serial percutaneous glue embolization of the nidus at monthly intervals. There was a marked resolution of the malformation at the end of 2 months.
DISCUSSION
Lymphangioma circumscriptum is a benign microcystic malformation of the lymphatics characterized by multiple clusters of pink, red, or skin-colored fluid-filled lesions, giving it a characteristic frog spawn appearance on clinical examination. It most commonly occurs due to a developmental defect in the superficial lymphatics, with a typical history of having a small number of vesicles at birth that gradually increase in size and number at puberty. Acquired variants of lymphangioma circumscriptum can occur at any age due to architectural destruction of the normal lymphatics resulting from trauma, surgery, radiation, etc.1 Dermoscopically, lymphangiomas are characterized by two kinds of structures: First, multiple yellow-colored lacunae with pale septa and second, dark red or blue lacunae due to the inclusion of blood.1 Treatment modalities include sclerotherapy, electrofulguration, CO2 laser ablation, and cryotherapy.2
AVMs are high-flow, low-resistance lesions resulting from an abnormal connection between the arterial and venous systems with an absent intervening capillary network. These are usually present since birth but become clinically evident only during puberty. The pathogenesis has been linked to the deficiency of transforming growth factor - beta (TGF-beta) in the lesions, and growth during puberty is associated with the expression of progesterone receptors over the lesions.3 Dermoscopy of peripheral AVM occurring over the skin is not well-defined. One case report of acquired digital AVM showed dermoscopic features of blue-red lacunae, milky red areas, and winding red vessels of various thicknesses.4 Clinically, AVM is classified based on increasing intensity of severity by the Schobinger classification, as shown in Table 1.
| Stage number | Clinical presentation |
|---|---|
| I | Cutaneous blush and warmth |
| II | Bruits and thrills |
| III | Pain, ischemic necrosis, ulceration |
| IV | High-output cardiac failure |
The management of peripheral AVM can be done by endovascular approaches, surgery, sclerotherapy, or a combination of the above. Our case is, to our knowledge, the first case presenting the clinical and dermoscopic appearance of lymphangioma circumscriptum but is AVMs on histopathological and radiological evaluation. Both lymphangioma circumscriptum and AVM increase in size during puberty and present as an enlarging lesion around adolescence, causing potential confusion in diagnosis. Surgical excision of AVM without proper radiological investigation could have potentially adverse outcomes due to heavy bleeding from the malformation. Therefore, adequate imaging should be done before subjecting the patient to surgery.
CONCLUSION
This case underscores the potential for arteriovenous malformations to present clinically and dermoscopically indistinguishably from lymphangioma circumscriptum. Therefore, comprehensive imaging should be done in suspected cases before proceeding with surgical interventions, as the surgical strategies may differ significantly between the two conditions.
Authors’ contributions
Report concept and draft: Dr Siddharth Bhatt. Reporting of radiology images: Dr Shweta Pandey. Proof reading: Dr Biju Vasudevan. Reporting of pathology slides: Dr Gourang Paliwal. Data Collection: Dr Silky Priya. Intervention (Glue embolization): Dr K. Uday Bhanu.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Dermoscopy of cutaneous lymphangioma circumscriptum. Dermatol Pract Concept. 2017;7:37-8.
- [CrossRef] [Google Scholar]
- Lymphangioma In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470333 [Last accessed on 2021 Aug 12]
- [Google Scholar]
- Progesterone receptors identified in vascular malformations of the head and neck. Otolaryngol Head Neck Surg. 2009;141:491-5.
- [CrossRef] [Google Scholar]
- Acquired digital arteriovenous malformation: Clinical, dermoscopy, ultrasound and histological study. Eur J Dermatol. 2012;22:138-9.
- [CrossRef] [Google Scholar]







