Translate this page into:
Autologous Platelet-rich Plasma Enriched Pixel Grafting
Address for correspondence: Dr. Ravi Kumar Chittoria, Department of Plastic Surgery and Telemedicine Division, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Dhanvantari Nagar 605006, Puducherry, India. E-mail: drchittoria@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Autologous platelet-rich plasma contains concentrated platelets after graded centrifugation, which has various applications. Skin grafting is an age-old procedure, which has been used for wound coverage. But the healing process is longer and may be difficult, depending on the wound site, skin defect size, and patient comorbidities, and is difficult to be carried out in patients who have limited donor sites, such as in burns or those who are not fit for long procedures. Hence, pixel grafting can be used in these areas. Platelet-rich plasma can be used to aid the graft take, and thereby decreasing patient morbidity and improve the surgeon’s efforts.
Keywords
Autologous platelet-rich plasma
pixel grafting
platelet
INTRODUCTION
Autologous platelet-rich plasma (APRP) as the name suggests is concentration of the patient’s own platelets in a small amount of plasma. It is enriched by growth factors and it acts as a fibrin sealant and has various properties. Its important application is in skin grafting where it aids as a fibrin sealant and also aids in the take of the graft by enriching it with growth factors and promoting angiogenesis.
Split skin graft is the gold standard for the treatment of a raw area. But in many of the patients, especially in burns, the donor site area is limited, or in some patients, they are not fit for a sheet graft, and thereby require intermediate measures to aid in early epithelialization. By mincing a small sheet of split-thickness graft, it will expand and each island will be acting as a nidus for epithelialization. In this article, we would like to share our experience with using APRP as an enrichment media for pixel grafting.
MATERIALS AND METHODS
This study was conducted in the department of plastic surgery, in a tertiary care center in Pondicherry, from January 2019 to July 2019. Total of seven patients were included in the study.
The details of the patients are as follows:
| S. no. | Wound site | Wound size | Associated comorbidity | Method of reconstruction | Time taken by the wound to heal |
|---|---|---|---|---|---|
| 1 | Heel of left foot | 10 cm × 6 cm with destruction of heel pad | Diabetes mellitus type II | Skin graft | 6 weeks |
| 2 | Lateral aspect of heel of left foot | 7 cm × 8 cm | Diabetes mellitus type II | Skin graft | 5 weeks |
| 3 | Ulcer in the dorsum of right foot | 15 cm × 6 cm | Diabetes mellitus type II/chronic liver disease/portal hypertension | Skin graft | 7 weeks |
| 4 | Ulcer in the heel of right foot | 5 cm × 6 cm | Diabetes mellitus type II/left cerebrovascular accident/ischemic heart disease | Healing by secondary intention | 5 weeks |
| 5 | Fournier’s gangrene | 7 cm × 4 cm | Diabetes mellitus/hyperthyroidism | Healing by secondary intention | 4 weeks |
| 6 | Infected thermal burns | 15%–20% total body surface area | Sepsis/anemia | Pixel graft + sheet grafting | 8 weeks |
| 7 | Scald burns | 30% | Seizure disorder/anemia | Pixel grafting + sheet grafting | 8 weeks |
Owing to various comorbidities as stated in the table, sheet split-thickness skin grafting could not be performed. Hence, decision was made to take a small split-thickness skin graft and mince it and use it to cover the wound.
To enrich the graft take, APRP was used, the minced graft was mixed with it and applied over the raw area [Figure 1].

- Skin graft minced and mixed with autologous platelet-rich plasma
A standard and validated technique of APRP as described by Franco et al.[1] and Li et al.[2] was used.
The steps of APRP preparation were as follows: 10 mL of the patient’s heparinized venous blood was taken and was centrifuged at 3000 rotation per minute for 10 min. The upper layer of the three layers was taken and recentrifuged at 4000rotation per minute for 10 min. After this step, the content was separated into two layers [Figure 2]. The bottom layer of the plasma was rich in platelets and was aspirated using 18-gauge needle and was used to mix with the wound and to inject into the wound bed. Other adjunctive methods such as low-level laser therapy was also used to aid in graft take.
