Translate this page into:
Comparative Evaluation of Therapeutic Efficacy and Safety of Microneedling Alone Versus Microneedling with Hyaluronic Acid in Post-Acne Scarring
Address for correspondence: Dr. Rubeena Bano, SR, Department of Skin and VD, Guru Gobind Singh Medical College and Hospital, Sadiq Road, Faridkot 151203, Punjab, India. E-mail: rubeena.bano20@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Facial acne scars are perceived negatively by society; in an era where everyone wants to look their best, acne and its sequelae are a great source of stress driving down self-worth and elevating the risk of depression and anxiety. It affects over 95% of acne patients, particularly in nodulocystic, conglobate, and fulminans varieties. Various treatment modalities are available, but no single modality is 100% curative. Microneedling produces controlled skin injury, releasing various growth factors and setting up a healing cascade, and laying down collagen as a result. Hyaluronic acid plays an important role in wound healing by creating physiological conditions in the extracellular matrix for the proliferation, migration, and organization of dermal cells.
Aims and Objectives:
To compare the therapeutic efficacy and safety of microneedling alone and microneedling with hyaluronic acid in acne scars.
Materials and Methods:
Sixty patients of age 18–40 years with clinically diagnosed acne scars were recruited and randomly divided into two groups of 30 each. Three sittings were done at an interval of 3 weeks of microneedling alone to Group A and microneedling with hyaluronic acid to Group B and followed up with two visits 4 weeks apart. Scoring was done with Goodman Quantitative Global Scarring Grade System. Side effects, patient satisfaction score, and pre and postprocedure Dermatological Life Quality Index (DLQI) were also recorded.
Results:
The female:male ratio was 3:2, mean age was 26.90 ± 4.90 years in Group A and 24.43 ± 5.39 years in Group B. Overall, 60% patients had a duration of 2–5 years, and unmarried patients outnumbered married ones in both groups. The combination morphology of the scars was the most common finding. In Group A mean Goodman Quantitative Global Scarring Grade System score reduced from baseline 24.13 ± 7.96 to 16.3 ± 7.2, and in Group B, from 27.73 ± 7.86 to 18.20 ± 7.12 at 17 weeks, this decrease was gradual and statistically significant. The patient satisfaction score for Group B (6.20 ± 1.45) was only slightly higher than that of Group A (5.73 ± 1.31). DLQI for Group A decreased from 7.77 to 4.10 and in Group B from 7.63 to 5.00. Both procedures were safe, with over 80% patients experiencing no side effects.
Conclusion:
The majority of patients showed “moderate” improvement in both groups; however, more patients in microneedling with hyaluronic acid group showed “good” and “very good” results at the end of the treatment completion. These are easy, office-based procedures not requiring training or any high-end machine, especially useful in resource-limited setups; the use of hyaluronic acid can enhance the efficacy of microneedling alone.
Keywords
Acne scars
microneedling
microneedling with hyaluronic acid
INTRODUCTION
Acne scars are one of the most common problems of adolescents. Facial acne scars are perceived negatively by society,[1] confirming the importance of preventing acne scars with early treatment of inflammatory acne and also justifying the use of invasive modalities for its treatment. Acne can lower self-esteem and cause troubles in forming interpersonal relationships at the workplace and other social platforms.[2] A synergistic combination of modalities is expected to have a better outcome, as no single modality is 100% curative for all scars alike. Therefore, for optimal results, we need to tailor the treatment accordingly depending upon the morphological type and depth of the scar, patients’ preferences, physicians’ preferences, and the available options. Various modalities are available, including topicals (retinoids), punch techniques, subcision, microdermabrasion, lasers, fillers, microneedling, and platelet-rich plasma.[34]
Microneedling creates micropunctures using fine needles to produce a controlled skin injury without actually damaging the epidermis. These microinjuries lead to minimal superficial bleeding and set up a wound healing cascade with the release of various growth factors such as platelet-derived growth factor, transforming growth factor (TGF-α and TGF-β), connective tissue activating protein, connective tissue growth factor, and fibroblast growth factor. The needles also breakdown the old hardened scar strands and allow it to revascularize.[5] Hyaluronic acid (HA) is a normal constituent of connective tissue and has been conventionally used as a filler; it has shown its effect in accelerating tissue repair and wound healing. It, therefore, holds a role in the treatment of acne scars by its rheological, viscoelastic, and hygroscopic properties, which are relevant for dermal tissue function. During tissue trauma or following infection, hyaluronan accumulates and stimulates immune cells at the injury site to express inflammatory mediators; higher levels were also found in newly formed granulation tissue.[6] There is the paucity of studies exploring the potential of simpler techniques such as microneedling and the role of hyaluronic acid as an adjunct with microneedling in post-acne scars; our study is an attempt to address the same.
