Translate this page into:
Bilobed Flaps: An Esthetic Method of Reconstructing Circular Defects
Address for correspondence: Dr. Tejashwani Lal, MD, Department of Dermatology and Venereology Civil Hospital, Jalandhar, Punjab, India. E-mail: tejashwa@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Local flap reconstruction is an important skill used to excise and repair many cutaneous defects in various anatomical regions of body. In this article, the authors have described the bilobed flap reconstruction technique useful in the resection of various circular and semicircular defects, especially over nose tip and lateral wall of the nose. The authors have highlighted various indications, procedural techniques, and complications related to the surgery which will help in better esthetic outcome.
Keywords
Basal cell carcinoma
bilobed flap
flap necrosis
pincushioning
undermining
INTRODUCTION
The bilobed flap is a local transposition flap primarily used in the head and neck region, particularly the nasal tip,[1] but can be employed in other areas of the body as well. With time it has gone under many modifications and has been used for other anatomical areas well. It was first described in 1918 by Esser for use in nasal tip reconstruction.[2] The original flap used a rotational arc of 180° and based the second lobe superiorly, toward the glabellar region. In 1953, Zimany showed that the second and third lobes could be smaller than the first lobe and that the flap could be utilized in more anatomical areas. In the 1980s, McGregor and Soutar introduced the concept that a reduced pivotal angle would result in smaller standing cutaneous deformities (dog ear deformity) and decreased pincushioning.[2] Zitelli went on to improve the design further limiting the total rotational arc to between 90° and 110°; this variant is the most common modification in use today. It has been used in the reconstructions of trunk,[3] hands,[4] cheek,[5] earlobe reconstruction,[6] and feet defects by many authors since then. Its principle is also advantageous in reconstructions of larger facial defects. Successful reconstruction of problematic suborbital area using the bilobed flap was reported by Yenidunya in 2007.