Translate this page into:
Combined Therapy with Laser and Autologous Topical Serum for Facial Rejuvenation: A Multiple Case Series Report
Address for correspondence: Dr. Eduardo Anitua, Eduardo Anitua Foundation, Vitoria, Jacinto Quincoces 39, 01007 Vitoria (Alava), Spain. E-mail: eduardo@fundacioneduardoanitua.org
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Lasers require several sessions to achieve significant results and may lead to adverse reactions. Platelet-rich plasma (PRP) therapy is a good adjuvant to laser therapies; however, repeated blood extractions and invasive injections are needed. A 100% autologous topical formulation based on the patient’s proteins has been recently developed, known as Endoret-Serum (ES). Unlike other PRPs, ES provides a home care, storable, and topical needle-free application.
Objective:
Preliminarily assess the clinical performance of a single session of the combined therapy with nonablative laser and ES in the management of cutaneous pigmented and vasculature lesions.
Materials and Methods:
Nine patients with clinical signs of skin aging received a single session of nonablative laser. ES was topically applied twice daily. They were clinically assessed after 1 and 8 weeks. VISIA-CR System was used for high-resolution topographic analysis. Subjects were asked to complete a self-assessment questionnaire and an impression of improvement survey. An investigator’s global assessment scale was fulfilled.
Results:
The combined treatment improved cutaneous spots, wrinkles, and texture after 8 weeks, whereas significant pore reduction was observable at 1 week. Ultraviolet (UV) spots and porphyrins decreased at 1 week, whereas red area improvement was noticeable after 8 weeks. Overall wrinkle amelioration, periorbital hyperpigmentation decrease, softened skin, and tone recovery was observed. Patients referred to be very satisfied and felt that their cutaneous condition was much better. At the end of the study, subjects presented minimal dermatological symptoms like pigmented lesions, redness, or capillaries. No side effects were reported.
Conclusion:
Results presented herein suggest that one session of laser in combination with ES provides a good clinical outcome.
Keywords
Autologous topical serum
laser
platelet-rich plasma
skin rejuvenation
INTRODUCTION
The term laser in dermatology is an acronym that means “light amplification by the stimulated emission of radiation.” It is based on the use of a high energy beam at low wavelength that produces a thermal impact into the skin aimed to destroy altered cutaneous structures. Lasers can be accurately focused into small spots due to their monochromatic, coherent, and collimated properties. This allows the performance of radiation beams at a single wavelength, in-phase waves, and parallel traveling, respectively.[1] In the last years, laser technology has been adapted for the treatment of many skin conditions including vascular and pigmented lesions, tattoo removal, scars, and wrinkles. There are several types of lasers that work at different wavelength peaks, pulse durations, and absorption range that determine their clinical application.[2]
Nonablative lasers, create microscopic heat columns causing areas of thermal damage separated by normal skin that are a healthy reservoir for tissue regeneration. Ablative lasers lead to full-thickness tissue destruction over areas to be deeply remodeled. Nonablative lasers leave a functionally and histologically intact stratum corneum with minimal disruption of the epidermis.[3] They work by delivering a precise wavelength light below the skin’s surface that is absorbed by specific dermal structures. This destroys target areas that do not harm the surrounding tissue. In addition, short pulses decrease de amount of heat transferred to cells thereby reducing thermal damage that could result in scarring. This type of treatment is usually aimed to improve skin texture and tone, reduce fine lines and mild wrinkles or eliminate pigmentation and vasculature issues such as capillaries.[4]
Nonablative lasers are comparatively less invasive, and they are usually associated with lesser efficacy as they need several sessions to achieve significant results. Moreover, despite the reduction in adverse symptoms, post-treatment events still arise due to the repeated dosage. These include temporary hyperpigmentation, persistent erythema, edema, swelling, and redness with an incidence of 15%.[5] Hence, new custom-tailored treatments with optimal safety profile and therapeutic efficacy are demanded by clinicians as adjunctive tools to boost the resurfacing effect of nonablative lasers and minimize adverse reactions.