MATERIALS AND METHODS
Patients of age 18–40 years with clinically diagnosed atrophic acne scars were enrolled, and after applying inclusion and exclusion criteria, sixty patients were selected using a convenient sampling technique. They were then randomly divided into two groups, A and B, of thirty each using a random number table. The study duration was one year between November 2019 and October 2020.
Exclusion criteria included active acne, keloidal tendency, bleeding disorder, and active skin infection like warts, herpes, and bacterial infection. The study was not blinded.
Procedure after gentle cleansing with normal saline, topical anesthetic cream (Eutectic mixture of local anesthetic, EMLA) was applied over the area to be treated and left for 60 min. After cleaning the area, microneedling with a hand-held motorized microneedling device was done over the affected area with a 1.5–2-mm needle depth using the stamping technique in Group A. In Group B, a uniform thin layer of 1% HA (noncross-linked sodium hyaluronate with molecular weight 9500–730–9500 kD, requiring around 0.5–1.0 mL) was applied over the affected area, and microneedling was done similar to Group A [Figure 1]. Three sittings were done at an interval of 3 weeks, followed by two follow-up visits 4 weeks apart. Grading was done with Global Scarring Grade System (GSGS),[7] and photographically, posttreatment improvement was calculated based on a reduction in GSGS scores from baseline such that a reduction of 0–5 was minimal, 6–10 was moderate, 11–15 was good, and >15 was labeled as a very good response. Side effects were recorded on every visit, DLQI (Dermatological Life Quality Index) was calculated pre and postprocedure, and patient satisfaction was recorded between 1 (the worst possible) and 10 (the best possible) upon treatment completion.[8]

- Showing (a) EMLA application for 60 min (b) microneedling using stamping technique and (c) pinpoint bleeding- End point
RESULTS
Data were collected and analyzed using IBM SPSS® v 20.0, Chicago, IL. The descriptive statistics for categorical variables were represented in the form of frequencies, percentages, and as mean and standard deviations for continuous variables. The association between categorical variables was explored using Pearson’s Chi-square test wherever appropriate. The difference of continuous variables between two points in one group was explored using paired samples t-test or Wilcoxon signed–rank test while the difference across two groups was analyzed using independent samples t-test or Mann–Whitney U test, P value of 0.05 or less was considered for statistical significance.
