Translate this page into:
Carbon Dioxide Laser Plus Topical 5% Luliconazole: A Better Combination Therapeutic Modality for Onychomycosis
Address for correspondence: Dr. Shahnawaz Bashir, Department of Dermatology, Government Medical College, 9-Hill View Colony, Old Airport Road, Wanabal Rawalpora, Srinagar 190005, Jammu and Kashmir, India. E-mail: drmsb2000@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Onychomycosis has always been a therapeutic challenge because of longer treatment duration, potential adverse effects of oral antifungals, and limited efficacy of topical agents. During the past few years, the emergence of laser therapy has been the topic of discussion as a newer, safe, minimally invasive modality of treatment.
Aim:
The aim of this study was to evaluate the role of fractional CO2 laser and topical luliconazole 5% lotion in the treatment of onychomycosis, as a combined treatment and as independent modalities.
Materials and Methods:
This was a prospective, randomized, triple-limb comparative observational study in which 106 patients with KOH and culture-proven onychomycosis were randomly assigned to three groups. Group A received fractional CO2 laser (10,600nm) triweekly for four sessions (0, 3, 9, and 12 weeks) plus topical luliconazole 5.0% lotion applied twice daily on the affected nail plates and nail folds for 12 weeks. Group B received only fractional CO2 with the same frequency of sessions and laser parameters as in group A. Group C received only topical luliconazole 5.0% solution twice daily for 12 weeks. Treatment outcome was evaluated using onychomycosis severity index (OSI) score, mycological parameters, and level of satisfaction of patients.
Results:
The degree of clinical improvement, mycological cure, and patient’s satisfaction was significantly better in the combined group than individual modalities. There were no severe adverse effects that warranted the discontinuation of the treatment in any of these patients.
Conclusion:
Fractional CO2 laser combined with topical luliconazole 5% lotion is a safe and effective treatment for onychomycosis especially in those who have contraindications to oral antifungals.
Keywords
Fractional CO2 laser
luliconazole
onychomycosis
OSI
INTRODUCTION
Onychomycosis (OM) describes a fungal infection of the nail caused by dermatophytes, nondermatophyte molds (NDMs), or yeasts. With a prevalence of 0.5%–5% in India[1] and up to 11% across Europe,[2] it accounts for 50% of all causes of nail dystrophy.[3] OM adversely impacts quality of life due to its effects on dexterity, appearance, and social and interpersonal relationships.
A number of treatment modalities are available for OM which includes antifungals, nail avulsion and debridement, iontophoresis, and ultrasound. Oral antifungal drugs have been the mainstay of therapy for many years offering a cure rate of 40%–80%,[4] but potential serious side effects and longer course of treatment restrict their use. Topical antifungals could be a relatively safer alternative bypasses the systemic adverse reactions, but their inability to penetrate through the nail plate renders them relatively less effective.[5] Laser-assisted drug delivery is an evolving modality that may allow for a greater depth of penetration by topical medications thereby improving their efficacy.[6] In addition, lasers may primarily result in fungal eradication owing to thermal effect of laser pulses that cause disruption of fungi and spores.[7]
Considering the poor response to various treatment modalities, new and broaden spectrum of treatment options with reduced side effects are required. This study was conducted with an aim to ascertain efficacy of fractional CO2 laser and luliconazole 5% lotion as sole treatment modalities and in combination for the management of OM.
METHODS AND MATERIALS
Study design
This was a prospective, randomized, triple-arm comparative observational study, which was conducted in our tertiary care center between February 1, 2019 and December 31, 2020. Patients were randomly allocated to three groups.
Group A: Received fractional CO2 laser (10,600nm) triweekly for four sessions (0, 3, 9, and 12 weeks) plus topical luliconazole 5.0% lotion applied twice daily on the affected nail plates and nail folds for 12 weeks. A topical esthetic cream (2.5% lidocaine and 2.5% prilocaine) was applied 20–30 min before the laser session. The fractional CO2 laser was used in a static mode to deliver pulse energy of 110 mJ, a density of 256 spots/cm2, pulse duration of 500 µs, and a circular spot size of 3–5 mm. The affected area including 1–2 mm margin was subjected to 2–3 passes of the laser beam. Wherever deemed necessary, adjacent nail-folds were also irradiated.
