Translate this page into:
Baker's Dozen on the Scalp: An Interesting Case of Multiple Trichilemmal Cyst
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
The common swellings of the scalp are the epidermoid cysts (ECs), trichilemmal cysts (TCs), lipomas, dermoid cyst, pilomatrixoma, steatocystoma multiplex, cylindroma of which TC can be multiple.
A 55-year-old female presented with multiple, slow growing, painless swellings on the scalp. The first swelling appeared 15 years ago followed by others at varying intervals. There was no similar family history.
Scalp examination showed 13 varying sized swellings with the largest 3.5 × 3 cm and the smallest 1 × 1 cm [Figure 1]. All were well defined, smooth, non-tender and cystic in consistency. Routine haematological investigations and skull X-rays were normal. Fine needle aspiration cytology (FNAC) of the largest swelling showed keratinous material with probable diagnosis of EC. All the 13 cysts were excised at single sitting using multiple small incisions, which were closed primarily with 3-0 nylon interrupted sutures using perilesional infiltration of a mixture of 2% lignocaine with adrenaline and 0.5% bupivacaine diluted with equal parts of sterile water for local anaesthesia (LA) [Figure 2]. Histopathology revealed features of TC without proliferation [Figure 3].

- Clinical photograph of the patient showing multiple trichilemmal cysts on the scalp
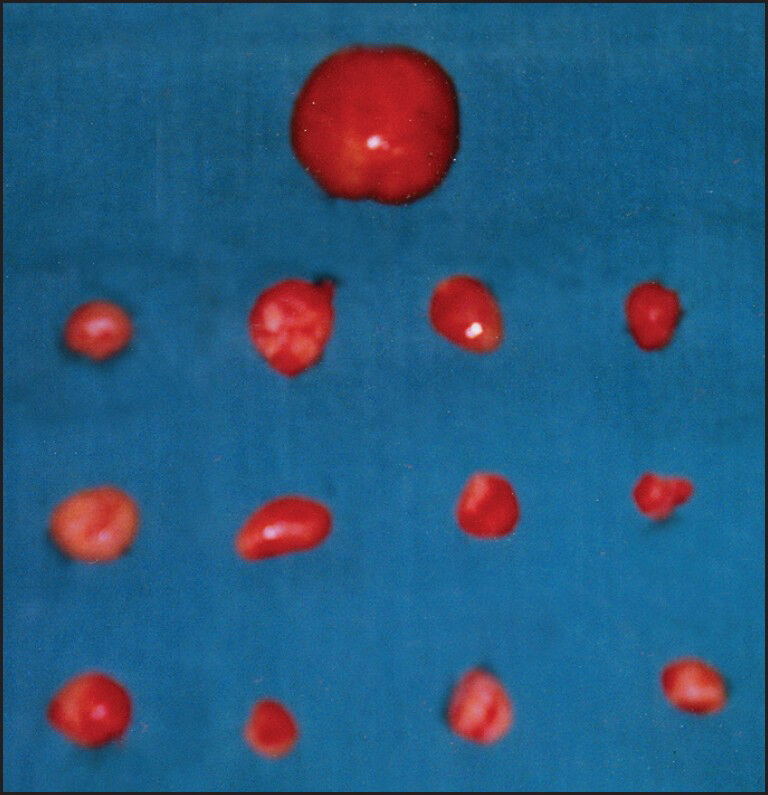
- Excised specimens showing thirteen trichilemmal cysts of varying sizes
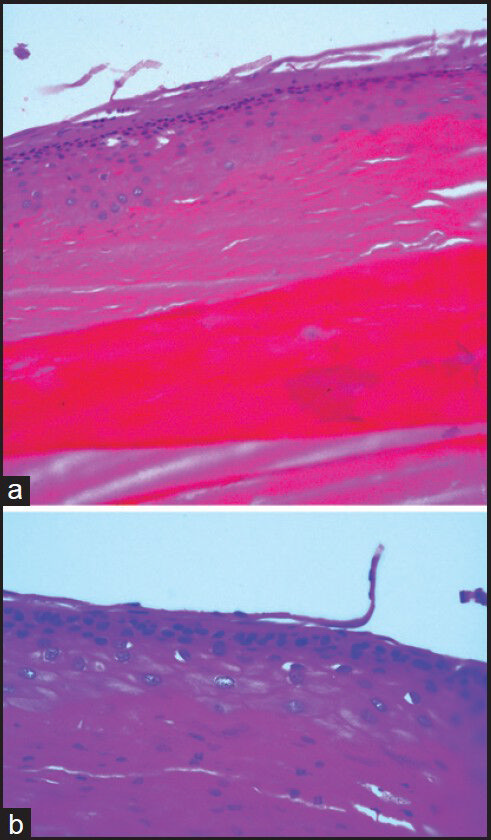
- (a) 20× (H&E): The section show the stratified squamous epithelium lining. The lumen is filled with acellular eosinophilic keratinous material (b) 40× (H&E): The higher magnification show the lack of granular layer
TCs are benign cystic swelling, which arise from the epithelium of follicular isthmus, where the inner root sheath is shed off and the outer root sheath (trichilemma) of the hair follicle undergoes a specific form of keratinisation forming a cyst wall without a granular layer.[1] They affect 5-10% of the population with a female preponderance.[1] A family history may be present because the condition can have an autosomal dominant (AD) pattern of inheritance.[2] Seidenari et al., proposed clinical criteria for recognising AD hereditary cases.[3]