[7] It can be a highly rewarding technique in the excision of basal cell carcinoma, melanoma, and moles over the head and neck region [Figures 1,2,3].
![Earlobe reconstruction with a superiorly based bilobed infra-auricular flap[6]](/content/173/2023/16/3/img/JCAS-16-245-g001.png)
- Earlobe reconstruction with a superiorly based bilobed infra-auricular flap[6]
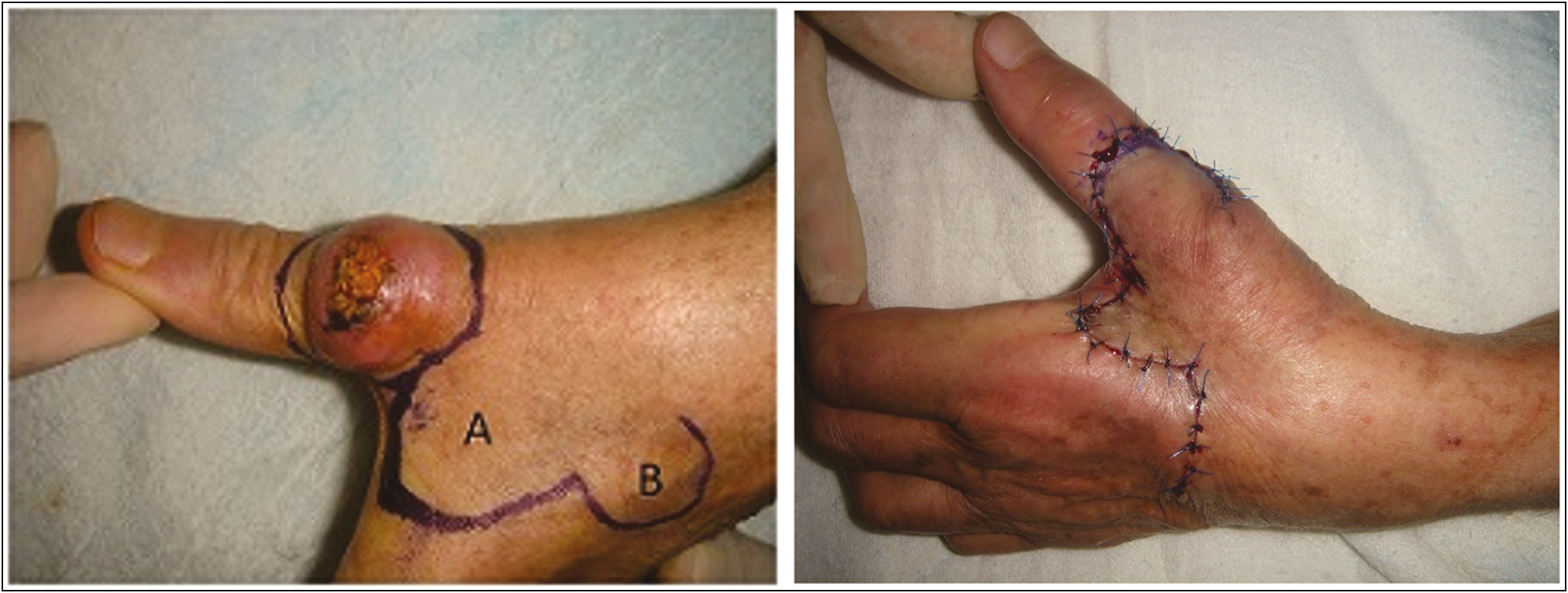
- Bilobed flap for reconstruction of a large keratoacanthoma of the thumb
![The usefulness of the bilobed flap for lateral cheek defects[5]](/content/173/2023/16/3/img/JCAS-16-245-g003.png)
- The usefulness of the bilobed flap for lateral cheek defects[5]
TECHNIQUE
The bilobed flap is a double transposition rotational flap wherein the first lobe serves to fill the first defect, and a second lobe fills the defect created due to the first lobe (the “secondary defect”). This approach helps in distributing the tension across a wider area of tissue, but at the cost of additional incision length.[2]
Firstly, the lesion due to be removed should be marked with an appropriate margin circumferentially with the help of a skin marking pen, nasal tip defects of 10–15 mm in diameter are ideally suited to bilobed flap reconstruction.
Then a pivot point (P) is marked in the direction of maximum skin elasticity where u want you skin flaps to lie. The pivot point is marked from the defect at a distance equal to the radius of defect. This pivot point serves as a landmark according to which remaining flaps are drawn.
At this pivot point (P), now an imaginary line is drawn at a maximum angle of 90° or 100° in which the flaps will lie [Figure 4].
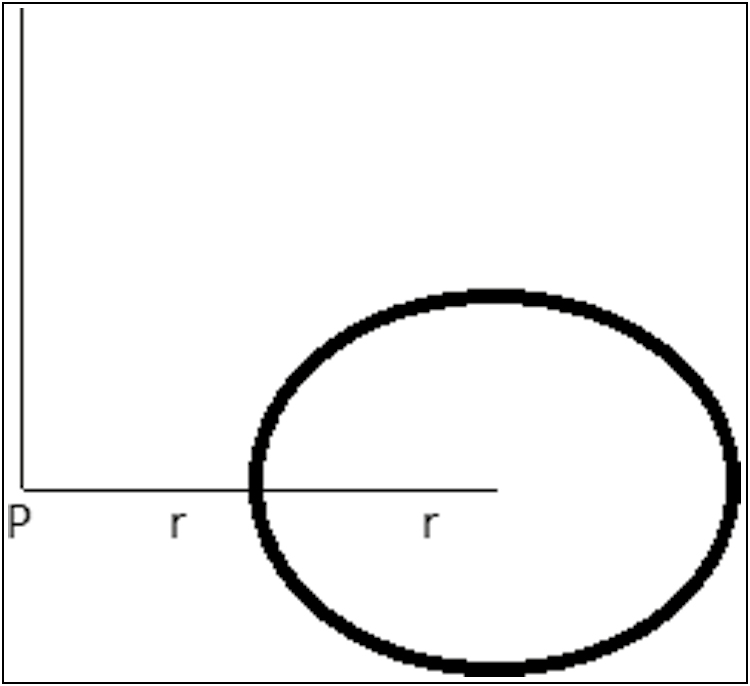
- The pivot point (P)
Now from the pivot point two concentric circles are drawn at a distance of 2r and 3r [Figure 5].