Group B: Received only fractional CO2 laser (10,600nm) triweekly for four sessions (0, 3, 9, and 12 weeks) with the same laser parameters as in group A.
Group C: Received only topical luliconazole 5.0% solution twice daily for 12 weeks.
Study population
A total of 102 patients with OM were recruited in the study. Diagnosis was made clinically, and confirmed by direct KOH microscopy of nail scrapings in addition to culture on modified Sabouraud dextrose agar medium.
Exclusion criteria of the study included patients who had received systemic or topical antifungal therapy within preceding 12 weeks and those with other nail disorders that cause nail plate dystrophy/discoloration (such as lichen planus, psoriasis, eczema, and traumatic dystrophy). In addition, pregnant females, nursing mothers, diabetics, patients with immunocompromising diseases or therapies were also excluded.
The study protocol was approved by the institutional ethical committee; and all the recruited patients willingly signed a written informed consent to be a part of the study.
Specially designed proformas were used to record parameters like sex of patients, age, duration of the disease, clinical type of OM, nails involved (fingernails or toenails), and degree of severity of OM.
Physical evaluation
Severity of OM was graded by measuring the onychomycosis severity index (OSI),[8] which was calculated at baseline, at 15 weeks (i.e., 3 weeks after treatment completion) and at 24 weeks (follow-up visit 12 weeks after treatment completion). Depending upon the percentage change in OSI score with respect to baseline, the degree of clinical improvement on 15th week and 24th week were evaluated as follows: 0%–25% change in OSI score = no improvement, 26%–50% = mild improvement, 51%–75% = moderate improvement, and 76%–100% = marked improvement.
Mycological evaluation
It was assessed by performing KOH microscopy of nail scrapings and culture of Sabouraud medium (with cycloheximide) 3 weeks after completion of treatment.
Evaluation of patient’s satisfaction
At the end of the study (3 weeks after the treatment completion), the patients’ satisfaction was assessed as unsatisfied, mildly satisfied, moderately satisfied, and very satisfied.
Evaluation of adverse effects
The patients were advised to report any adverse effect in the form of severe pain, itching, burning sensation, erythema, contact dermatitis, or nail fold swelling.
Statistical analysis
Data were entered in Microsoft Excel and analyzed using Statistical Package for the Social Sciences (SPSS) software program, version 25.0. Data were statistically described in terms of mean ± standard deviation (±SD), frequencies (number of cases), and relative frequencies (percentages) when appropriate. Analysis of variance (ANOVA), chi-square test, and Kruskal–Wallis test were used to find statistical associations between various variables. A value of P < 0.05 was considered statistically significant.
RESULTS
Of 102 patients recruited, 4 patients were lost to follow-up from each group leaving only 90 subjects for analysis. The mean age of the participants was 37.54 ± 14.32 years in group A, 34.42 ± 12.14 years in group B, and 35.22 ± 13.34 in group C with insignificant differences among the groups. Also, there was no statistically significant difference between the three studied groups as regards the gender, duration of disease, type number of nails involved (finger/toe), clinical type of OM, and the fungal pathogen identified on culture. In all the three groups, it was observed that toenails were more commonly involved than fingernails. Regarding types of OM, distal lateral subungual onychomycosis (DLSO) was more common in all studied groups, followed by total dystrophic onychomycosis (TDO) and proximal subungual onychomycosis (PSO) which approximately accounted for 72.5%, 21.5%, and 6.0% of total cases, respectively. Fungal culture showed that the commonest incriminating agents were dermatophytes constituting 87.5% cases, followed by yeasts and non-dermatophyte mold which together comprised 12.5% cases.