About 70% of the patients have multiple cysts.[4] Ninety percent of the TC occur over the scalp[24] and rarely the face, trunk and extremities may be involved.[2] TC may be commonly confused with EC clinically.[4] Unlike EC, no punctum is seen.[2] As was in our case, patients with TC frequently present late as the swelling is painless, slow growing[2] and can be left hidden under the hair.
The hallmark pathological feature is in the cells of lining epithelium, which gradually increase in size as they approach the cyst cavity, appearing swollen with pale cytoplasm.[2] On histopathology, TC can be differentiated from EC by the absence of granular layer and presence of abrupt keratinisation in the cyst wall.[2] Lobules of squamous epithelium in the cyst wall suggest a proliferating trichilemmal cyst (PTC).[5] Other histologic characteristics of PTC may include mitoses, cell atypia and necrosis. Rapid growth and ulceration indicates malignant degeneration, which is quite rare.[2]
Treatment is excision biopsy,[1] which can be easily done under LA. It is the personal experience of the author that TCs are rather easy to excise than the other cysts on the scalp because of the easy plane of cleavage between the cyst wall and surrounding structures. Thomas et al.[1] have also reported that excision can be done with smaller incisions because of the more firm nature of the cyst facilitating easy enucleation.
This case highlights the multiplicity of the cyst, late presentation of the patient and surgical ease of excision.
REFERENCES
- Benign epithelial tumors, hamartomas and hyperplasias. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, eds. Fitzpatrick's Dermatology in General Medicine (7th ed). New York: McGraw-Hill Companies; 2008. p. :1054-67.
- [Google Scholar]
- Hereditary trichilemmal cysts: A proposal for the assessment of diagnostic clinical criteria. Clin Genet. 2013;84:65-9.
- [Google Scholar]
- Skin and subcutaneous tissue. In: Williams Norman S, Bulstrode Christopher JK, Ronan OP, eds. Bailey and Love's Short Practice of Surgery (25th ed). London: Hodder Arnold; 2008. p. :593-622.
- [Google Scholar]
- Benign epithelial tumors, hamartomas, and hyperplasias. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, eds. Fitzpatrick's Dermatology in General Medicine (8th ed). New York: McGraw-Hill; 2012. p. :1334.
- [Google Scholar]





