Translate this page into:
Cicatricial Ectropion of Lower Eyelid: A Report of Two Cases
Address for correspondence: Dr. Sunil Sidana, Department of Oral and Maxillofacial Surgery, MGM Dental College and Hospital, Junction of NH4 and, Sion - Panvel Expy, Sector 18, Navi Mumbai, Maharashtra, India. E-mail: drsunilsidana@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Cicatricial lower lid ectropion is characterized by vertical shortening and/or scarring of the anterior lamella of eyelid and can be the result of thermal or chemical burns, mechanical or surgical trauma/scars, medications, sun damage, chronic inflammation, and involutional changes.
Ectropion repair presents a challenge to the surgeon. The surgical management of cicatricial ectropion depends on the situation after the release of the scar traction in the lower lid area. Various techniques have been described for correcting cicatricial ectropion by lengthening the anterior lamella with transposition flaps or with full-thickness free skin grafts.
We would like to describe two cases of lower lid cicatrical ectropion with two different causes, which were managed in two different ways.
Keywords
Cicatricial
ectropion
eyelid
flap
skin graft
INTRODUCTION
An ectropion is an eversion of eyelid margin in which the eyelid is pulled away from the globe. Most commonly occurs in the lower eyelid. It may be unilateral or bilateral. Ectropion can be congenital or acquired. Acquired ectropion constitutes of four categories: involutional, paralytic, cicatricial, and mechanical. Cicatricial lower lid ectropion is characterized by vertical shortening and/or scarring of the anterior lamella of eyelid and can be the result of thermal or chemical burns, mechanical, or surgical trauma/scars, medications, sun damage, chronic inflammation, and involutional changes.[1]
In maxilofacial surgery, it is most commonly found in patients operated through lower lid approaches, especially the subciliary approach to access midface trauma or orbital pathology.[234]
Ectropion repair presents a challenge to surgeons. Therefore, an individualized surgical approach based on thorough preoperative evaluation considering the etiology and the predominant location of the ectropion is necessary. We would like to describe two cases of lower lid cicatrical ectropion with two different causes, which were managed in two different ways.
CASE REPORT 1
A 29-year-old patient reported to our department with a draining sinus and exposed miniplate in the right infraorbital region [Figure 1]. The patient was operated for right zygomtico-maxillary complex fracture 4 years ago and plating was done via lower eyelid approach. On examination, there was cicatricial ectropion with the scleral show and epiphora with no evidence of chemosis or keratoconjuctivitis.

- Preoperative photograph of patient with cicatricial ectropion of lower eyelid following infection
SURGICAL TECHNIQUE
After the local infection was controlled with antibiotics, the patient was taken up for correction of cicatricial ectropion under general anesthesia. The scar tethering the lower eyelid just above the sinus region was released. Another incision was taken over the exposed plate to remove it [Figure 2]. Skin grafting was planned to cover the raw area left after the first incision. Template was marked at the right preauricular donor site measuring about 2 cm × 1 cm and full-thickness skin graft was harvested [Figure 3]. Graft was defatted and sutured to the defect using 4.0 ethilon [Figure 4]. Compressive bolster over graft was placed for 5 days postoperatively. Frost suture was placed securing the lower eyelid to forehead for 5 days. Bolster dressing was removed after 7 days and skin graft take was good. The patient was followed up for 1 year and was satisfactory with the outcome [Figure 5].

- Defect left after release of ectropion and removal of manipulate

- Foil used to measure the size of skin graft from preauricular region

- Skin graft sutured to the recipient site

- Postoperative photograph at 1-year follow-up
CASE REPORT 2
A 18-year-old patient came to our department with a history of facial abrations sustained 1 month ago following road traffic accident . On examination, multiple scarring over left side of face was noticed along with lower lid eversion due to scarring from healed abrasions [Figure 6].
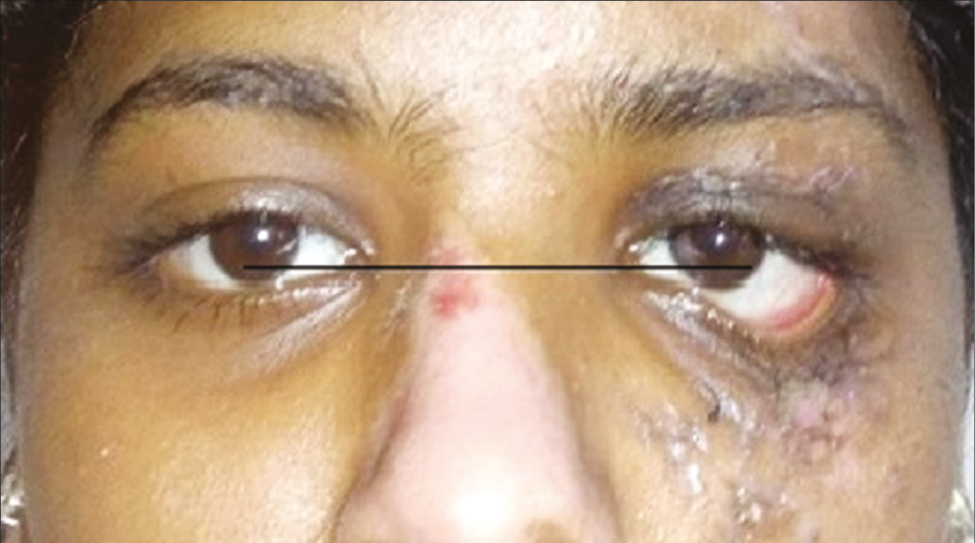
- Preoperative photograph of patient with left lower eyelid cicatricial ectropion following facial abrasion
Surgical technique
Similar to the first case, the scar was released [Figure 7] Defect left after scar release was deep. Covering this defect with skin graft would have left her with unesthetic appearance. Hence, plan was changed and transposition flap from adjacent cheek was raised and rotated into the defect [Figures 8 and 9]. At 1-year follow-up, the patient was happy with the outcome [Figure 10].