Females outnumbered males in a 3:2 ratio; the mean age was 26.90 ± 4.90 years in Group A and 24.43 ± 5.39 years in Group B. The mean duration of scars in our study was 2–5 years, and the majority were self-employed in family business. Mixed type of acne scar was seen at a greater frequency than individual types. A combination of rolling and icepick scars was found to be the most common type (18.33%), followed by icepick and boxcar scars (16.66%) and icepick, rolling, and boxcar scars (16.66%) [Table 1].
| Demographics | Procedure | Total | P-value | ||||
|---|---|---|---|---|---|---|---|
| Group A | Group B | ||||||
| SEX | Male | 11 | 37% | 13 | 43% | 24 | 0.598 |
| Female | 19 | 63% | 17 | 57% | 36 | ||
| DURATION | <1 year | 3 | 10% | 9 | 30% | 12 | 0.065 |
| 1-2 year | 7 | 23% | 11 | 37% | 18 | ||
| 2-5 year | 18 | 60% | 9 | 30% | 27 | ||
| >5 year | 2 | 7% | 1 | 3% | 3 | ||
| MARITAL | Unmarried | 21 | 70% | 22 | 73% | 43 | 0.774 |
| Married | 9 | 30% | 8 | 27% | 17 | ||
| PROFESSION | Business | 9 | 30% | 8 | 27% | 17 | 0.960 |
| Service | 7 | 23% | 8 | 27% | 15 | ||
| Housewife | 4 | 13% | 6 | 20% | 10 | ||
| Farmer | 3 | 10% | 3 | 10% | 6 | ||
| Student | 5 | 17% | 3 | 10% | 8 | ||
| Others | 2 | 7% | 2 | 7% | 4 | ||
| RESIDENCE | Rural | 19 | 63% | 19 | 63% | 38 | 1.000 |
| Urban | 11 | 37% | 11 | 37% | 22 | ||
| PREDOMINANT SCAR MORPHOLOGY | Icepick | 2 | 7% | 1 | 3% | 3 | 0.925 |
| Rolling | 3 | 10% | 5 | 17% | 8 | ||
| Boxcar | 5 | 17% | 4 | 13% | 9 | ||
| Rolling+icepick | 6 | 20% | 5 | 17% | 11 | ||
| Icepick+boxcar | 4 | 13% | 6 | 20% | 10 | ||
| Rolling+boxcar | 4 | 13% | 5 | 17% | 9 | ||
| Icepick+Rolling+Boxcar | 6 | 20% | 4 | 13% | 10 | ||
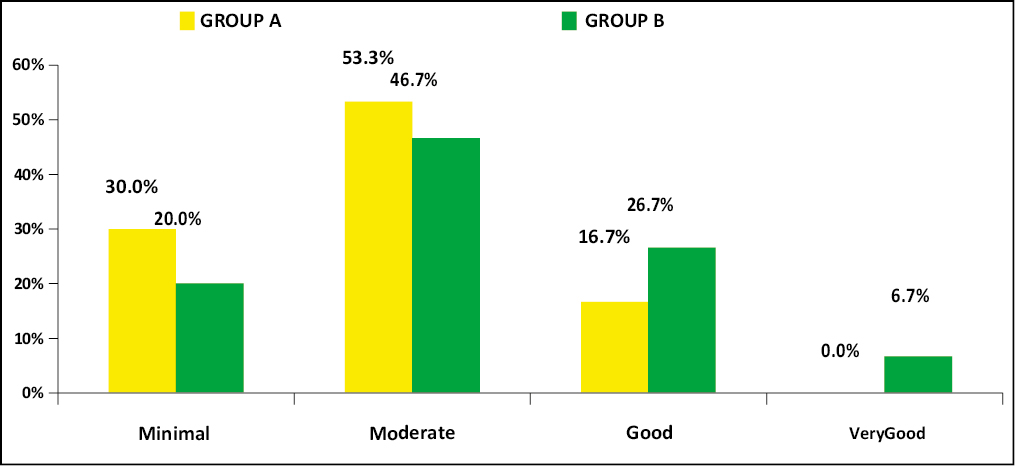
In Group A, mean acne score reduced from 24.13 ± 7.96 (baseline) to 16.3 ± 7.2 (17 weeks), while in Group B, it reduced from 27.73 ± 7.86 (baseline) to 16.9 ± 7.72 (17 weeks) [Table 2]. Maximum patients of both groups showed “moderate” to “minimal” improvement; however, the proportion of patients showing good and very good improvement was more in Group B [Table 3].
| GSGS scores | Group A | Group B | p-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Baseline | 24.13 | 7.96 | 27.73 | 7.86 | 0.083 |
| 3wk | 22.50 | 7.90 | 27.30 | 7.43 | 0.018 |
| 6wk | 20.87 | 7.38 | 25.10 | 7.26 | 0.029 |
| 9wk | 18.83 | 7.02 | 22.50 | 7.26 | 0.051 |
| 13 Wk | 17.30 | 7.05 | 20.83 | 7.01 | 0.056 |
| 17 Wk | 16.30 | 7.20 | 18.20 | 7.12 | 0.030 |
 |
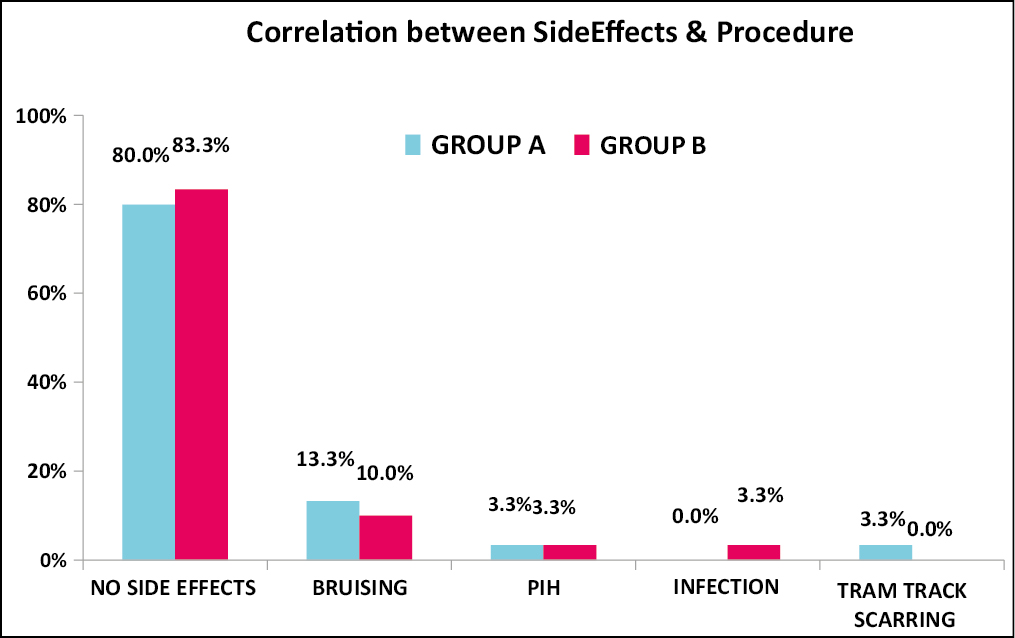
The correlation of response to therapy with scar morphology and duration is shown in Table 4. In terms of secondary effects, our patients reported a decrease in oiliness and an overall improved texture of the skin. Overall, there were no side effects in the majority of our patients in either arm.