- Showing concentric arcs in which the flaps will lie
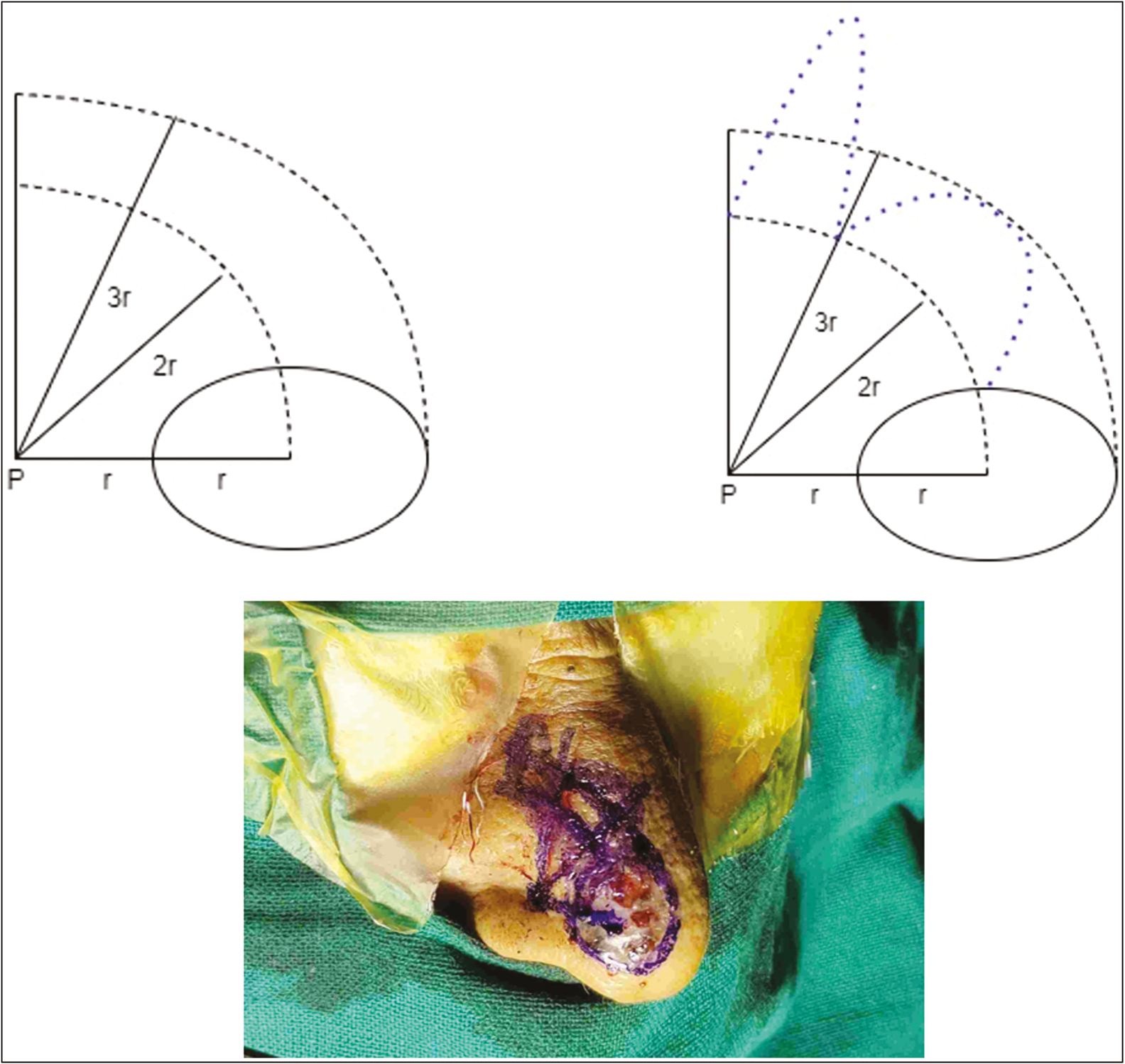
The first lobe of the flap (a) is marked directly superior to the defect, with a diameter 80–100% of that of the defect. For nasal tip defects, the diameter of the first lobe usually needs to be quite close to the diameter of excised defect because the skin of the lower nasal dorsum and supratip is not particularly elastic.