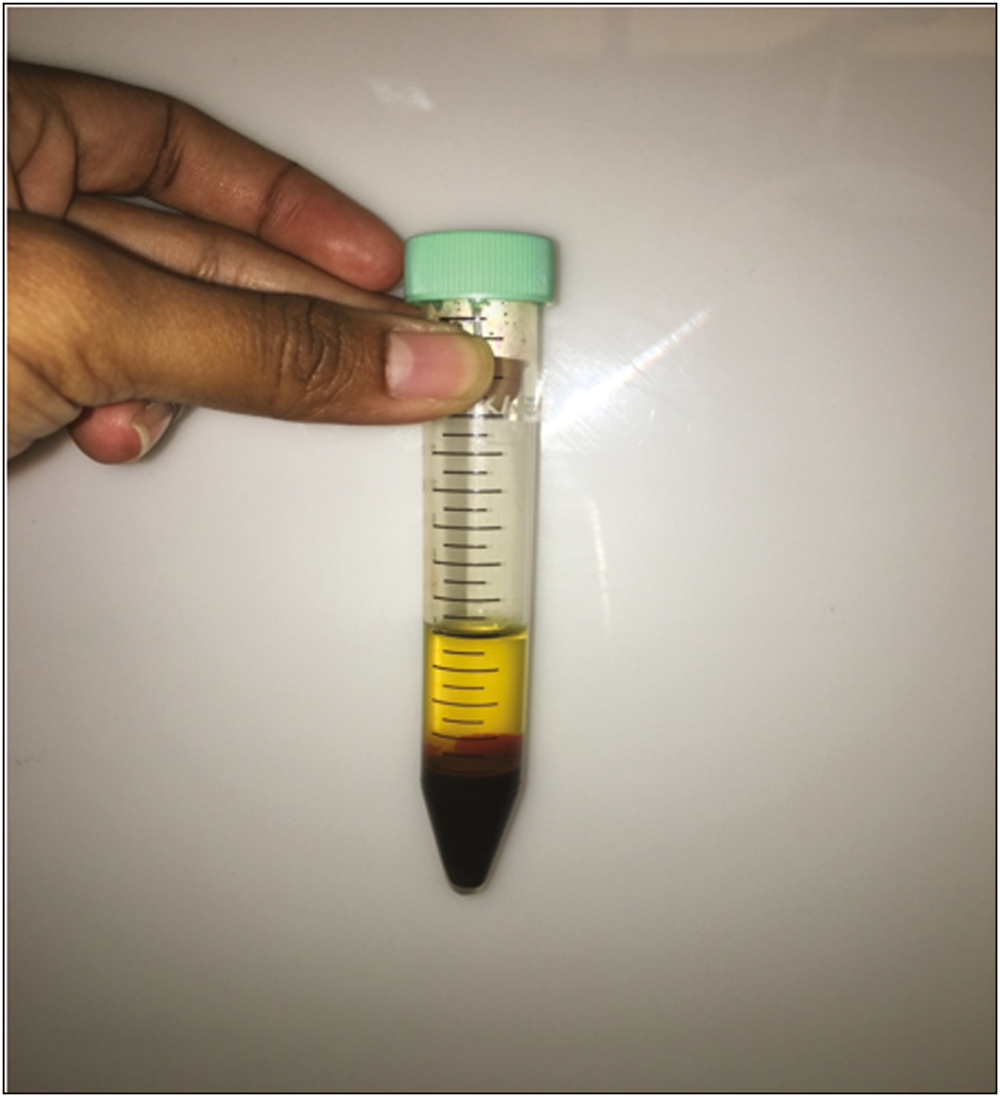
- Autologous platelet-rich plasma being prepared
The applied pixel graft was covered with a thin collagen sheet, and regular dressing was done [Figures 3 and 4].
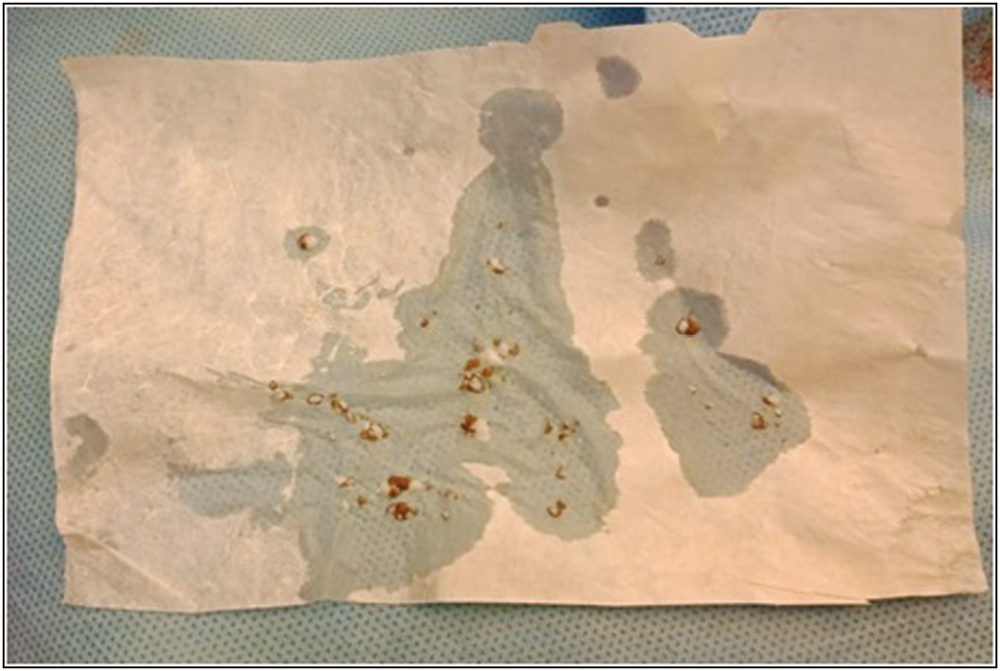
- Autologous platelet-rich plasma mixed pixel graft in collagen sheet

- Pixel grafts applied on the wound
The first look of the wound was carried out on day 7 and even though the wound was not completely healed, small areas of epithelialization appeared on the wound [Figures 5 and 6].

