Translate this page into:
Comparative study in treatment of acne scars fractional carbon dioxide laser versus micro needling fractional radio frequency – A retrospective study
*Corresponding author: Rashmi Sriram, Department of Dermatology, Venereology, Leprosy, Balagangadhara Swamiji Global Institute of Medical Sciences, Bengaluru, Karnataka, India. kirannsriram@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sriram R, Chandrashekar BS, C M, Gowda HH. Comparative study in treatment of acne scars fractional carbon dioxide laser versus micro needling fractional radio frequency – A retrospective study. J Cutan Aesthet Surg. 2024;17:214-8. doi: 10.25259/jcas_122_23
Abstract
Objectives:
Efficacy of fractional carbon dioxide laser and microfractional radiofrequency in treatment of acne scars is well substantiated. The objective of this study was to compare the efficacy and safety of carbon dioxide laser versus microfractional radiofrequency in treatment of acne scars in skin type 3,4.
Material and Methods:
Thirty-two patients of skin types 3–4 with grade 3 and 4 atrophic acne scars, of which 16 were treated with fractional carbon dioxide (CO2) laser and 16 were treated with microfractional radiofrequency were retrospectively analyzed. All patients received either treatment 4 sessions at an interval of 4–6 weeks. Objective assessment was done with qualitative and quantitative Goodman and baron acne scar grading system by assessment of photographs at baseline and 3 months after last session.
Results:
All the data collected were entered in a Microsoft Excel worksheet and analyzed using R Software R-4.2.1. The study variables acne scar grades were described using frequency with percentage, acne scar scores were described using Mean with Standard deviation, and Median with interquartile range (IQR) (Q1-Q3). Since the data were ordinal, which is non-normal, hence, non-parametric tests are applied. To compare grades between the groups, Mann–Whitney U-test was applied.
Conclusion:
There was no difference in the last session (after the treatment) between the groups, the Mann– Whitney U-test was 109.5 with P-value of 0.484 >0.05. Therefore, there was no statistically significant difference between the microfractional radiofrequency and carbon dioxide laser group. There were 2 (12.5%) cases reported with post-inflammatory hyperpigmentation in the CO2 laser group and zero cases in the microfractional radiofrequency group.
Keywords
Acne scars
Fractional CO2 laser
Microfractional radiofrequency
INTRODUCTION
A fractional laser resurfacing technique, based on the principle of fractional photothermolysis, causes microscopic treatment zones of complete epidermal ablation with variable amounts of dermal coagulation.1 It results in microscopic pattern with spatial separation of columns of thermally affected epidermal and dermal tissue. Unlike ablative lasers, it is not associated with extended post-operative recovery period, prolonged erythema, and worsening of the scars which hinder application of this technique in dark skinned individuals.2
Fractional bipolar radiofrequency technique based on creating radiofrequency thermal zones without epidermal injury can be used to induce natural neo collagen in skin. After damage to the reticular dermis, long-term dermal remodeling, neoelastogenesis and neocollagenesis results in dermal thickening. With this modality, only 5% of epidermis is affected compared to 10–70% with fractional ablative laser treatment.3
Although fractional carbon dioxide (CO2) laser and micro needling fractional radiofrequency have gained acceptance, studies comparing efficacy and side effects are lacking. This study has been done to compare efficacy and safety in treatment of acne scars using fractional CO2 laser and microneedling radiofrequency.
MATERIAL AND METHODS
A retrospective photographic analysis of 32 patients, of which 16 patients treated with fractional CO2 laser and 16 patients treated with microfractional radiofrequency of facial atrophic scars between November 2012 and December 2013 were done. None of the patients had received any treatment for acne scars. Patients were excluded if they had received other modalities of treatment for acne scars.
Patients had undergone either treatment for acne scars, four sessions with an interval of 4–6 weeks between each session. Treatment regimen was individualized based on predominant scar type, scar depth, and fibrosis of dermal tissue.
The treatment areas were cleansed of debris, including dirt, make up and powder, using mild cleanser and 70% isopropyl alcohol. Lidocaine 2.5% and prilocaine 2.5% cream were applied under occlusion to the treatment area. After an hour of application, the anesthetic cream was gently removed, and then alcohol was used to degrease the skin to obtain a completely dry skin surface. All subjects were treated by a single operator.
In microfractional radiofrequency (Infini-lutronic), high-energy settings, 25W–30W, respectively, were used at lower penetration depths to prevent epidermal coagulation, penetration depth limited to 1.5 mm on forehead, and temple areas with bony prominences. Patients with predominantly ice pick scars and mixed scarring were given a needle depth of 3.5 mm on first pass and 2.5 mm on the second pass and third pass with minimal or no overlapping.