The second lobe of the flap (b) is then drawn immediately adjacent to the first lobe, in the half past one O’clock position, 45° off the vertical axis. This second lobe should then have a “conical hat” added to it that will facilitate closure without a standing cutaneous deformity/dog ear formation [Figure 6]. Dog ear/standing cutaneous deformity is a characteristic bunching up of excess tissue formed during wound closure.[8]
![Showing improved design with minimum chance of dog ear formation[9]](/content/173/2023/16/3/img/JCAS-16-245-g006.png)
- Showing improved design with minimum chance of dog ear formation[9]
At this point, some surgeons will then excise a Burow’s triangle extending laterally from the defect along the base of the flap, but others prefer to wait until they are certain exactly how much excess tissue needs to be excised to overcome any dog ear/standing cutaneous deformity.[2]
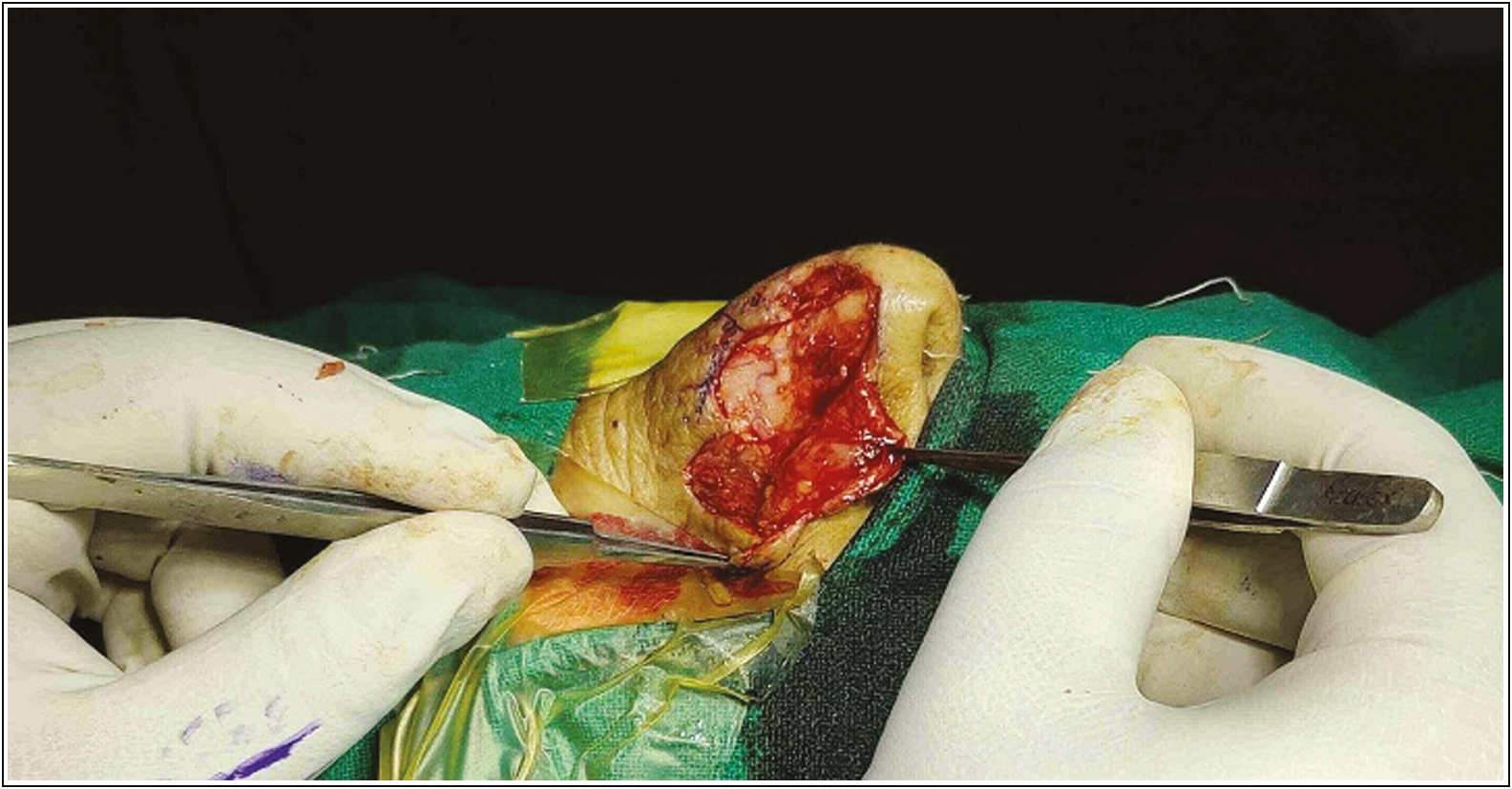
Once the lesion has been excised, the wound bed should be removed down to the level of the perichondrium [Figure 7], not only for oncological integrity, but for ease of dissection and maximization of flap perfusion.

- Showing excision of the defect up to the level of perichondrium
After the incisions are done, wide undermining must be performed in a subdermal plane, or if on the nose, a submuscular plane. Undermining is one of the most critical point in almost all local flap reconstructions, as it is not only the flap that moves to the wound, but the wound that moves to the flap as well. After achieving hemostasis with coagulation or cauterization, closure begins.
The tertiary defect, with the conical hat should be sutured first, with buried, interrupted, deep dermal stitches. On the nasal dorsum, a 5-0 vicryl suture works well. Then the secondary defect is to be closed with similar buried, interrupted sutures which usually requires excision of some or all of the “hat.”