- Defect after release of ectropion

- Marking of a transposition flap

- Transposition flap rotated into the defect

- Postoperative photograph at 1-year follow-up
DISCUSSION
The surgical management of cicatricial ectropion depends on the situation after the release of the scar traction in the lower lid area.[5] Various techniques have been described for correcting cicatricial ectropion by lengthening the anterior lamella with transposition flaps or with full-thickness free skin grafts[56789] [Table 1].
| 1. Full thickness skin graft (preauricular, post auricular, upper eyelid, supraclavicular) |
| 2. Transposition flap from cheek (rhombic, nasolabial flap) |
| 3. Tripier flap unipedicle or bipedicle from upper eyelid |
| 4. Z plasty |
| 5. V to Y plasty |
| 6.Mustarde’ cheek rotation transposition flap |
| 7. Lateral tarsal stip combined to any of the above options |
The defects resulting from the release of ectropion include the skin and orbicularis oculi, which comprise the anterior lamella of the eyelid. Skin grafting in conjunction with tightening of the lower lid, especially in elderly patients, has been the standard method of reconstruction in these cases.[10]
The ideal donor site for skin graft for eyelid reconstruction is the periocular region, which is characterized by the same color and thickness.[6] Skin graft can also be obtained from the postauricular and preauricular region. Choi et al.[7] performed a retrospective, noncomparative chart review of patients who underwent lower eyelid ectropion repair with placement of a full-thickness skin graft between June 2004 and March 2014. They noticed 100% viability of the skin grafts.
A traditional skin graft is a simple and convenient method, but the texture, thickness, and color of skin grafts in the repaired region are not in harmony with the surrounding skin, especially in East Asians. In the long term, the different degrees of contracture of grafted skin affect the lower eyelid function and appearance. Also adaptation of the graft to the recipient bed needs utmost care postoperatively.[10]
To overcome the disadvantages of skin grafts, a great variety of cutaneous and mycocutaneous flaps from face and scalp close to the eyelids have been used to repair lower eyelid wounds after correction of ectropion to improve the function of the lower eyelid. The main advantages of these flaps are one-stage reconstruction, good color and texture match, and reliable vascularity leading to success of the flap.[11] Each flap has its advantages and disadvantages, and the surgeon has to decide and justify his flap selection.
In our cases, both the defects were near the infraorbital region. Unipedicle or bipedicle flap from upper eyelid is a good option for lower eyelid reconstruction due to good skin color match and texture. The disadvantages are limited width of skin flap and two-stage reconstruction. In the first case, skin grafting was done after ectropion release as defect was more than 1.5 cm and to avoid two stage. But in the second case as the scar was below the infraorbital rim; the defect was found to be deep and skin graft would have given a crater effect after healing; hence, a local transposition flap was decided and executed and results were satisfactory. A lateral canthal tightening procedure for lateral eyelid laxity is sometimes required in managing cicatricial ectropion. In our cases, the second patient would have benefitted from the lateral canthal tightening procedure.
CONCLUSION
Cicatricial ectropion management is challenging and each case needs to be treated individually.
Practice points
Cicatricial ectropion is secondarily to retraction of anterior lamella of the eyelid
Successful management depends on preoperative evaluation of cause and severity.
There are various options for management of cicatricial ectropion. The option with least morbidity and optimal aesthetics should be selected.
Cicatricial ectropion is a complication that demands an adjusted and personalized surgical treatment.
Ethical policy and institutional review board statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
- Vertical-to-horizontal rotational myocutaneous flap for repairing cicatricial lower lid ectropion: a novel surgical technique. Biomed Res Int. 2017;2017:8614580.
- [Google Scholar]
- Surgical approaches to the infraorbital rim and orbital floor: the case for the subtarsal approach. J Oral Maxillofac Surg. 2006;64:104-7.
- [Google Scholar]
- Lower eyelid complications in facial fracture surgery. J Craniofac Surg. 2017;28:391-3.
- [Google Scholar]
- The incidence of lower eyelid malposition after facial fracture repair: A retrospective study and meta-analysis comparing subtarsal, subciliary, and transconjunctival incisions. Plast Reconstr Surg. 2009;124:1578-86.
- [Google Scholar]
- Management of lower lid ectropion. Dermatol Surg. 2006;32:1050-6; discussion 1056-7.
- [Google Scholar]
- Our approach to operative treatment of lower lid ectropion. Acta Clin Croat. 2010;49:283-7.
- [Google Scholar]
- Full-thickness skin graft as an independent or adjunctive technique for repair of cicatricial lower eyelid ectropion secondary to actinic skin changes. Ophthal Plast Reconstruc Surg. 2015;31:474-7.
- [Google Scholar]
- Viability of full-thickness skin grafts used for correction of cicatricial ectropion of lower eyelid in previously irradiated field in the periocular region. Head Neck. 2013;35:103-8.
- [Google Scholar]
- Bipedicle myocutaneous flap repair of cicatricial ectropion. Ophthalmic Plast Reconstr Surg. 1990;6:119-21.
- [Google Scholar]
- Orbicularis oculi myocutaneous flap in reconstruction of postburn lower eyelid ectropion. Burns. 1999;25:553-7.
- [Google Scholar]
- Reconstruction of lower eyelid retraction or ectropion using a paranasal flap. Aesth Plast Surg. 2012;36:611-7.
- [Google Scholar]