All three treatment groups had no significant difference in their mean OSI score at baseline (P > 0.84). The percentage of improvement in mean OSI score in all the three groups on completion of treatment and on the 12-week follow-up visit is depicted in Table 1.
| Parameters | Group A (n = 30) | Group B (n = 30) | Group C (n = 30) | Statistical test | P Value |
|---|---|---|---|---|---|
| OSI score at baseline (mean ± SD) | 24 ± 4.56 | 25 ± 5.21 | 24.4 ± 6.42 | ANOVA;0.74 | 0.84 |
| Percentage of improvement in mean OSI score at treatment completion (mean ± SD) | 72.42 ± 30.24 | 51.34 ± 29.12 | 22.72 ± 10.21 | Kruskal–Wallis test;7.4 | 0.03 |
| Significance between groups at treatment completion: P1 = 0.024, P2 = 0.032, P3 = 0.014 | |||||
| Percentage of improvement in mean OSI score 12 weeks after completion of treatment (mean ± SD) | 77.64 ± 32.76 | 53.46 ± 30.14 | 20.32 ± 16.42 | Kruskal–Wallis test;8.7 | 0.023 |
| Significance between groups 12 weeks after treatment completion: P1 = 0.012, P2 = 0.029, P3 = 0.004 | |||||
Group A = combined group, Group B = laser group, Group C = topical group: significance between the three groups, P1 = comparing between Groups A and B, P2 = comparing between Groups B and C, P3 = comparing between Groups A and C
Regarding the grade of clinical improvement on treatment completion, there was a significant difference between the three groups (P < 0.005), whereas 77.3% in group A showed marked clinical improvement versus 46.6% in group B versus 0% in group C [Table 2]. On intergroup comparison, it was found that the combined group showed a significantly better degree of clinical improvement than both the other groups (P1 = 0.024, P3 = 0.014), whereas the laser group showed significantly better results than the topical group (P2 = 0.032). Further, on follow-up visit 12 weeks after completion of treatment, the degree of improvement was still significantly better in the group A, followed by group B and then group C (P1 = 0.014, P2 = 0.026, and P3 = 0.033) as depicted in Table 2. Figures 1 and 2 show the clinical improvement in patients receiving the combined therapy.
| Parameters | Group A (N = 30) | Group B (N = 30) | Group C (N = 30) | Statistical test | P Value |
|---|---|---|---|---|---|
| At the completion of treatment | |||||
| None, n (%) | 0 (0) | 3(10.0) | 8(26.6) | Chi-square test;19.6 | P = 0.034 |
| Mild improvement, n (%) | 2(6.7) | 8(26.7) | 20(66.7) | ||
| Moderate improvement, n (%) | 6(20.0) | 5(16.7) | 2(6.7) | ||