Finally, the primary or the main defect is closed and the Burow’s triangle excised, if it had not been excised earlier, as mentioned above.
Lastly, a superficial suture layer should be placed; on the nose, a 6-0 monofilament polyamide black is suitable, which can be removed after 1 week [Figure 8].
- Primary skin closure done with 6-0 monofilament polyamide black sutures
Adhesive tape strips or nasal cast may be applied as well, similar to a rhinoplasty dressing which will help reduce edema and protect the surgical site.
COMPLICATIONS
The potential complications specific to this procedure are swelling, scarring, flap necrosis, infection, and bleeding. With the decrease in the arc of rotation the tension can be minimized at closure site, as is wide undermining. Dog ear formations/standing cutaneous deformities are also a risk, and again can be reduced with a smaller rotation arc. Smaller angles of flap transposition produce less severe “dog ear” deformities along the border of the flap and allow the surgeon to transfer the flap more easily producing lesser wound tension causing less alar displacement.[10] In the original bilobed flap, as described by Esser with a 180° rotation, standing cutaneous deformities (dog ear) were almost inevitable, but they are much less common when employing the Zitelli modification. If tension while closing is too great, the perfusion will suffer, particularly venous drainage, and flap loss can happen. Infection can also appear in any area of the wound and is more liable to appear in areas of necrosis. Postoperative bleeding resulting in the hematoma formation can occur under the flap, which may compromise blood flow and potentially result in loss of the flap.