In this line, the progression in the field of autologous treatments has led to the emergence of products based on the patient’s own proteins. Preparations like platelet-rich plasma (PRP) have shown their efficacy and safety in different dermatological applications.[6] In fact, numerous findings reveal that the combination of ablative lasers and platelet-based formulations promotes cutaneous remodeling more efficiently.[7] When managing atrophic lesions such as acne scars or facing cutaneous resurfacing, studies report shorter downtime, better tolerability, and improved skin quality after PRP treatment.[89] However, these interventions require repeated blood extractions and invasive and painful intradermal injections of PRP during the treatment period to reach the desired effect.
In this sense, a topical formulation based on plasma rich in growth factors technology (PRGF) has been recently developed.[10] This product, known as Endoret-Serum (ES), is 100% autologous and can be in situ prepared after a single session of blood withdrawal.[11] ES maintains its physicochemical and biological properties after long-term storage and contains a pool of growth factors that undergo a sustained percutaneous absorption playing a major role in cutaneous regeneration.[12] Unlike other PRPs, ES has been designed for a home care and topical needle-free application with no need of physician intervention or repeated blood extractions. Thus, ES provides a minimally invasive approach for maintaining a constant dosage of growth factors that might boost the resurfacing effect of lasers and minimize adverse reactions. The aim of this study was to preliminarily assess the clinical performance of a single session of the combined therapy with nonablative laser and ES in the management of facial rejuvenation.
MATERIALS AND METHODS
Ethical statement
The study was conducted following the principles established in the Declaration of Helsinki amended in 2013 and patients gave their informed consent. This study included medical treatments that are applied in the regular clinical practice under healthcare professional prescription.
Patients
Following a retrospective design, patients between 18 and 70 years old from “Aesthetic and Dermatological Centre” (Alicante, Spain) were included in the study. A total of nine patients with clinically diagnosed sings of aged skin within the facial area were treated. Patients that did not apply for the combined therapy included pregnant or lactating patients, active inflammation in the intervention area, systemic infections, cancerous lesions for 5 years before the beginning of the treatment, connective tissue disease, a history of rheumatic disorders, hematological alterations, current treatment with immunosuppressants or anticoagulants, presence of permanent facial implants, and allergy to hematological derivatives.
Endoret-Serum preparation
Manufacturer’s instructions were followed for ES preparation (KMU10-TPC, BTI Biotechnology Institute, Vitoria, Spain). Peripheral blood was harvested into 9-mL collection tubes containing 0.4 mL of 3.8% (wt/v) trisodium citrate as anticoagulant. Afterward, the blood was centrifuged at 580G for 8 min (System V, BTI Biotechnology Institute). The whole plasma column was collected, avoiding the leukocyte-rich buffy coat. Part of the plasma was thermally gelated at 76°C for 12 min (Plasmaterm II, BTI Biotechnology Institute). The remaining plasma was activated with calcium chloride following manufacturer’s instructions and incubated at 37°C for 40 min for fibrin clot formation (Plasmaterm I, BTI Biotechnology Institute). After clot retraction, the obtained supernatant was vigorously mixed with the gelated plasma in a 1:2 ratio and dispensed into airless pump bottles that were specially designed to avoid external air intake.
Combined therapy
Patients were treated with a combination of ES and nonablative laser therapy. First, the patients underwent a single laser resurfacing session with either alexandrite or pulsed dye laser (PDL) adjusted at 755 nm and 595 nm, respectively (V-Beam II, Candela, Madrid, Spain). Afterward, a single extraction of peripheral blood and personalized ES preparation was carried out as described above. The product was given to the patients and cold stored at 4°C in their regular home fridge for homecare application. The ES was applied over the face twice daily. Prior application patients cleansed their face and washed their skin with water. Then the product was applied over the face using slight rubbing movements and was left to air dry. Patients underwent an uninterrupted treatment of ES for 8 weeks.
Clinical assessment
Participants were clinically assessed at baseline, just after the laser session and at 1 and 8 weeks after the beginning of the treatment. Any undesired side effects or adverse reactions were recorded. The clinical assessment was performed by trained technicians in a controlled environment regarding room temperature and humidity. The assessment was carried out using the VISIA-CR System (Canfield Imaging Systems, Fairfield, New Jersey) to obtain high-resolution facial photographs. Several skin parameters were recorded including spots, wrinkles, texture, pores, ultraviolet (UV) spots, brown spots, red area, and porphyrins. In addition, subjects were asked to complete a self-assessment questionnaire and rated their satisfaction following a Likert’s 10-point scale. Patients also fulfilled a global impression of improvement survey (PGI-I) comparing their post-treatment condition to baseline. For the clinical objectivation of the dermatological symptoms, images from each patient were evaluated by two trained specialists who were asked to complete an investigator’s global assessment (IGA) scale.