In fractional CO2 laser (ECO2-Lutronic), full face was treated in rejuvenation mode with power of 20–30W, energy of 20– 30 mJ, 100 spots/cm2, scan size 18 × 18 with 300 tip single pass followed by 2 passes over atrophic scars with power of 60–80 W, energy of 20–30 mJ, 50 spots/cm2, and scan size of 8 × 8, with 120 tip.
Post-procedure ice compresses were given for 15–20 min, pain was managed by oral non-steroidal anti-inflammatory drugs. Patients were advised strict sun protection along with reepithelialization agents containing cyclopentasiloxane, cyclohexasiloxane, and sodium hyaluronate. Post CO2 laser, patients had downtime of 5 days unlike microfractional radiofrequency patients who could resume their work from next day.
A single non-treating physician assessor evaluated clinical response to treatment by goodman and baron acne scar grading system by assessment of photographs at baseline and 3 months after the last session. Digital photographs were obtained using identical camera settings and lightening conditions at each follow-up session.
Assessment of efficacy
Objective assessment of physician scores of improvement was determined by goodman and baron global acne grading system.
Statistical analysis
All the data collected were entered into a Microsoft Excel worksheet and analyzed using R Software R-4.2.1. The study variables acne scar grades were described using frequency with percentage, acne scar scores were described using mean with standard deviation, and median with interquartile range (IQR) (Q1-Q3).
Since the data were ordinal, which is non-normal; hence, non-parametric tests are applied. To compare grades between the groups, Mann–Whitney U-test is applied. To compare the pre-post-intervention, the Wilcoxon Signed-Ranks test is applied.
RESULTS
In Table 1, it shows that in the first session, the median score in the Infini group was 17 (13–26) IQR, and in the CO2 group was 21.5 (15.3–24), the Mann-Whitney U test was 111.5 with a P-value of 0.533>0.05, there is no statistically significant difference at a first session between the groups.
| First session | n | Min-Max | Mean±SD | Median (Q1-Q3) | Mann-Whitney U | P-value |
|---|---|---|---|---|---|---|
| Infini | 16 | 8-33 | 19.19±7.28 | 17 (13-26) | 111.5 | 0.533 |
| CO2 Last Session |
16 | 12-38 | 21.31±7.38 | 21.5 (15.3-24) | ||
| Infini | 16 | 6-22 | 12.56±5.06 | 11 (8-17.5) | 109.5 | 0.484 |
| CO2 | 16 | 7-34 | 14.88±7.68 | 12.5 (9.3-18.8) | ||
| At | Paired difference (Before-After) | Wilcoxon signed ranks test | P-value | |||
| First session to last session | n | Min-Max | Mean±SD | Median (Q1-Q3) | ||
| Infini | 16 | 1-17 | 6.63±4.06 | 5.5 (4.3-8) | -3.529 | 0.00041 |
| CO2 | 16 | 2-16 | 6.44±4.59 | 4.5 (3-8.5) | -3.523 | 0.00042 |
Q: Quartile, SD: Standard deviation, CO2: Carbon dioxide
Similarly, there was no statistically significant difference in the last session (after the treatment) between the groups, the Mann–Whitney U-test was 109.5 with P-value of 0.484 > 0.05. Therefore, there is no statistically significant difference in the first session and last session between the Infini and CO2 groups.
To compare the improvement from the first session to the last session among the groups assessed, the Infini group had the median difference score with IQR of 5.5 (4.3–8), with Wilcoxon Signed-Rank test −3.529 and P-value of 0.00041 < 0.05. Therefore, there is a statistically significant difference from the first session to the last session in the Infini group.
Similarly, in the CO2 group, the median difference score with IQR was 4.5 (3–8.5), with Wilcoxon Signed-Rank test −3.523 and P-value of 0.00042 < 0.05. Therefore, there is a statistically significant difference from the first session to the last session in the CO2 group.
Therefore, there is an overall improvement in both Infini and CO2 groups.
In this study, from Table 2, 16 patients participated in each group. Most patients had mixed types of atrophic acne scars including ice pick, box scar, and rolling scars. Estimation of improvement with Goodman and baron qualitative acne scarring system was done.
| Infini | Grades after | Total | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Grades before | ||||
| 2 | 2 (100%) | - | - | 2 (12.5%) |
| 3 | 4 (66.7%) | 2 (33.3%) | - | 6 (37.5%) |
| 4 | - | 8 (100%) | - | 8 (50%) |
| Total | 6 (37.5%) | 10 (62.5%) | - | 16 |
| CO2 | Grades after | |||
| 1 | 2 | 3 | Total | |
| Grades before | ||||
| 2 | 2 (100%) | - | - | 2 (12.5%) |
| 3 | 5 (62.5%) | 3 (37.5%) | - | 8 (50%) |
| 4 | - | 5 (83.3%) | 1 (16.7%) | 6 (37.5%) |
| Total | 7 (43.7%) | 8 (50%) | 1 (6.3%) | 16 |
CO2: carbon dioxide
Out of the 16 patients who underwent microfractional radiofrequency, 8 (50%) patients had a grade of 4 before the treatment, and all 8 had improved and reduced to grade 2. 6(37.5%) patients had a grade of 3 before, and 4 (66.7%) reduced to grade 1 [Figure 1a and b] and 2 (33.3%) reduced to grade 2. Two (12.5%) patients had grade 2 before the treatment and all two were reduced to grade 1. Rolling scars and box scars showed better improvement than ice-pick scars.