| Marked, n (%) | 22(73.3) | 14 (46.6) | 0 | ||
| Significance between groups: P1 = 0.012, P2 = 0.020, P3 = 0.031 | |||||
| At 12 weeks after treatment completion | |||||
| None, n (%) | 0(0) | 3(10.0) | 9(30.0) | Chi-square test; 18.4 | P = 0.027 |
| Mild improvement, n (%) | 2(6.7) | 9(30.0) | 21(70.0) | ||
| Moderate improvement, n (%) | 6(20.0) | 5(16.7) | 0 | ||
| Marked improvement (%) | 22(73.3) | 13(43.7) | 0 | ||
| Significance between groups: P1 = 0.014, P2 = 0.026, P3 = 0.033 | |||||
Group A = combined group, Group B = laser group, Group C = topical group, P = significance between the three groups, P1 = comparing between Groups A and B, P2 = comparing between Groups B and C, P3 = comparing between Groups A and C
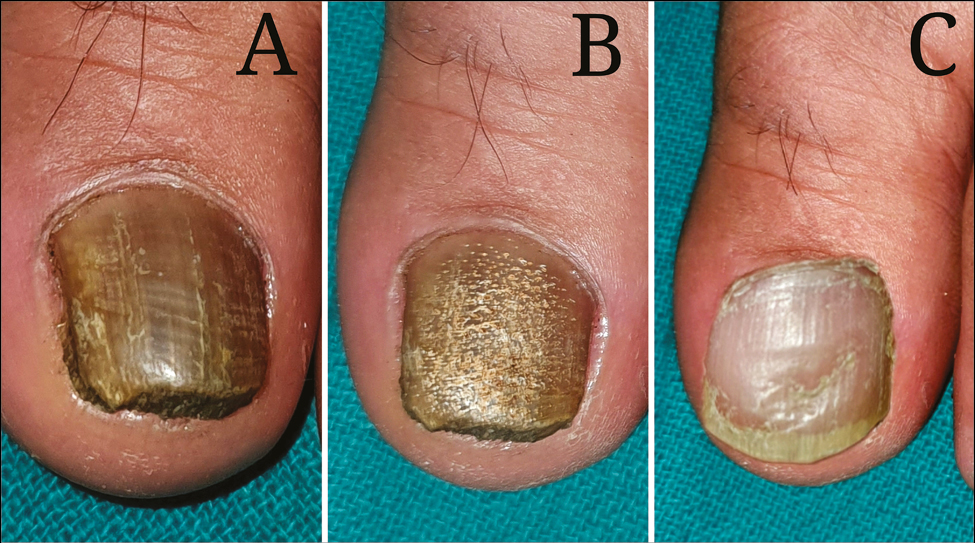
- Clinical results in combined group (laser + topical luliconazole 5% lotion) in a patient with toenail onychomycosis: (A) before treatment, (B) on third laser session, and (C) 12 weeks after treatment completion
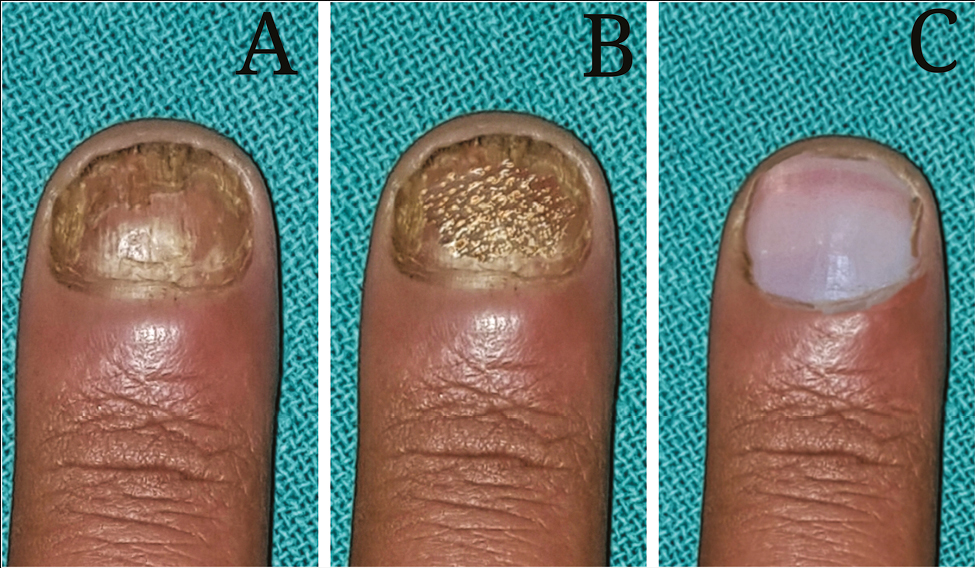
- Clinical results in combined group (laser + topical luliconazole 5% lotion) in a patient with finger-nail onychomycosis: (A) before treatment, (B) on second laser session, and (C) 12 weeks after treatment completion
Table 3 shows a significant difference between the three studied groups in KOH positivity and fungal culture on completion of treatment with best results shown by group A, followed by group B, and then by group C.
| Lab test | Group A (N = 30) | Group B (N = 30) | Group C (N = 30) | Statistical test | P Value |
|---|---|---|---|---|---|
| KOH Microscopy, n (%) | |||||
| Positive | 8 (26.7) | 16 (53.3) | 28 (93.3) | Chi-square test; 10.20 | 0.032 |
| Negative | 22 (77.3) | 14 (46.7) | 2 (6.7) | ||
| Significance between groups for KOH Microscopy: P1 = 0.026, P2 = 0.038, P3 = 0.016 | |||||
| Fungal culture, n (%) | |||||
| Positive | 4 (13.3) | 12 (40) | 24 (80) | Chi-square test;10.40 | 0.044 |
| Negative | 26 (86.7) | 18 (60) | 6 (20) | ||
| Significance between groups for fungal culture: P1 = 0.012, P2 = 0.029, P3 = 0.004 | |||||
Group A = combined group, Group B = laser group, Group C = topical group, P = significance between the three groups, P1 = comparing between Groups A and B, P2 = comparing between Groups B and C, P3 = comparing between Groups A and C
Regarding patient’s satisfaction, 70% of patients in group A were “very satisfied” versus 50% in group B and 0% in group C [Table 4].