Statistical analysis
Statistical analysis was performed using R computing environment.[13] After assessing normality of distribution (Shapiro–Wilk normality test) and sphericity (Mauchly test), mixed-effect linear models were constructed for the dependent variables. The function lme in the package nlme was used, considering the interaction between treatment and time point as fixed effects and patient as random effects.[14] Moreover, an autocorrelation structure was included with corAR1. Type-II analyses of variance (ANOVA) were applied for repeated factorial measures. Linear models of mixed effects and estimated marginal means (EMMs) were calculated for significant factors or combination of factors using the function emmeans from the package lsmeans with Tukey adjustment. The applied statistical significance level was 5% (P ≤ 0.05).
RESULTS
The study included nine women whose age ranged from 29 to 63 years being the average 54 ± 11 years. Patients presented slight-to-moderate skin aging signs such as pigmented lesions, redness, and capillaries (Goglau’s grade I–II). The main clinical symptoms to be treated included cutaneous vascular lesions like telangiectasis (11%), age spots related to solar lentigines (55%), and dermatoses like rosacea (34%). During the follow-up period no adverse effects related to the treatment were observed. Moreover, patients did not need maintenance therapy after the follow-up period.
Results showed that the combined therapy improved cutaneous spots, wrinkles, and texture after 8 weeks, whereas significant pore reduction was observable at 1 week [Figure 1] (P ≤ 0.05). Spot, wrinkle, and texture index showed a significant fold improvement of 1.95 ± 2.6, 1.42 ± 1.4, and 1.8 ± 0.8 compared to baseline, respectively. Pore reduction showed a significant fold improvement of 1.33 ± 0.5. Similarly, UV spot and porphyrin decrease reached statistically significant values at 1 week, whereas red area improvement was noticeable after 8 weeks [Figure 2] (P ≤ 0.05). UV spot and porphyrin showed a significant fold improvement of 4.42 ± 3.4 and 1.85 ± 1.7, respectively. Red area showed a 1.8 ± 1.2-fold improvement compared to baseline. Although brown spots showed a slight improvement after 1 week, the statistical significance was not reached (3.76 ± 6.4-fold improvement).
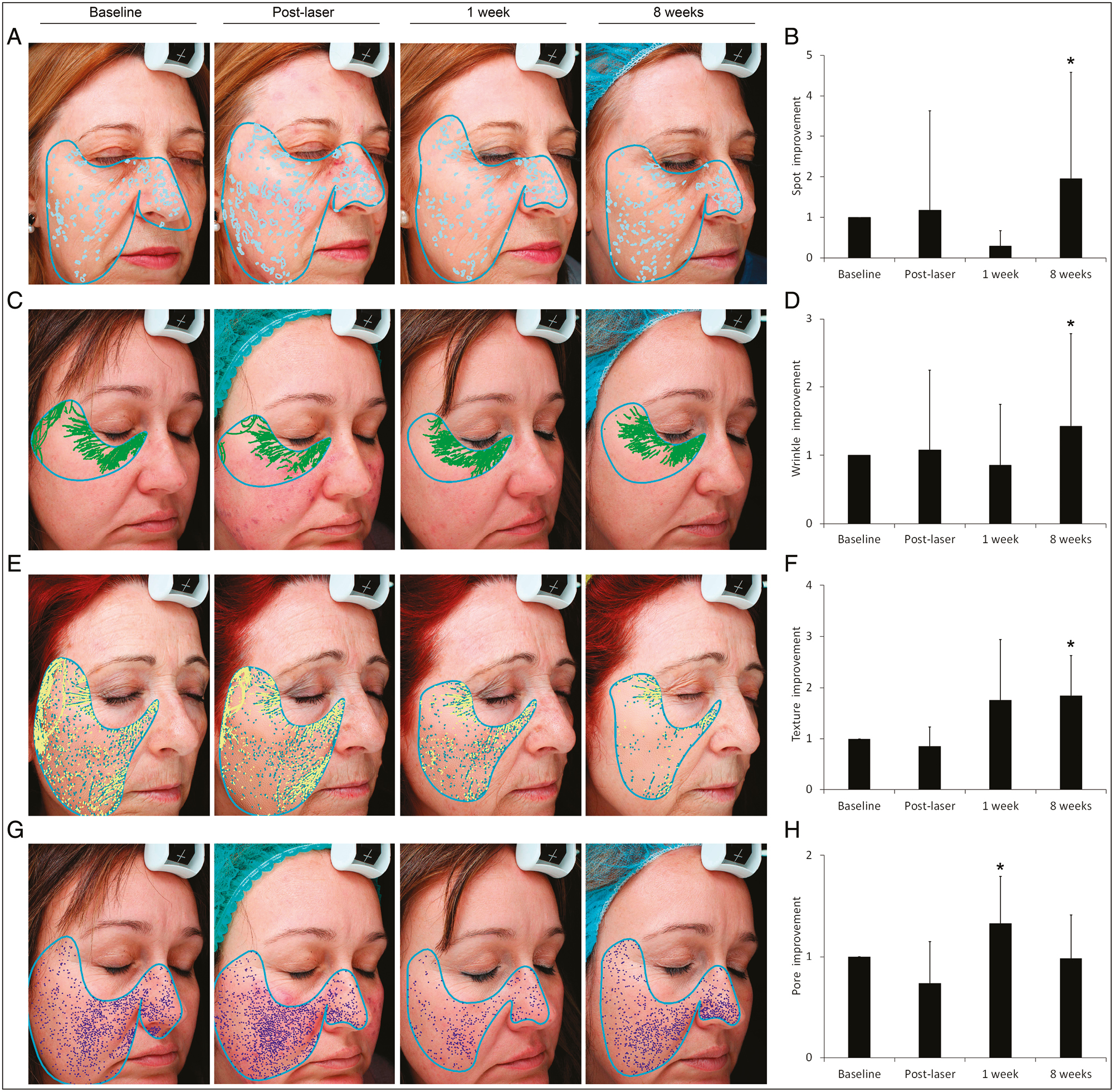
- Skin complexion analysis using the VISIA-CR System. (A and B) Combined treatment showed to improve spot percentile after 8 weeks. (C and D) Wrinkle reduction was noticeable at 8 weeks. (E and F) Texture improvement achieved the statistical significance after 8 weeks. (G and H) Pore index decreased 1 week after treatment. *Statistically significant differences compared to baseline (*P ≤ 0.05)
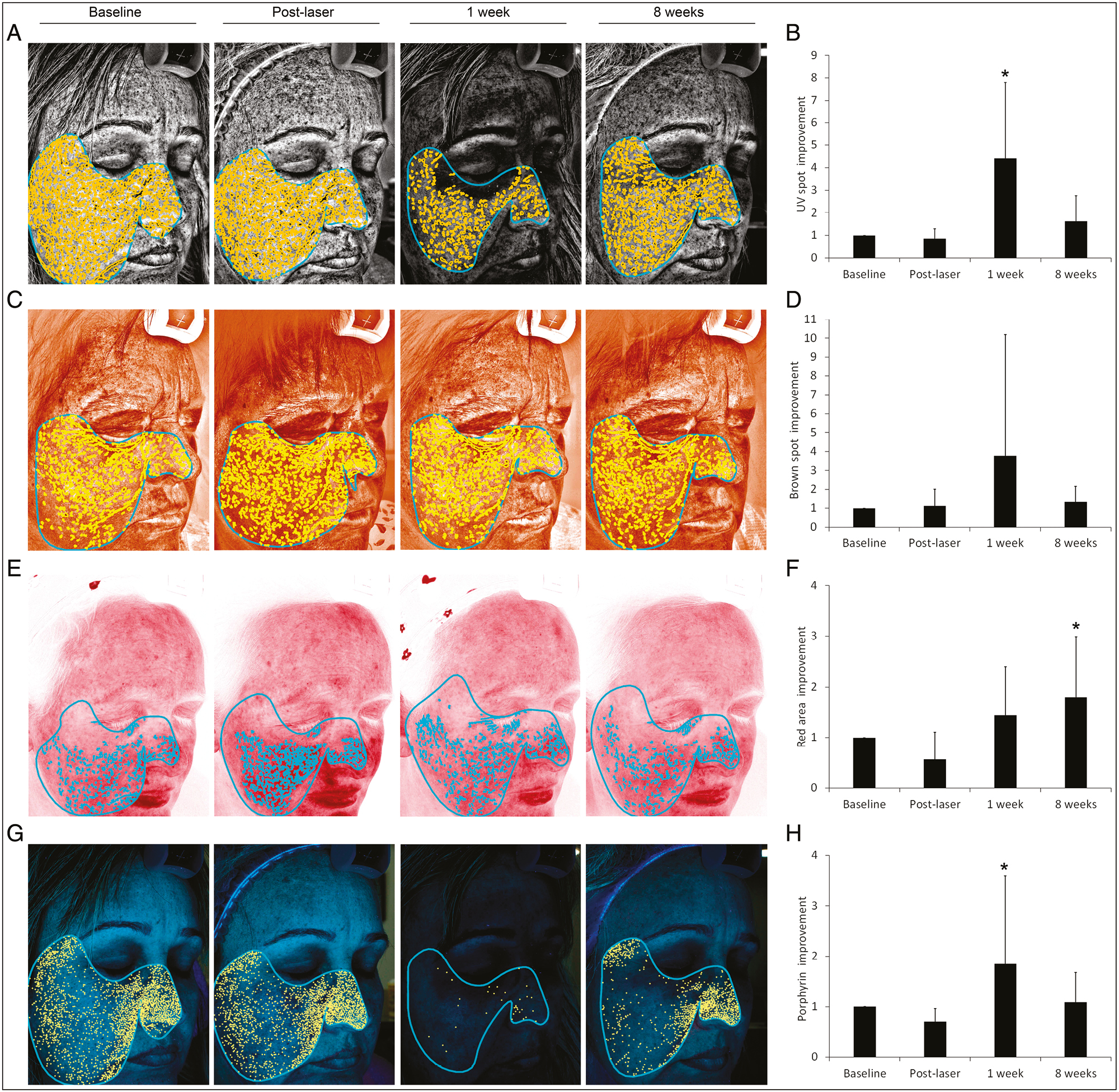
- Skin complexion analysis using the VISIA-CR System. (A and B) Combined treatment showed to improve UV spot percentile after 1 week. (C and D) Although brown spots showed a slight improvement after 1 week, the statistical significance was not reached. (E and F) Red area improvement achieved the statistical significance after 8 weeks. (G and H) Porphyrin index decreased 1 week after treatment. *Statistically significant differences compared to baseline (*P ≤ 0.05)
Standardized images revealed that after the laser session, mild erythema, local edema, and slight redness and bruising occurred over the facial area. However, following ES treatment these symptoms disappeared after 24 or 48 h, and the final clinical outcome revealed a noticeable skin quality improvement [Figure 3]. At the end of the follow-up period, overall wrinkle amelioration, periorbital hyperpigmentation decrease, softened skin, and tone recovery was observed. Moreover, the combined therapy helped in the lessening of facial static lines and the reduction of the uneven surface texture. The skin brightness also improved [Figure 3]. Pigmented lesions and vasculature issues like redness and capillaries decreased noticeably.

- Standardized facial photographs of patients during the study at baseline, just after the laser treatment and at the end of the follow-up period
Patients fulfilled a personal satisfaction survey during the study based on a Likert’s 10-point scale. After 1 and 8 weeks, patients referred to be satisfied and very satisfied, respectively [Table 1]. Regarding the global impression of improvement, patients also referred that their cutaneous condition was much better after the combined therapy compared to baseline [Table 1]. Moreover, two trained specialists checked the follow-up images of each patient and concluded that subjects presented minimal dermatological symptoms of skin aging compared to the baseline status [Table 1].