Excessive tension can occur upon closure of the primary lobe or primary defect[11] specially in Asians; hence many modifications of the current techniques have been developed to overcome the specific difficulties in different ethnicities. The modification of Zitelli’s bilobed flap to have a longer primary lobe and making slight downward displacement of the ipsilateral alar margin intraoperatively, can prevent nasal alar retraction in the reconstruction of distal nasal defects in Asians.[11]
Due to the crescentic shape of the flap, it is at risk of developing a pincushion deformity or trapdoor deformity as a result of subdermal tissue contraction [Figure 9]. The trapdoor effect is an elevated and bulging deformity of tissue within the semicircular confines of a U-, C-, or V-shaped scar. Various theories to explain this phenomenon are lymphatic and venous obstruction, hypertrophy of the scar, excessive fatty and redundant tissue, beveled wound edges, and contracture of the scar.[13] When the tension at flap inset is minimized, less pincushioning effect is seen. The excess skin for this flap is ultimately recruited from the lax skin of the upper side-wall of the nose. Wide undermining is important not only to reduce tension and simplify tissue movement but also to reduce pincushioning. While the true pathogenesis of pincushioning flaps is unknown, the contraction phase of wound healing limited to the underside of a transposition flap contributes to pincushioning. To prevent this complication, the skin surrounding a transposition flap must be undermined and the plate like scar that is continuous beneath the flap and adjacent skin will contract uniformly, stabilizing the entire surgical site[9] and preventing pincushioning of the flap alone [Figure 10]. Tissue undermining may prevent the development of the trapdoor effect in transposition flaps.[14] However, the deformities such as pincushion effect and trapdoor can be corrected with the help of dermabrasion, pinhole laser ablation, or shave excision or z plasty.
![Pincushion deformity creates a scar on the supratip region of nose[12]](/content/173/2023/16/3/img/JCAS-16-245-g009.png)
- Pincushion deformity creates a scar on the supratip region of nose[12]
- Wide undermining of the surrounding area making a plate like scar