- Preoperative image of the wound

- Wound after final reconstruction
DISCUSSION
APRP is a biological product defined as a portion of the plasma fraction of autologous blood with a platelet concentration above the baseline.[3] The contents of the APRP are not only platelets, but also growth factors such as platelet-derived growth factors, chemokines, clotting factors, and fibrin.
The concept and description of PRP started in the field of hematology.[4] It was used for patients with thrombocytopenia. In the coming days, PRP has been used in various other fields such as musculoskeletal field in sports injuries, cardiac surgery, pediatric surgery, gynecology, urology, plastic surgery, and ophthalmology.
Owing to its contents, the use of APRP has been researched in the field of regenerative medicine in conditions such as alopecia, chronic wounds, and scar management.
The mainstay management of wounds is skin grafting. The main part of the skin graft is the take of the graft, which is in three stages:
Stage of imbibitions
Stage of inosculation
Stage of revascularization.
PRP aids in bridging the stages of skin graft take.
PRP functions as a tissue sealant and drug delivery system, with the platelets initiating wound repair by releasing locally acting growth factors via α-granules degranulation.[5] The application of APRP to STSG application sites has been recently described and theorized to provide immediate skin graft anchorage as well as inosculation of the STSG with nutrient-rich blood media.[6] Studies conducted by Gibranet al.,[7] on burns patients, have proven that PRP is safe and effective for fixation of skin grafts due to its adhesive nature, and its outcomes are better than securing skin graft to wound margins or bed with sutures, staples, or glue, hence it not only decreases the surgery time but also avoids the removal of sutures/staplers in postoperative period.[7]
Previous study conducted by Puttirutvong[8] has evaluated the healing time of both meshed full-thickness skin grafts versus STSGs (i.e., 0.015-in thickness) in patients with diabetes. This study revealed a mean total healing time of 20.1 ± 7.3 days for the STSG group, with the primary factor affecting graft take being hematoma/seroma formation and infection. Vijayaraghavan et al.[9] showed that wounds treated with APRP therapy alone healed in 4–8 weeks. Wounds treated with APRP and split skin graft/flap cover healed in 3–6 weeks.
Though effective in one patient, it requires multicenter, randomized control trial to validate the study and also needs to be tried on wounds of various etiology.
CONCLUSION
Hence APRP can be used as an effective media for enrichment of pixel graft, in patients who are do not have adequate donor sites or not fit for surgery, but also mainly without side effects. It is a cost-effective procedure, helps in early skin grafting and reduced hospital stay.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Protocol for obtaining PRP for autologous use. Aesthetic Plast Surg. 2012;36:1254-9.
- [Google Scholar]
- Subcutaneous injections of platelet-rich plasma. Plast Reconstr Surg. 2012;129:858-6.
- [Google Scholar]
- Randomized placebo-controlled, double-blind, half-head study to assess the efficacy of platelet-rich plasma on the treatment of androgenetic alopecia. Dermatol Surg. 2016;42:491-7.
- [Google Scholar]
- Platelet-rich plasma: underlying biology and clinical correlates. Regen Med. 2013;8:645-58.
- [Google Scholar]
- Efficacy of autologous platelet rich plasma over conventional mechanical fixation methods in split thickness skin grafting. Int Surg J. 2018;6:108.
- [Google Scholar]
- Use of platelet-rich plasma with split-thickness skin grafts in the high-risk patient. Foot Ankle Spec. 2008;1:155-9.
- [Google Scholar]
- Comparison of fibrin sealant and staples for attaching split-thickness autologous sheet grafts in patients with deep partial- or full-thickness burn wounds: a phase 1/2 clinical study. J Burn Care Res. 2007;28:401-8.
- [Google Scholar]
- Meshed skin graft versus split thickness skin graft in diabetic ulcer coverage. J Med Assoc Thai. 2004;87:66-72.
- [Google Scholar]
- Role of autologous platelet rich plasma (APRP) in wound healing. J Soc Wound Care Res. 2014;7:23-8.
- [Google Scholar]






