Translate this page into:
Can Radiofrequency Ablation Be Utilized With Equal Effect in Place of Carbon Dioxide Laser in the Treatment of Facial Angiofibromas in Patients of Tuberous Sclerosis?
Address for correspondence: Dr. Gomathy Sethuraman, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi 110029, India. E-mail: aiimsgsr@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Facial angiofibromas in patients of tuberous sclerosis cause significant cosmetic concern in them. Available medical and surgical modalities for the treatment of angiofibromas are limited.[12] Carbon dioxide (CO2) laser has been the most widely used modality and was found to be effective in small case series.[3] But, it is expensive and beyond the reach of a majority of patients due to unavailability in most dermatology facilities. Radiofrequency ablation (RFA) is a commonly used office procedure in most dermatology clinics. It can be an alternative modality in the management of angiofibroma as it is effective in other benign appendageal tumors of the face.[456] No randomized studies compared the efficacy and safety of CO2 laser vs. RFA in facial angiofibromas.
This split-face randomized study was conducted in tuberous sclerosis patients >10 years of age with angiofibromas over the face. Patients with uncontrolled seizures, photosensitive disorders, cardiac pacemakers, and metallic implants were excluded. Their cheeks were randomized by a computer-generated sequence to receive either CO2 laser or RFA. CO2 laser (CIS-F1, Sellas, Korea) was done in THE ablative mode using the following parameters: energy 18–24 mJ/cm2, frequency 800 Hz, pulse duration 1.25 ms. RFA was done (SHALYA LX, monopolar and bipolar cut with pure sine wave 390 kHz RFA) with power ranging from 12 to 20 in the cutting mode. Both the procedures were done under topical anesthesia with a eutectic mixture of lignocaine and prilocaine. If required, additional infiltration anesthesia was given with 2% lignocaine with adrenaline. All the patients received at least two sittings of the procedure. In case of lack of response, further sittings were done on both sides at 4 weeks’ interval according to the protocol. Serial digital photographs were taken, and the improvement was assessed by two independent dermatologists blinded to the trial protocol. The percentage improvement was graded on a quaternary scale.
Eleven patients of angiofibroma with no history of seizures or seizures controlled on medication were included over 12 months. There were six males and five females. The mean age of the patients was 19.6 ± 5.01 years. Five patients received two sessions, five patients required three sessions, and one patient received four sessions of both laser and RFA. The number of sittings was equal on both sides. Patients were assessed at each visit, and the final assessment was done 2 months after the last sitting. In the laser-treated side, the mean percentage improvement ranged from 35% to 80% (52.7 ± 17.8), whereas in the RFA-treated side the improvement was from 10% to 80% (49.3 ± 23.3) [Figures 1 (B) and (D) and2(B) and (D)]. Improvement in both the arms was comparable (P = 0.35).