| Parameters | Group A (N = 30) | Group B (N = 30) | Group C (N = 30) | Statistical test | P Value |
|---|---|---|---|---|---|
| Unsatisfied, n (%) | 0(0) | 3(10) | 8(26.6) | Chi-square test;18.4 | P = 0.024 |
| Mildly satisfied, n (%) | 2(6.7) | 8(26.7) | 20(66.7) | ||
| Moderately satisfied, n (%) | 7(23.3) | 4(13.3) | 2(6.7) | ||
| Very satisfied, n (%) | 21(70) | 15(50) | 0 | ||
| Significance between groups: P1 = 0.013, P2 = 0.021, P3 = 0.032 | |||||
Group A = combined group, Group B = laser group, Group C = topical group, P = significance between the three groups, P1 = comparing between Groups A and B, P2 = comparing between Groups B and C, P3 = comparing between Groups A and C
DISCUSSION
Due to its minimally invasive nature and potential to restore clear nail growth with relatively few sessions, lasers are emerging as a new modality of treatment for OM. Although the US Food and Drug Administration (FDA) has indicated that lasers have a role in nail clearance, but mere clearance does not ensure the eradication of dermatophytes. Further, because of paucity of comparative studies, the efficacy of lasers as the first line of management has not been yet established.
Fractional CO2 exerts its effect in OM by “selective photo-thermolysis,” wherein a short burst of laser light energy is delivered into the target tissue causing a rapid elevation in temperature into the defined target area.[9] Fungi are heat sensitive above 55°C, so laser-induced thermal heating of the mycelium is likely to result in fungicidal effects.[10] Also, fractional CO2 laser exfoliates the nail tissue that leads to diffuse remodeling and at the same time destroys the environment for fungal growth environment.[11] Being ablative in nature fractional CO2 laser serves as a primary treatment for OM or as an adjunct to topical antifungals, providing a means of penetration through the hard densely keratinized nail plate.
In our study, we found that fractional CO2 laser combined with topical luliconazole 5% lotion was effective for treating OM. Compared to baseline, the mean OSI score showed a significant decrease at the end of treatment and at 12 weeks of follow-up. Nearly 70% of the patients were markedly satisfied. Negative results in KOH microscopy and fungal cultures were found in 77.3% and 86.7% of patients, respectively, at the end of treatment. All these parameters were significantly lower in the laser group and the topical group. El-Tatawy et al.[12] carried a similar triple limb comparative study in which both laser and combined groups showed significantly better degrees of improvement, mycological cure and patient’s satisfaction in comparison with topical group. They also reported no significant difference in the cure rates of the combined group and laser group, suggesting that the laser group alone can more or less equally effective. On the contrary, our study showed that fractional CO2 laser combined with topical treatment had a significantly better efficacy than fractional CO2 laser treatment alone. Our results were in line with the results obtained by Zhou et al.[13] The plausible explanation may be that in the combined group the laser not only kills the fungi by its thermal effect but also creates passages for the penetration of topical agents into the nail plate resulting in overall improved efficacy than with treatment with either modality alone. Lim et al.[14] administered fractional CO2 with topical terbinafine and followed up for 3 months with a 50% complete response, whereas Shi et al.[15] in thirty cases with 124 nails found a clinical efficacy rate of 68.5%, 3 months after the last session. Bhatta et al.[16] used fractional CO2 with topical terbinafine for treating OM, and found that 73.32% of patients showed significant clinical cure and 92% attained negative culture 3 months after completion of treatment.