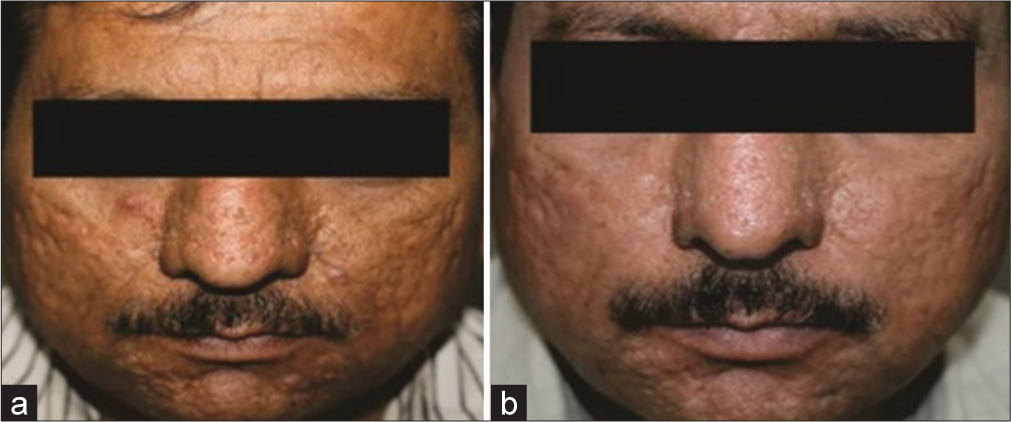
- (a) Grade 3 acne scars before microfractional radiofrequency. (b) Improvement to grade 1 post-microfractional radiofrequency.
Out of the 16 patients who underwent CO2 laser, 6 (37.5%) patients had a grade of 4 before the treatment, 5 (83.3%) had improved and reduced to grade 2 [Figure 2a and b], and 1 (16.7%) had reduced to grade 3. Eight (50%) patients had a grade of 3 at before, and 5 (62.5%) reduced to grade 1 and 3 (37.5%) reduced to grade 2. Two (12.5%) patients had a grade of 2 before the treatment and all two were reduced to grade 1. There were 2 (12.5%) cases reported with post-inflammatory hyperpigmentation in the CO2 group and zero cases in the Infini group.

- (a) Grade 4 acne scars before carbon dioxide (CO2) laser. (b) Improvement to grade 2 post CO2 laser.
As shown in Table 1, the Mann–Whitney U-test was 109.5 with P-value of 0.484 > 0.05.
Therefore, there is no statistically significant difference in the first session and last session between the Infini and CO2 groups.
DISCUSSION
Acne scarring is known to impart a heavy psychosocial burden on patients and it is of utmost importance to treat them. There are a wide range of ablative, fractional ablative, fractional non-ablative lasers, radiofrequency microneedling, and combination therapies to treat acne scars.
CO2 laser resurfacing has been used for more than 20 years. Newer versions of CO2 utilize fractionated laser beams rather than non-fractionated devices. Fractional laser resurfacing has been proven effective for treatment of acne scars.4 It basically utilizes light-based energy to destroy columns of skin which stimulates production of new collagen fibers, elastic fibers, and epidermis.5 However, this treatment has been associated with adverse events such as persistent erythema, scarring, infection, and pigmentary changes.