| Survey | Objective | Score | One week | Eight weeks |
|---|---|---|---|---|
| Likert’s satisfaction score (patient survey) | Overall satisfaction | 0–1: very dissatisfied
2–3: dissatisfied 4–6: indifferent 7–8: satisfied 9–10: very satisfied |
7.2 ± 0.8 | 8.1 ± 0.5 |
| PGI-I (patient global impression of improvement) | Posttreatment condition compared to baseline | 1: very much better
2: much better 3: a little better 4: no change 5: a little worse 6: much worse 7: very much worse |
2.6 ± 0.8 | 2.3 ± 0.9 |
| IGA (investigator’s global assessment) | Clinical objectivation of dermatological symptoms | 0: resolved symptoms
1: minimal symptoms 2: mild symptoms 3: moderate symptoms 4: marked symptoms 5: severe symptoms |
1.6 ± 0.5 | 0.3 ± 0.8 |
DISCUSSION
Previous studies have investigated the role of PRGF as an assisted therapy for laser resurfacing.[15] These types of treatments are usually based on the extraction of a limited plasma volume which is intradermally injected in combination with a variety of lasers for managing cutaneous conditions such as atrophic post-acne scars or irradiation symptoms.[16] The therapy combines ablative CO2 and erbium YAG lasers, which are based on the concept of selective photo-thermolysis, with autologous platelets and growth factors due to their regenerative potential once released at the site of injection.[8] In this sense, the bioactive molecules derived from the patient’s own blood have been shown to reduce fibrotic tissue and to decrease the duration and severity of laser-related side effects.[9]
Platelet-derived bioproducts have also been used as an adjuvant therapy among less potent lasers with the aim of promoting cutaneous repair during repeated irradiation sessions.[1718] In this study, nonablative alexandrite and PDLs were used for the management of facial resurfacing. These lasers were cleared by the FDA to manage cutaneous inflammatory conditions and treat pigmented lesions. Today these lasers are considered the laser of choice for most congenital and acquired vascular lesions as they promote skin remodeling by direct cutaneous immunologic activation. Several skin conditions have been successfully treated with alexandrite and PDLs including acne, psoriasis, spider veins, or age spots showing improvements in dyspigmentation and new collagen and elastic tissue deposition.[1920]
The alexandrite laser incorporates specific crystals as the laser source and produces an infrared wavelength of light to treat pigmented lesions without affecting the surrounding skin. The micro-damaged areas launch the healing process so that the collagen is restructured, the skin is tightened, and the skin texture is improved. Hence, this technique involves the controlled destruction of the superficial layers of the skin, by means of successive passes of the laser beam over the area to be treated.[20] The PDL penetrates the skin to reach target chromophores at the blood vessels. Its energy is absorbed by oxyhemoglobin to coagulate and cleanse the capillaries with a great tolerance and low melanin absorption. The absorbed light is converted in thermal energy thereby damaging surrounding cells. The pulse duration is shorter than the thermal relaxation time, which is the time taken for cooling after irradiation, ensuring that the impact is limited to the target structure. PDL allows to treat scars caused by acne, spider veins, spots, and birthmarks.[19]
However, these types of lasers usually require repeated sessions and when the energy beam is nonselectively diffused and is absorbed by surrounding tissues, complications and adverse effects may occur. These include pain, redness, swelling, itching, blistering, hyperpigmentation, bruising, and infection.[5] In addition, PRP-derived formulations are invasively injected at a dermal level following varying treatment regimens which may lead to discomfort and aggravate the damaged surface condition of the skin. In this study, a novel topical formulation (ES) has been tested as an autologous adjunctive therapy for nonablative resurfacing to promote facial rejuvenation after a single session of fractional laser. ES derives from PRGF, which is a specific type of PRP. PRGF allows versatile modifications of plasmatic physicochemical properties with the aim of designing custom-tailored bio-products that meet specific clinical needs.[21] In fact, other formulations derived from PRGF such as eye drops, gel-like fillers, or fibrin clots have been already evaluated in different medical fields including ophthalmology, oral surgery, traumatology, and dermatology.[22232425] For this purpose, ES provides a home care, storable and topical needle-free application that can be used in combination with laser rejuvenation.