In the topical group, majority of the patients showed only “mild clinical improvement” on treatment completion. Also, by the end of the treatment, complete mycological cure as assessed with KOH microscopy and fungal culture was seen in only 6.7% and 20% cases, respectively. This poor efficacy of topical antifungals can be due to ineffective drug penetration into the nail plate. This was in line with a study done by Hay et al.[17] who reported a cure rate of only 22% using topical tioconazole 28% solution. Baran and Kaoukhov[18] also reported unsatisfactory results with topical antifungal monotherapy except in very mild cases.
Regarding adverse effects, moderate-to-severe pain, nail-fold swelling, and burning sensation were noted in 2.5% cases of combined and laser group each. Contact dermatitis was the main side effect in the topical group (20.5%).
Limitations
The limitations of this study were the smaller sample size and shorter duration of follow-up (12 weeks).
CONCLUSION
Fractional CO2 laser combined with a topical antifungal is a safe and effective treatment for OM, and its efficacy is superior to either modality used alone. However, further studies are needed for comparing the efficacy of fractional CO2 with other lasers (Nd:YAG, diode laser); and also to evaluate the ideal parameters of laser sessions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Incidence and epidemiology of onychomycosis in patients visiting a tertiary care hospital in India. Cutis. 2015;95:E20-5.
- [Google Scholar]
- The prevalence of onychomycosis in the global population: A literature study. J Eur Acad Dermatol Venereol. 2014;28:1480-91.
- [Google Scholar]
- Onychomycosis in the 21st century: An update on diagnosis, epidemiology, and treatment. J Cutan Med Surg. 2017;21:525-39.
- [Google Scholar]
- Oral antifungal medication for toenail onychomycosis. Cochrane Database Syst Rev. 2017;7:CD010031.
- [Google Scholar]
- Insights into drug delivery across the nail plate barrier. J Drug Target. 2014;22:769-89.
- [Google Scholar]
- Laser assisted drug delivery: A review of an evolving technology. Lasers Surg Med. 2014;46:249-62.
- [Google Scholar]
- Evaluation of nd:YAG laser device efficacy on onychomycosis: A case series of 30 patients. Mycoses. 2016;59:7-11.
- [Google Scholar]
- A new classification system for grading the severity of onychomycosis: Onychomycosis severity index. Arch Dermatol. 2011;147:1277-82.
- [Google Scholar]
- The effectiveness of laser treatments for onychomycosis in adults in the community: A systematic review protocol. JBI Database Syst Rev Implement Rep. 2013;11:1-15.
- [Google Scholar]
- Mammalian endothermy optimally restricts fungi and metabolic costs. mBio. 2010;1:e00212-10.
- [Google Scholar]
- A prospective trial of fungal colonization after laser resurfacing of the face: Correlation between culture positivity and symptoms of pruritus. Dermatol Surg. 2003;29:255-60.
- [Google Scholar]
- Fractional carbon dioxide laser and topical tioconazole in the treatment of fingernail onychomycosis. Lasers Med Sci. 2019;34:1873-80.
- [Google Scholar]
- The efficacy of fractional carbon dioxide (CO2) laser combined with luliconazole 1% cream for the treatment of onychomycosis: A randomized, controlled trial. Medicine (Baltimore). 2016;95:e5141.
- [Google Scholar]
- Toenail onychomycosis treated with a fractional carbon-dioxide laser and topical antifungal cream. J Am Acad Dermatol. 2014;70:918-23.
- [Google Scholar]
- The efficacy of fractional carbon dioxide (CO2) laser combined with terbinafine hydrochloride 1% cream for the treatment of onychomycosis. J Cosmet Laser Ther. 2017;19:353-9.
- [Google Scholar]
- Fractional carbondioxide (CO2) laser-assisted topical therapy for the treatment of onychomycosis. J Am Acad Dermatol. 2016;74:916-23.
- [Google Scholar]
- Tioconazole nail solution—an open study of its efficacy in onychomycosis. Clin Exper Dermatol. 1985;10:111-5.
- [Google Scholar]
- Topical antifungal drugs for the treatment of onychomycosis: An overview of current strategies for monotherapy and combination therapy. J Eur Acad Dermatol Venereol. 2005;19:21-9.
- [Google Scholar]