| Group A | Icepick scar | Rolling scar | Boxcar scar | Rolling and Icepick scar | Icepick and Boxcar scar | Rolling and Boxcar scar | Icepick, Rolling and Boxcar scar |
|---|---|---|---|---|---|---|---|
| Response | |||||||
| Minimal | 2 | 0 | 0 | 2 | 3 | 0 | 2 |
| Moderate | 0 | 2 | 5 | 4 | 1 | 2 | 2 |
| Good | 0 | 1 | 0 | 0 | 0 | 2 | 2 |
| Very Good | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Group B | Icepick scar | Rolling scar | Boxcar scar | Rolling and Icepick scar | Icepick and Boxcar scar | Rolling and Boxcar scar | Icepick, Rolling and Boxcar scar |
| Response | |||||||
| Minimal | 1 | 0 | 1 | 4 | 0 | 0 | 0 |
| Moderate | 0 | 5 | 3 | 1 | 3 | 0 | 2 |
| Good | 0 | 0 | 0 | 0 | 3 | 3 | 2 |
| Very Good | 0 | 0 | 0 | 0 | 0 | 2 | 0 |
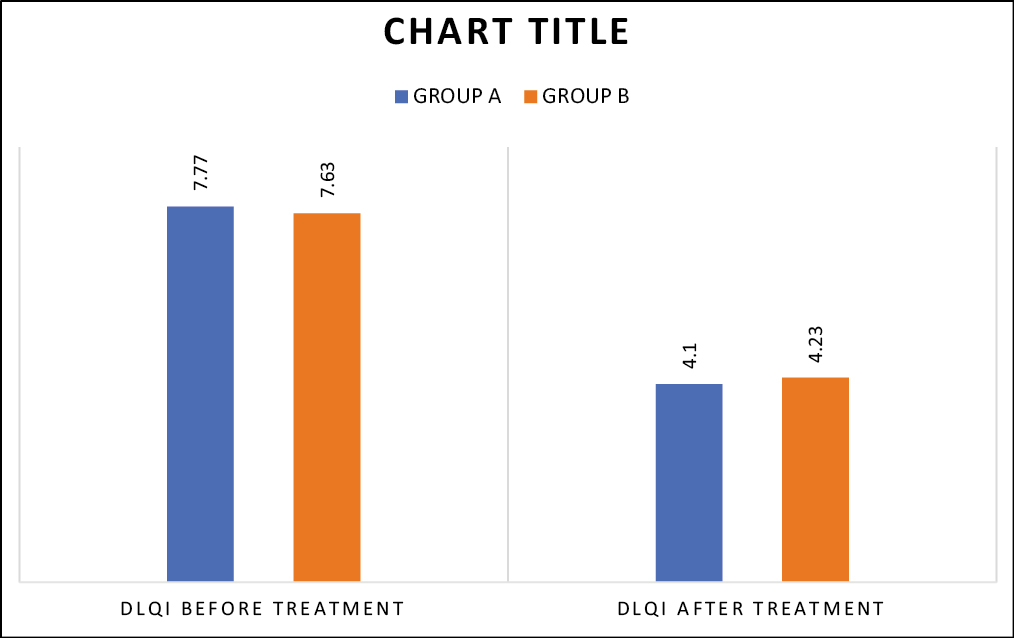
Temporary bruising was the most common side effect observed, which resolved spontaneously. Postinflammatory hyperpigmentation, infection, and tram track scarring were rare and were observed in 3.3% patients each [Table 5]. There was no statistically significant difference between two groups in terms of side effects (P = 0.706). Mean patient satisfaction score in Group A was 5.73 ± 1.31 and in Group B was 6.20 ± 1.45 with P = 0.196 [Table 6]. DLQI in Group A decreased from 7.77 ± 2.13 to 4.10 ± 1.63, and in Group B, it decreased from 7.63 ± 2.11 to 5 ± 1.34 (P = 0.023) [Table 7].