Results of the skin complexion analysis presented herein showed that ES boosted the resurfacing effect of a single session of nonablative laser. Patients fulfilled specific surveys and dermatological life quality questionnaires regarding the clinical outcome of the combined therapy. In line with previous reports, participants and physicians referred a noticeable improvement of the aging signs and final satisfaction with no reported side effects.[262728]
Data from high-resolution topography of the skin showed that spots and UV marks, which are related to altered pigmentation and melanin accumulation below the cutaneous surface, improved significantly. This is consistent with other reports in which PRGF shown to reduce cutaneous photo-oxidative damage and actinic elastosis.[2930] In fact, ES downregulates UV-derived free radical accumulation and prevents DNA cleavage that occurs after solar exposure by means of antioxidant enzyme activation.[3132]
Wrinkled surface and skin texture, detected as irregular and uneven topography of the skin, also presented a noticeable improvement. These results are consistent with previous studies where high-resolution imaging revealed both an increased skin quality and hydration restoration after PRGF.[33] The high load of growth factors of ES has been shown to penetrate the stratum corneum in a sustained manner after smooth surface extension and might be involved in the remodeling of the dermal extracellular matrix. These growth factors include epidermal growth factor (EGF), insulin-like growth factor-I (IGF-I), platelet-derived growth factor-AB (PDGF-AB), and transforming growth factor-β1 (TGF-β1).[12] Moreover, these bioactive proteins promote dermal fibroblast activity by inducing cell proliferation and migration while increasing the biosynthesis on new collagen and hyaluronic acid which may explain the clinical outcomes observed herein.[10]
In addition, red areas associated with undelaying vascular conditions such as telangiectasis and rosacea that are common in the aged skin also proved to improve significantly after the combined therapy. Skin redness usually develops after papillary dermal vasodilation with an increased local level of hemoglobin. In this study, a single laser session and topical ES showed to modulate the inflammatory response of the skin and ameliorate laser side effects such as local erythema, burning, and redness. In fact, previous studies have shown the anti-inflammatory potential of ES which may be related to the downregulation of the nuclear-factor-κβ (NF-κβ) pathway and the reduction of inflammatory cytokines such as IL-1, IL-8, or TNF-alpha in response to autologous proteins.[3435]
In line with previous reports, skin pore number and porphyrin reduction were also observed during the follow-up period.[33] Pores are an important entrance way of bacteria which may lead to over-colonization and acne development thus enhancing porphyrin production. In this sense, the combined therapy might help in the renewal of the dermo-epidermal layers of the skin and prevent commensal bacterial growth and sebum overproduction. In fact, previous studies have shown the antibacterial activity of several proteins within PRGF and derivatives, which may help in the prevention of surface infection.[36]
To the best of author’s knowledge, this is the first study where a platelet-based 100% autologous topical product is used in combination with laser therapy for the management of pigmented and vasculature issues. However, it presents important limitations in the design such as the low sample size, the short follow-up period, and the absence of a control group. Hence, additional randomized and controlled clinical trials are needed to clearly assess the efficacy and safety of ES as an adjuvant therapy for laser. Nevertheless, this pilot study provides valuable preliminary data that would support further research involving the therapeutic use of ES. Results presented herein suggest that one session of laser resurfacing in combination with ES provides a good clinical outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
- An overview of laser in dermatology: The past, the present and … the future (?) Open Access Maced J Med Sci. 2017;5:526-30.
- [Google Scholar]
- Fractional photothermolysis: A new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34:426-38.
- [Google Scholar]
- Short-term side effects of fractional photothermolysis. Dermatol Surg. 2005;31:1245-9.
- [Google Scholar]
- Opening new horizons in regenerative dermatology using platelet-based autologous therapies. Int J Dermatol. 2017;56:247-51.
- [Google Scholar]
- A meta-analysis of the evidence for assisted therapy with platelet-rich plasma for atrophic acne scars. Aesthetic Plast Surg. 2019;43:1615-23.
- [Google Scholar]
- A meta-analysis of fractional Co2 laser combined with Prp in the treatment of acne scar. Lasers Med Sci. 2021;36:1-12.
- [Google Scholar]
- Efficacy of autologous platelet-rich plasma combined with ablative fractional carbon dioxide laser for acne scars: A systematic review and meta-analysis. Aesthet Surg J. 2019;39:NP279-87.
- [Google Scholar]
- A novel protein-based autologous topical serum for skin regeneration. J Cosmet Dermatol. 2020;19:705-13.
- [Google Scholar]
- The management of postsurgical wound complications with plasma rich in growth factors: A preliminary series. Adv Skin Wound Care. 2020;33:202-8.
- [Google Scholar]
- Long-term stability of a novel platelet-rich plasma-based topical serum for cutaneous applications. J Cosmet Dermatol. 2021;20:854-61.
- [Google Scholar]
- R. Core. R: A language and environmental for statistical computing. Vienna: R. Foundation for Statistical Computing.