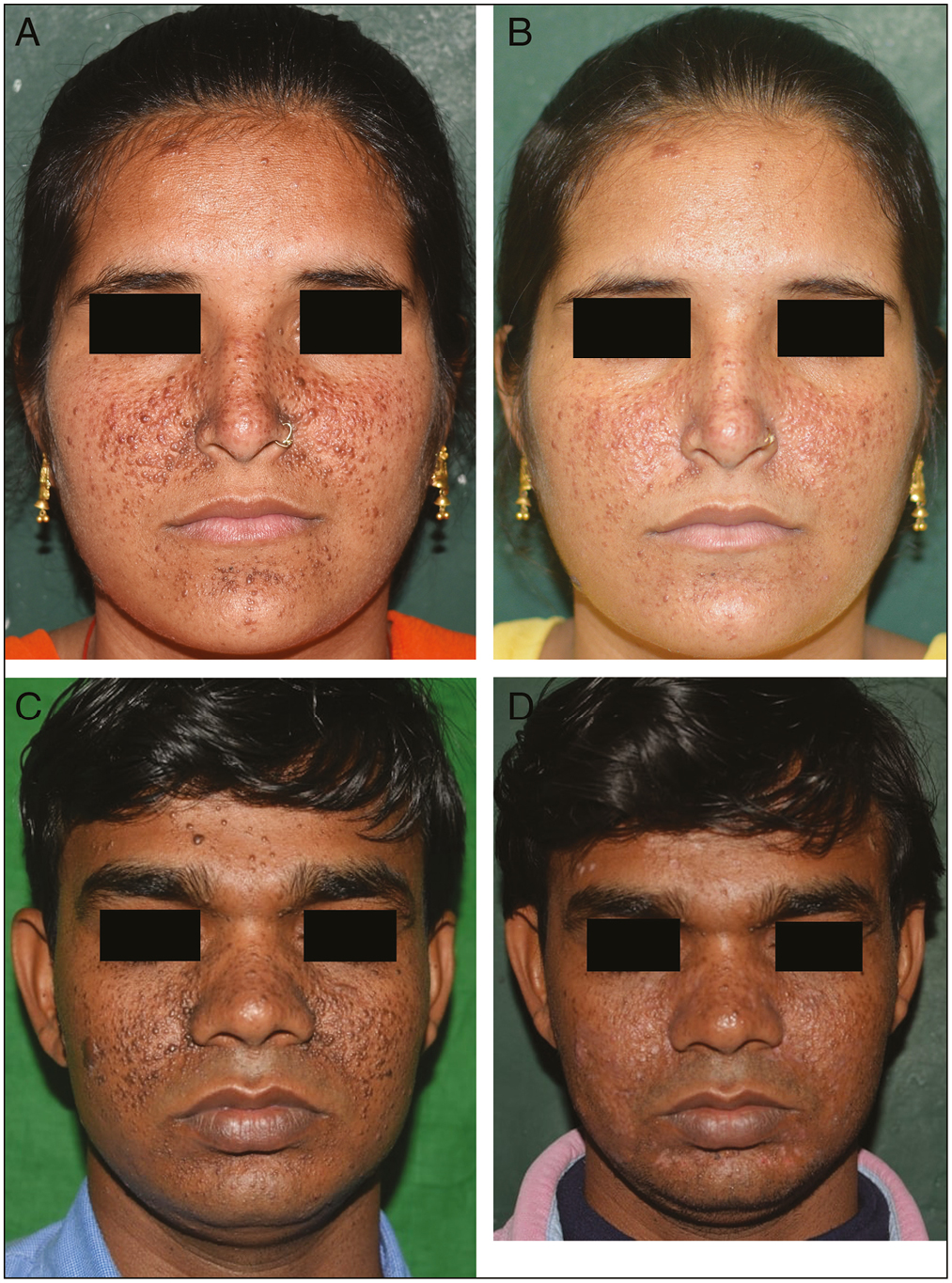
- Improvement in facial angiofibromas: (A) and (C) at baseline; (B) and (D) after carbon dioxide laser (right cheek) and radiofrequency ablation (left cheek) after three sessions

- Improvement in facial angiofibromas; (A) and (C) at baseline; (B) and (D) after carbon dioxide laser (left cheek) and radiofrequency ablation (right cheek) after two sessions
Similarly, there was no difference in improvement according to the patient global assessment (mean 57.3 ± 23.3 vs. 53.7 ± 28.4, P = 0.37). Nine patients in the laser group and 10 patients in the RFA group required infiltration anesthesia. Pain during the procedure was graded according to a visual analog scale ranging from 1 to 10. It varied from 2 to 6 in both the groups with a mean of 3.4 ± 1.1 and 3.5 ± 1.2 in the laser and RFA groups, respectively. There was no significant difference between the two sides (P = 0.88).
All patients had transient hypo- or hyperpigmentation after the procedure. On the RF-treated side, one patient had post-inflammatory hyperpigmentation, and another patient had a shallow depressed scar at the final assessment. No patient on the laser-treated side had persistent pigmentary changes or scarring.
Our trial demonstrates no statistically significant differences in the overall outcome between CO2 laser and RFA in the treatment of angiofibroma. Owing to the similar outcomes and ease in the administration of RFA, it can be considered in the initial management of facial angiofibromas. Although not backed by results of cost–benefit analysis, considering the similar number of sessions for both the procedures, RFA can be employed in a resource-poor setting as a safe and economic procedure. The limitations of the study were small sample size and a lack of a validated grading system to assess the severity of involvement for comparison. Even with limited sample size, our research has provided some preliminary guidance in the management of angiofibromas. However, further large-scale randomized trials are recommended.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
None.
References
- Treatment of angiofibromas with a scanning carbon dioxide laser: A clinicopathologic study with long-term follow-up. J Am Acad Dermatol. 2001;45:731-5.
- [Google Scholar]
- Our experience of carbon dioxide laser ablation of angiofibromas: Case series and literature review. J Cosmet Laser Ther. 2016;18:372-5.
- [Google Scholar]
- CO2/erbium:YAG/dye laser combination: An effective and successful treatment for angiofibromas in tuberous sclerosis. Aesthetic Plast Surg. 2014;38:192-8.
- [Google Scholar]
- Periorbital syringoma treated with radiofrequency and carbon dioxide (CO2) laser in 5 patients. J Drugs Dermatol. 2012;11:879-80.
- [Google Scholar]
- Radiofrequency ablation: A safe and economical modality in treatment of Brooke–Spiegler syndrome. Dermatol Online J. 2012;18:7.
- [Google Scholar]