 |
| Scar morphology | Procedure | N | Mean Patient satisfaction score | SD | p value |
|---|---|---|---|---|---|
| Ice Pick Scar | GROUP A | 2 | 3 | 1.414 | 0.212 |
| GROUP B | 1 | 8 | 0 | ||
| Rolling Scar | GROUP A | 3 | 6.67 | 1.528 | 0.074 |
| GROUP B | 5 | 5 | 0.707 | ||
| Boxcar Scar | GROUP A | 5 | 5.4 | 1.14 | 0.675 |
| GROUP B | 4 | 5.75 | 1.258 | ||
| Rolling And Icepick Scar | GROUP A | 6 | 6.33 | 0.816 | 0.550 |
| GROUP B | 5 | 5.8 | 1.924 | ||
| Icepick & Boxcar Scars | GROUP A | 4 | 5 | 0.816 | 0.081 |
| GROUP B | 6 | 6.67 | 1.506 | ||
| Rolling & Boxcar Scars | GROUP A | 4 | 6.75 | 1.258 | 0.951 |
| GROUP B | 5 | 6.8 | 1.095 | ||
| Icepick, Rolling And Boxcar Scars | GROUP A | 6 | 5.67 | 0.516 | 0.247 |
| GROUP B | 4 | 6.75 | 1.5 |
 |
DISCUSSION
Acne scars are broadly classified into atrophic and hypertrophic based on whether there is net loss or gain of collagen. Scarring has profound effects on the psyche of the sufferer, i.e., these are scars on soul rather than just on skin. The aim of all treatment modalities is to aid the natural dynamic process of wound healing to reform skin surface irregularity and hence aesthetic function. Currently, there are no large high-quality studies evaluating the efficacy of different modalities. Often the patient’s scar severity perception is greater than the severity assessment done by the dermatologist. Atrophic post-acne scars are further subclassified as ice-pick or V-shaped scars (60%–70%), rolling or W-shaped scars (15%–25%), and boxcar or U-shaped scars (20%–30%).[3] Management of acne scars depends upon scar type, patient’s preferences, physician’s experience, available options, and pocket of the patient. Although scarring is more common in males, but in our study, females outnumbered males; similarly, unmarried patients outnumbered married patients, explained by greater concern for their looks. Mean age was 26.90 ± 4.90 years and 24.43 ± 5.39 years, respectively, in Groups A and B. Similar observations were noted by Alsaedy et al.[9] and others, including Porwal et al.,[10] Dogra et al.[11] etc. The majority of patients had mixed types of acne scars; similar findings were also observed by Alsaedy et al.,[9] whereas contrasting observations were present in studies conducted on atrophic acne scar patients by Amer et al.[12] and Dogra et al.,[11] who observed a higher prevalence of boxcar scars and rolling scars, respectively. The difference in the pattern of acne scarring is due to differences in ethnicity, genetic makeup, environmental exposures, and early treatment of inflammatory acne. Mean grading of scars showed a significant reduction after the treatment of the patients in both the groups, as shown in Figure 2,Figure 3,Figure 4,Figure 5, but statistically significant and better results were observed in the patients who were treated with microneedling with HA versus those treated with microneedling alone. At the end of 17 weeks, there was an improvement of 32.45% in the microneedling group versus a 39.06% improvement in microneedling with HA group (P = 0.029, statistically significant). The improvement in acne scars (shown by the rate of fall of GSGS score) showed gradually increasing trend throughout the study duration in both groups. A similar study on acne scars using microneedling with HA was done by Amer et al.[12] This study reported an improvement of 82.9% at the end of 16 weeks in contrast to 39.06% at the end of 17 weeks observed in our study, probably due to the higher concentration of HA used by them. Another explanation is the different morphology of scars as well as the grading system (Goodman and Baron Qualitative score). Another study by Alsaedy et al.[9] used Dermatologists’ Assessment of Level of Improvement, their study concluded that the addition of hyaluronic acid provided faster recovery time and fewer side effects; this finding was also observed in our study in the form of decreased healing time and reduced bruising in Group B patients. HA promotes the migration and maturation of keratinocytes in the process of re-epithelialization and has been proposed as a possible marker for effective healing in soft tissues. The grade of improvement majority of patients was “moderate” in both groups; however, more patients in microneedling with HA group showed “good” and “very good” results at the end of the treatment completion, whereas none of the patients in Group A showed very good response. In terms of scar morphology, icepick scar showed the least improvement compared to other types highlighting the need of other therapies in combination or alone (like subcision and TCA CROSS) for better outcomes. As per the findings of our study, both procedures were found to be safe with minimal side effects. A maximum number of patients (81.67%) presented with no side effects after the procedure completion. Only a few of the patients complained of bruising, post inflammatory hyperpigmentation, and tram track scarring after the procedure, lesser with microneedling with HA group. DLQI reduction in Group A was more as compared to Group B probably because patients have unrealistic expectations, and the level of improvement as assessed objectively can differ from patients’ subjective assessment as indicated by the reduction in GSGS scores.