- Combination of CO2 fraxional laser and plasma-rich growth factor (PRGF) for face rejuvenation. Cosmet Med. 2012;33:222-4.
- [Google Scholar]
- Lasers, microneedling, and platelet-rich plasma for skin rejuvenation and repair. Facial Plas Surg Clin. 2018;26:455-68.
- [Google Scholar]
- Platelet-rich plasma combined with fractional laser therapy for skin rejuvenation. Dermatol Surg. 2012;38:623-30.
- [Google Scholar]
- Treatment of traumatic scars using fat grafts mixed with platelet-rich plasma, and resurfacing of skin with the 1540 nm nonablative laser. Clin Exp Dermatol. 2012;37:55-61.
- [Google Scholar]
- The efficacy of pulsed dye laser treatment for inflammatory skin diseases: A systematic review. J Am Acad Dermatol. 2013;69:609-15.e8.
- [Google Scholar]
- The histology of skin treated with a picosecond alexandrite laser and a fractional lens array. Lasers Surg Med. 2016;48:646-52.
- [Google Scholar]
- Perspectives and challenges in regenerative medicine using plasma rich in growth factors. J Control Release. 2012;157:29-38.
- [Google Scholar]
- Comparison of intra-articular injections of plasma rich in growth factors (Prgf-endoret) versus durolane hyaluronic acid in the treatment of patients with symptomatic osteoarthritis: A randomized controlled trial. Arthroscopy. 2013;29:1635-43.
- [Google Scholar]
- Autologous serum and plasma rich in growth factors in ophthalmology: Preclinical and clinical studies. Acta Ophthalmol. 2015;93:e605-14.
- [Google Scholar]
- Plasma rich in growth factors: Preliminary results of use in the preparation of future sites for implants. Int J Oral Maxillofac Implants. 1999;14:529-35.
- [Google Scholar]
- Effectiveness of autologous preparation rich in growth factors for the treatment of chronic cutaneous ulcers. J Biomed Mater Res Part B Appl Biomater. 2008;84:415-21.
- [Google Scholar]
- Plasma rich in growth factor gel as an autologous filler for facial volume restoration. J Cosmet Dermatol. 2020;19:2552-9.
- [Google Scholar]
- Autologous platelet-rich gel for facial rejuvenation and wrinkle amelioration: A pilot study. J Cosmet Dermatol. 2019;18:1353-60.
- [Google Scholar]
- An autologous protein gel for soft tissue augmentation: In vitro characterization and clinical evaluation. J Cosmet Dermatol. 2019;18:762-72.
- [Google Scholar]
- Benefits of plasma rich in growth factors (PRGF) in skin photodamage: Clinical response and histological assessment. Dermatol Ther. 2015;28:258-63.
- [Google Scholar]
- Plasma rich in growth factors enhances wound healing and protects from photo-oxidative stress in dermal fibroblasts and 3d skin models. Curr Pharm Biotechnol. 2016;17:556-70.
- [Google Scholar]
- A novel autologous topical serum based on plasma rich in growth factors technology counteracts ultraviolet light-derived photo-oxidative stress. Skin Pharmacol Physiol. 2020;33:67-81.
- [Google Scholar]
- Plasma rich in growth factors reduces blue light-induced oxidative damage on retinal pigment epithelial cells and restores their homeostasis by modulating vascular endothelial growth factor and pigment epithelium-derived factor expression. Clin Exp Ophthalmol. 2020;48:830-8.
- [Google Scholar]
- Combined therapy with endoret-gel and plasma rich in growth factors vs endoret-gel alone in the management of facial rejuvenation: A comparative study. J Cosmet Dermatol. 2020;19:2616-26.
- [Google Scholar]
- High-throughput proteomic characterization of plasma rich in growth factors (PRGF-Endoret)-derived fibrin clot interactome. J Tissue Eng Regen Med. 2015;9:E1-12.
- [Google Scholar]
- Anti-inflammatory effect of different PRGF formulations on cutaneous surface. J Tissue Viability. 2021;30:183-9.
- [Google Scholar]
- Antibacterial effect of plasma rich in growth factors (PRGF®-Endoret®) against staphylococcus aureus and staphylococcus epidermidis strains. Clin Exp Dermatol. 2012;37:652-7.
- [Google Scholar]