Undermining should continue beyond the base of the bilobed flap. Undermining is usually done at the level just above the perichondrium or periosteum. For flaps based laterally, the pedicle should be undermined deeply in or beneath the muscle of the nasal side wall so that the flap has an adequate blood supply. Undermining above the muscle compromises the blood supply and increases the risk of distal flap necrosis.[9] As the flap is against the relaxed skin tension lines, there are more chances of the dehiscence of the suture line; hence wide undermining and buried dermal sutures should be done at the places of maximum tension to reduce the tension which is also accentuated due to rotation of flap and the areas such as nasal bridge where skin is relatively thin the dermal sutures can be skipped and closure in a single layer can be done.
CONCLUSION
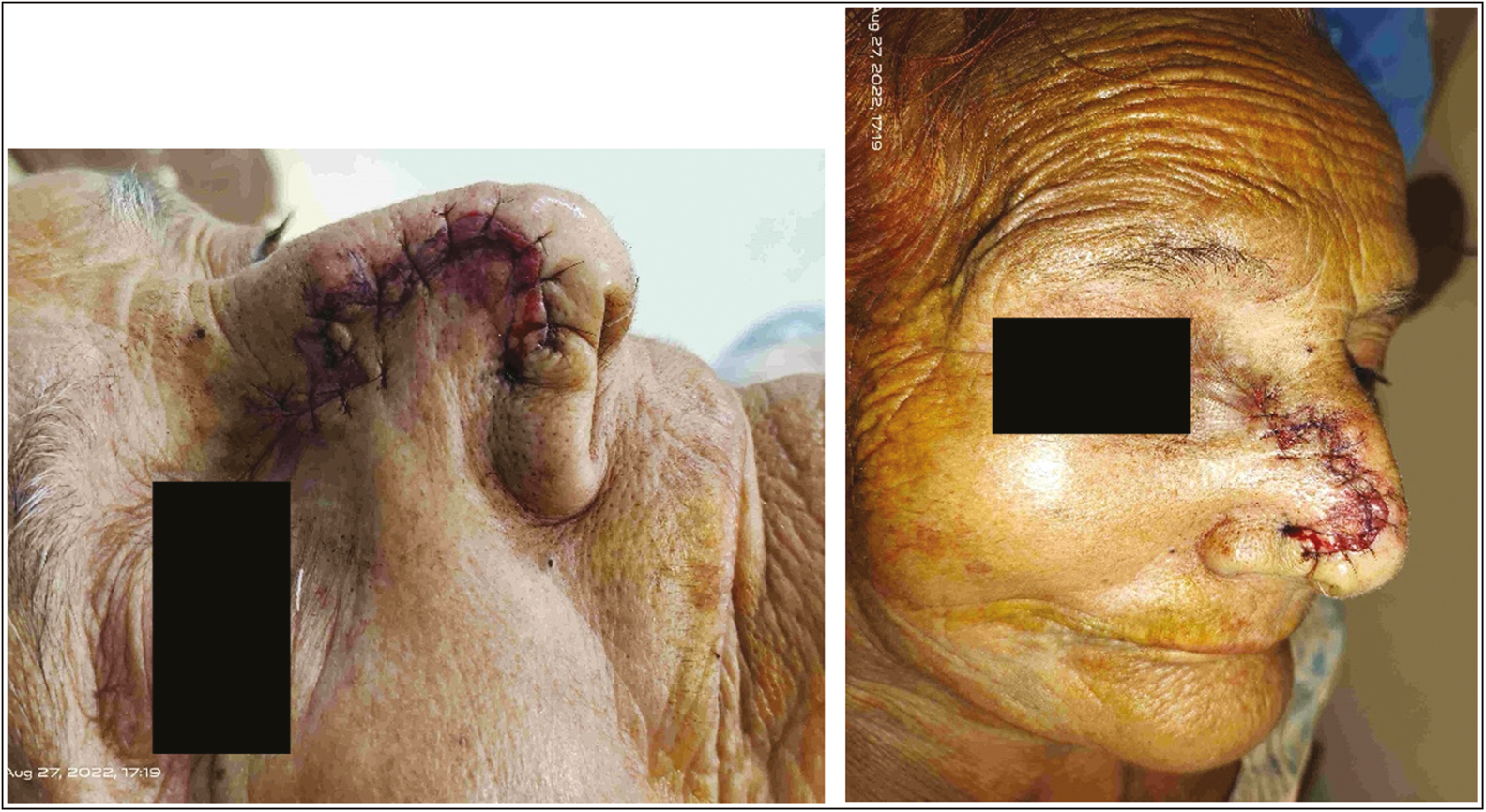
Bilobed flap plasty is a versatile method of reconstruction which can be used not only over face but various other anatomical sites and should be considered in the reconstruction of defects of the face, because unlike other techniques, it preserves good texture and color of facial skin with minimal donor site morbidity [Figure 11].

- Pre and post op 7 days and after 1-month results
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Basal cell carcinoma of the outer nose: overview on surgical techniques and analysis of 312 patients. J Cutan Aesthet Surg. 2014;7:143-50.
- [Google Scholar]
- Bilobed flaps. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2022.
- [Google Scholar]
- Reconstruction of trunk defects with bilobed myocutaneous flap. Br J Plast Surg. 2005;58:652-7.
- [Google Scholar]
- Bilobed flap for reconstruction of a large keratoacanthoma of the thumb. Case Reports Plast Surg Hand Surg. 2019;6:86-7.
- [Google Scholar]
- The usefulness of the bilobed flap for lateral cheek defects. Can J Plast Surg. 2012;20:e19-21.
- [Google Scholar]
- Earlobe reconstruction with a superiorly based bilobed infra-auricular flap. J Cutan Aesthet Surg. 2019;12:201-2.
- [Google Scholar]
- Bilobed flap reconstruction in infraorbital skin defects. Plast Reconstr Surg. 2007;119:145-150.
- [Google Scholar]
- Bilobed flaps for cutaneous nasal defects: a case series. Int Surg J. 2022;9:1742-4.
- [Google Scholar]
- The bilobed flap for reconstruction of distal nasal defect in Asians. Aesthetic Plast Surg. 2009;33:600-4.
- [Google Scholar]
- Available from: https://www.drlamperti.com/blog/news-and-updates/uncategorized/pin-cushion-deformity-and-bulbous-nose-repair [Last accessed on 6 September 2022]
- Trapdoor effect in nasolabial flaps. Causes and corrections. Arch Otolaryngol. 1985;111:421-4.
- [Google Scholar]
- Role of tissue undermining in the trapdoor effect of transposition flaps. J Dermatol Surg Oncol. 1993;19:128-32.
- [Google Scholar]