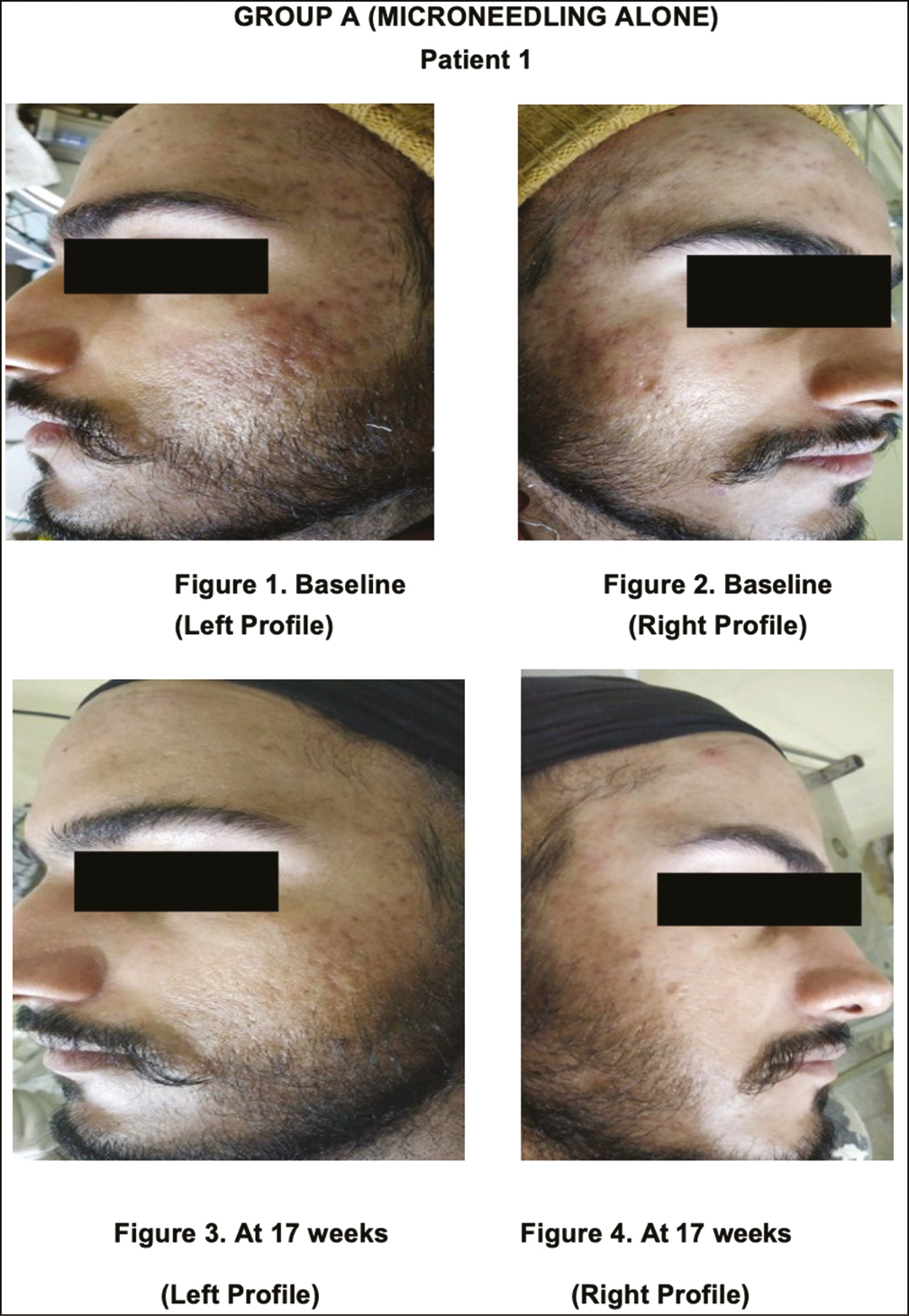
- Group A, before and after photographs, (Patient 1)
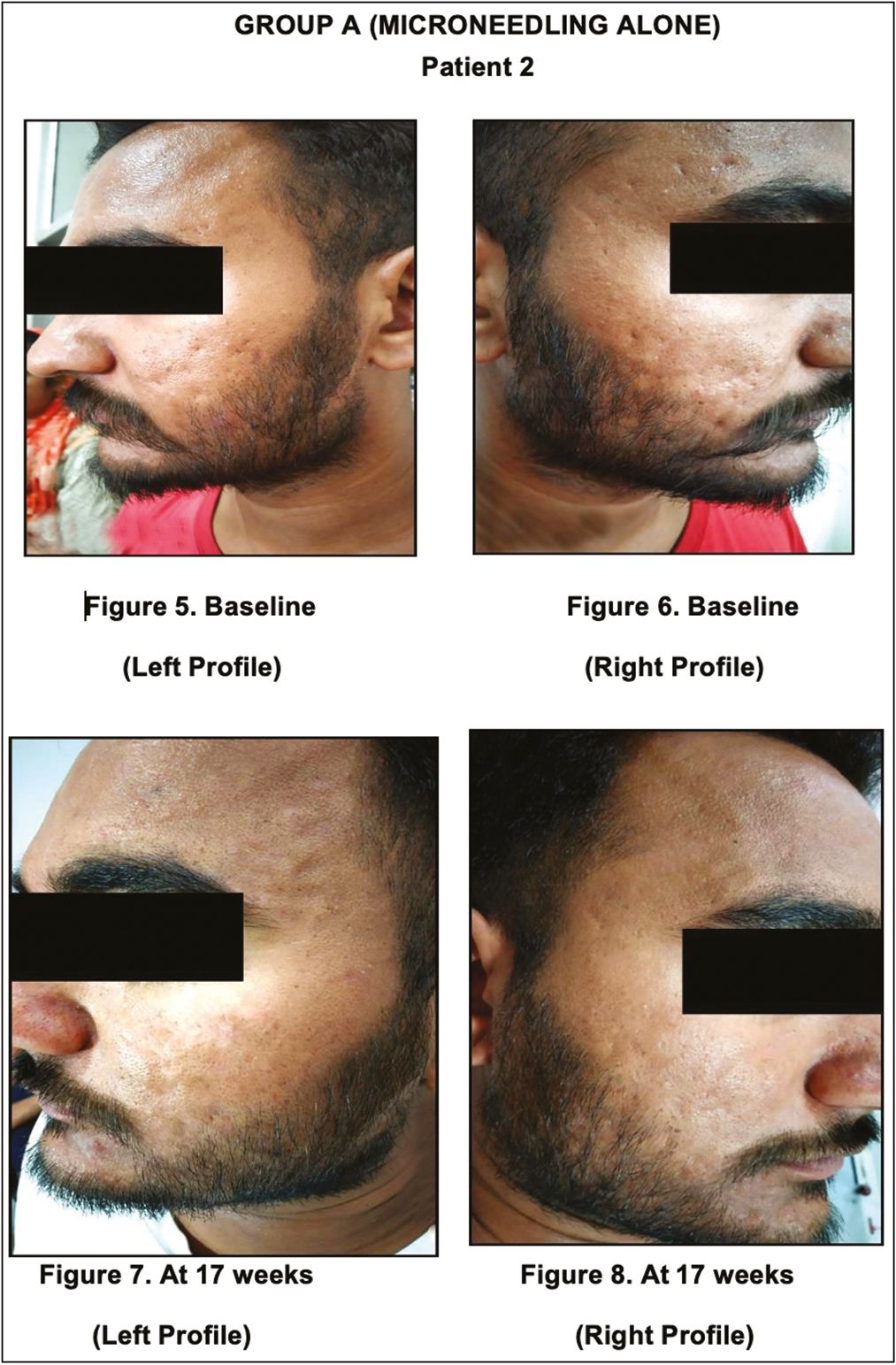
- Group A, before and after photographs, (Patient 2)
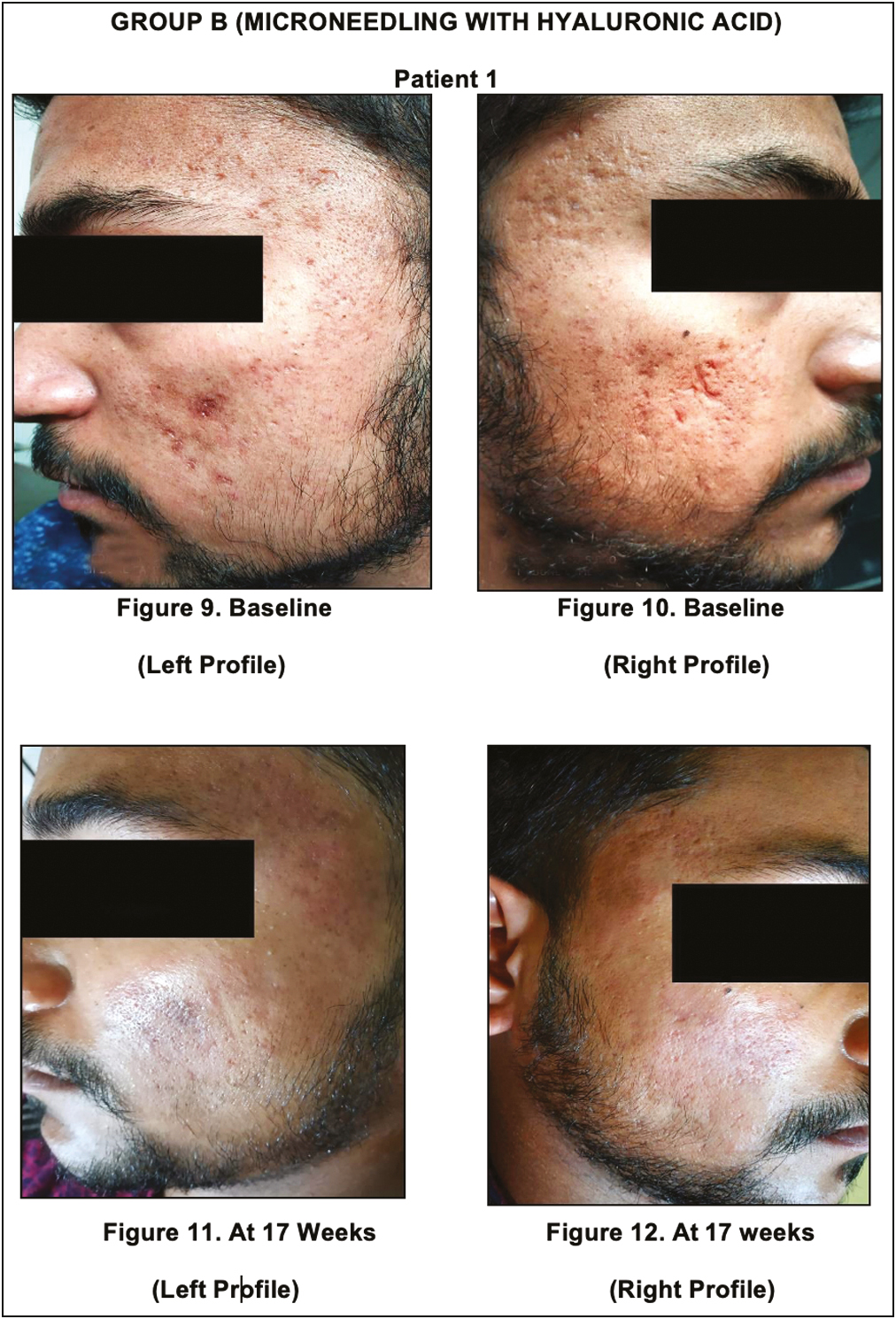
- Group B, before and after photographs, (Patient 1)

- Group B, before and after photographs, (Patient 2)
CONCLUSION
The use of hand-held motorized microneedling devices in our study with adjustable needle depth allowed addressing acne scars in difficult-to-reach areas and areas with thin skin like periorbital region, nose, and forehead without much damage. Microneedling can be combined with other methods since the synergistic combination of modalities is expected to have a better outcome. In conclusion, needling with HA is easy to perform and provides satisfactory results; however, we propose more sittings for better clinical outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- How people with facial acne scars are perceived in society: An online survey. Dermatol Ther. 2016;6:207-18.