Non-ablative fractional lasers are useful for patients with superficial acne scars or those who do not have the time for a fully ablative procedure. They do not vaporize the skin, instead they heat and stimulate reparative mechanisms to remodel which results in faster healing. However, there was higher incidence of hyperpigmentation.6
You et al. have compared ablative fractional CO2 with ablative CO2 (non-fractionated), Er Yttrium Aluminium Garnet (Er YAG), and fractional erbium 1550 nm. The data suggest that ablative fractionated laser was as effective as non-fractionated laser with less erythema. However, non-ablative lasers had significantly less improvement. Based on this study, it seems reasonable to utilize ablative fractional resurfacing as primary mode of treatment in moderate to severe acne scars.7
Microneedling radiofrequency has the advantage of avoiding hyperpigmentation unlike fractional ablative and non-ablative lasers especially in darker skin types. It creates thermal zones of injury without targeting the epidermis. It involves use of insulated microneedles which produce electrothermal damage only at tip and produces collagen through release of growth factors.8
Qian et al. have done study in treatment of acne scars with fractional CO2 laser (Active Fx-Lumenis). In this study, 31 patients received three sequential treatment were given over 6 months, and evaluation was done at 3 and 12 months after final treatment. About 12.9% patients showed excellent improvement in acne scars, while 38.71% noted good to fair results. Four patients had transient post-inflammatory hyperpigmentation and three were noted to have prolonged erythema. However, in our study, only two had post-inflammatory hyperpigmentation as adverse effect.9
Gold and Biron have conducted clinical trials in treatment of acne scars using bipolar radiofrequency (matrix-radiofrequency [RF]). Fifteen subjects with mild-to-moderate acne scars received three monthly treatments and noticed significant improvement in acne scars, fine lines, and wrinkles. Adverse effects were limited to transient erythema, stinging. However, in our study, no adverse effects were reported and patients tolerated a procedure well.10 Ramesh et al. treated facial acne scars of 30 subjects (skin types IV-VI) with a matrix tunable radiofrequency device that was safe in skin types IV to VI. To conclude bipolar radiofrequency, RF technology is safe in all skin types as proven by all studies including current study.11 From the available literature search, there are two studies comparing the efficacy and safety of microfractional radiofrequency and CO2 laser.
In our study, both microfractional radiofrequency and CO2 laser were equally effective in treatment of atrophic acne scars consistent with study by Zhang et al.12 Rajput et al.13 too post-inflammatory hyperpigmentation, however, was reported with CO2 laser which makes fractional radiofrequency as better choice in skin type IV-VI.
The advantage of CO2 laser was that it was effective in popular scars over the nose and this area could not be treated with microfractional radiofrequency.
The limitation of this study was that we have done retrospective study, limited sample size, and no histological evaluation was done.
CONCLUSION
Fractional microneedling radiofrequency and fractional CO2 laser are equally effective for treatment of atrophic acne scars. However, fractional radiofrequency has less down time and Post Inflammatory Hyperpigmentation (PIH), making it an efficient and safer treatment option in darker skin types.
Authors’ contributions
All the authors, Rashmi Sriram, B S Chandrashekhar, Madura C and Harshvardhan Gowda have contributed to the research study. They have contributed in the collection of data, consent, design, statistics, analysis and review of study.
Ethical approval
Institutional Review Board approval is not required because the study is a retrospective study.
Declaration of patients consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Fractional photothermolysis: A new concept of cutaneous remodelling using microscopic patterns of thermal injury. Laser Surg Med. 2004;34:426-38.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional photothermolysis for the treatment of acne scars: A report of 27 Korean patients. J Dermatolog Treat. 2008;19:45-9.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the effect of fractional laser with radiofrequency and fractionated radiofrequency on the improvement of acne scars. Dermatol Surg. 2011;37:1260-7.
- [CrossRef] [PubMed] [Google Scholar]
- Review of fractional photothermolysis: Treatment indications and efficacy. Dermatol Surg. 2009;35:1445-61.
- [CrossRef] [PubMed] [Google Scholar]
- Skin responses to fractional thermolysis. Lasers Surg Med. 2006;38:142-9.
- [CrossRef] [PubMed] [Google Scholar]
- Non ablative fractional laser resurfacing for acne scarring in patients with Fitzpatrick skin phototypes IVVI. Dermatol Surg. 2016;42:392-402.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of four different lasers for acne scars: Resurfacing and fractional lasers. J Plast Reconstr Aesthet Surg. 2016;69:e87-95.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of microneedling radiofrequency for treatment of scars. J Cutan Aesthet Surg. 2014;7:93-7.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of acne scarring with fractional CO2 laser. J Cosmet Laser Ther. 2012;14:162-5.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of acne scars by fractional radiofrequency energy. J Cosmet Laser Ther. 2012;14:172-8.
- [CrossRef] [PubMed] [Google Scholar]
- A novel technology in treatment of acne scars: The matrix tunable radiofrequency technology. J Cutan Aesthet Surg. 2010;3:97-101.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of fractional microplasma radiofrequency technology and carbon dioxide fractional laser for treatment of atropic acne scars: A randomised split face clinical study. Dermatol Surg. 2013;39:559-6.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective, nonrandomized open label study, comparing the efficacy, safety, and tolerability of fractional CO2 laser versus fractional microneedling radiofrequency in Acne scars. J Cutan Aesthet Surg. 2021;14:177-83.
- [CrossRef] [PubMed] [Google Scholar]