- [Google Scholar]
- The association between stress and acne among female medical students in Jeddah, Saudi Arabia. Clin Cosmet Investig Dermatol. 2017;10:503-6.
- [Google Scholar]
- Acne scarring: A classification system and review of treatment options. J Am Acad Dermatol. 2001;45:109-17.
- [Google Scholar]
- Standard guidelines of care for acne surgery. Indian J Dermatol Venereol Leprol. 2008;74:28.
- [Google Scholar]
- Microneedling therapy for atrophic acne scars: An objective evaluation. J Clin Aesthet Dermatol. 2015;8:36-42.
- [Google Scholar]
- Expression of proteoglycans and hyaluronan during wound healing. J Histochem Cytochem. 1995;43:125-35.
- [Google Scholar]
- Postacne scarring: A quantitative global scarring grading system. J Cosmet Dermatol. 2006;5:48-52.
- [Google Scholar]
- Dermatology life quality index (DLQI)—A simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-6.
- [Google Scholar]
- The efficacy of topical hyaluronic acid serum in acne scar patients treated with fractional CO2 laser. Am J Dermatol Venereol. 2017;6:17-24.
- [Google Scholar]
- A comparative study of combined dermaroller and platelet-rich plasma versus dermaroller alone in acne scars and assessment of quality of life before and after treatment. Indian J Dermatol. 2018;63:403-8.
- [Google Scholar]
- Microneedling for acne scars in Asian skin type: An effective low cost treatment modality. J Cosmet Dermatol. 2014;13:180-7.
- [Google Scholar]
- Combined autologous platelet-rich plasma with microneedling versus microneedling with non-cross-linked hyaluronic acid in the treatment of atrophic acne scars: Split-face study. Dermatol Ther. 2020;27:e14457.
- [Google Scholar]






