Translate this page into:
Comparison of Intralesional Measles, Mumps, Rubella Vaccine and Needling in the Treatment of Recurrent Warts
Address for correspondence: Dr. Vidyadhar R. Sardesai, 102 Alliance Nakshatra, 48 Tulshibagwale Colony, Sahakarnagar 2, Pune 411009, Maharashtra, India. E-mail: nitin_sardesai@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Context:
Warts constitute 21% of all the cases in a dermatology clinic. Their causative agent is the human papillomavirus (HPV). Most of the cutaneous warts are cosmetically disfiguring and their treatment requires patience by both the practitioner and the patients.
Aim:
This study aimed to compare the efficacy of intralesional measles, mumps, rubella (MMR) vaccine and needling in the treatment of recurrent warts.
Settings and Design:
This was a prospective, comparative, and interventional study.
Subjects and Methods:
This hospital-based study was conducted in a tertiary health-care center from September 2017 to August 2019. Overall 40 patients of recurrent warts were included in the study.
Statistical Analysis:
Fisher test, Student t test, and chi-square test were used for statistical analysis.
Results:
Improvement was noted in patients belonging to both the groups. However, after applying chi-square test, it was found that results were statistically significant in the needling group only. When both the groups were compared using chi-square test, needling showed statistically significant results after 4 and 6 weeks.
Conclusion:
Needling was observed to be a better treatment modality as compared to intralesional MMR vaccine at the end of 4 and 6 weeks. More number of sessions were required in the intralesional MMR vaccine group for complete clearance of the lesions as compared to needling. Hence, the response was better and faster in the needling group as compared to the intralesional MMR group.
Keywords
Intralesional MMR vaccine
needling
warts
Search for the most effective therapy for the treatment of warts is still on. When compared with intralesional MMR vaccine, needling has shown better and faster results and is also less painful and cost-effective.

INTRODUCTION
Warts are a notorious source of frustration for both the practitioners and the patients alike, as no single treatment is completely effective in all patients. Despite a plethora of medical literature available on this subject, high-quality evidence for the efficacy of almost all sorts of treatments is nonexistent.[1]
Treatment is difficult, with frequent failures and recurrences. Treatment strategies for warts can be categorized into ablative or cytodestructive therapies, topical modalities, and intralesional injections.[2] Studies comparing different wart treatments are few. An ideal treatment should result in resolution of majority of the warts; it should be painless, need only one of the multiple lesions to be treated, be cost-effective and non-scarring, and offer human papillomavirus (HPV) immunity for a lifetime. Hence, this study was carried out to determine such more efficacious, faster acting, cost-effective, and less painful therapy for warts.
This study aimed to compare the efficacy of intralesional measles, mumps, rubella (MMR) vaccine and needling in the treatment of recurrent warts.
The objectives of this study were as follows:
To assess the efficacy of needling in 20 patients of recurrent warts.
To assess the efficacy of intralesional MMR vaccine in another 20 patients of recurrent warts.
To compare the aforementioned modalities of treatment and determine the efficacy of these less invasive, non-scarring, and less painful modalities of treatment for recurrent warts.
SUBJECTS AND METHODS
In this study, a total of 40 patients diagnosed with recurrent warts attending the Dermatology outpatient department in a tertiary health-care center were selected.
This study was carried out with following two groups of 20 patients each.
Group A: Needling was performed on 20 patients. It was carried out under surface anesthesia cream (Eutectic Mixture of Local Anesthetics). The area was first cleansed with povidone-iodine and spirit. A 26.5-gauge needle was used to puncture the lesion up to the subcutaneous tissue. The largest wart was selected in cases of multiple warts. Each puncture would produce pinpoint bleeding points and this was continued until there was no more resistance from the epidermis. The total number of punctures would depend upon the size of the lesion. The procedure was performed every 2 weeks, that is, at 2, 4, and 6 weeks.
Group B: Intralesional MMR vaccine was given to 20 patients. The vaccine was reconstituted and a volume of 0.3 mL (12 units) was injected with the help of an insulin syringe into the wart or into the largest wart in patients with multiple warts. This was repeated every 2 weeks for a maximum of three treatment sessions, that is, at 2, 4, and 6 weeks.[3]
The results with the aforementioned two modalities were compared on the basis of colored photographs and following grades:[4]
Grade I: no response.
Grade II: 0%–49% reduction in size.
Grade III: 50%–99% reduction in size
Grade IV: complete clearance of the lesion.
RESULTS
A total of 40 patients were enrolled in the study with a diagnosis of recurrent warts. Twenty were treated with needling, whereas remaining 20 were treated with intralesional MMR vaccine. The mean age of the patients was 28.75 ± 11.86 years in the needling group, whereas it was 29.85 ± 12.44 years in the intralesional MMR vaccine group. Improvement was noted in patients belonging to both the groups [Figures 1–4]. However, after applying chi-square test, it was found that results were statistically significant in the needling group with a P value of <0.05 [Tables 1 and 2]. However, when both the groups were compared using chi-square test, needling showed statistically significant results after 4 and 6 weeks [Tables 3 and 4]. Male preponderance was observed in both the groups. It was 3:2 and was statistically insignificant (P > 0.05). The mean number of warts was 6.25 ± 3.82 in the needling group, whereas it was 3.35 ± 4.42 in the intralesional MMR vaccine group. This was statistically significant (P < 0.05). There was no statistically significant difference in the P value for resolution of distant warts between the two groups, although clinically resolution was more observed in the patients of the needling group. Fewer side effects were observed in both the groups. Mild pain after the procedure, which subsided within an hour and did not require any medication, was observed in four patients in the needling group. Pain and swelling after the procedure were observed in eight patients in the MMR group. The symptoms got relieved after taking one tablet of nonsteroidal anti-inflammatory drug.

- Needling performed for warts on feet
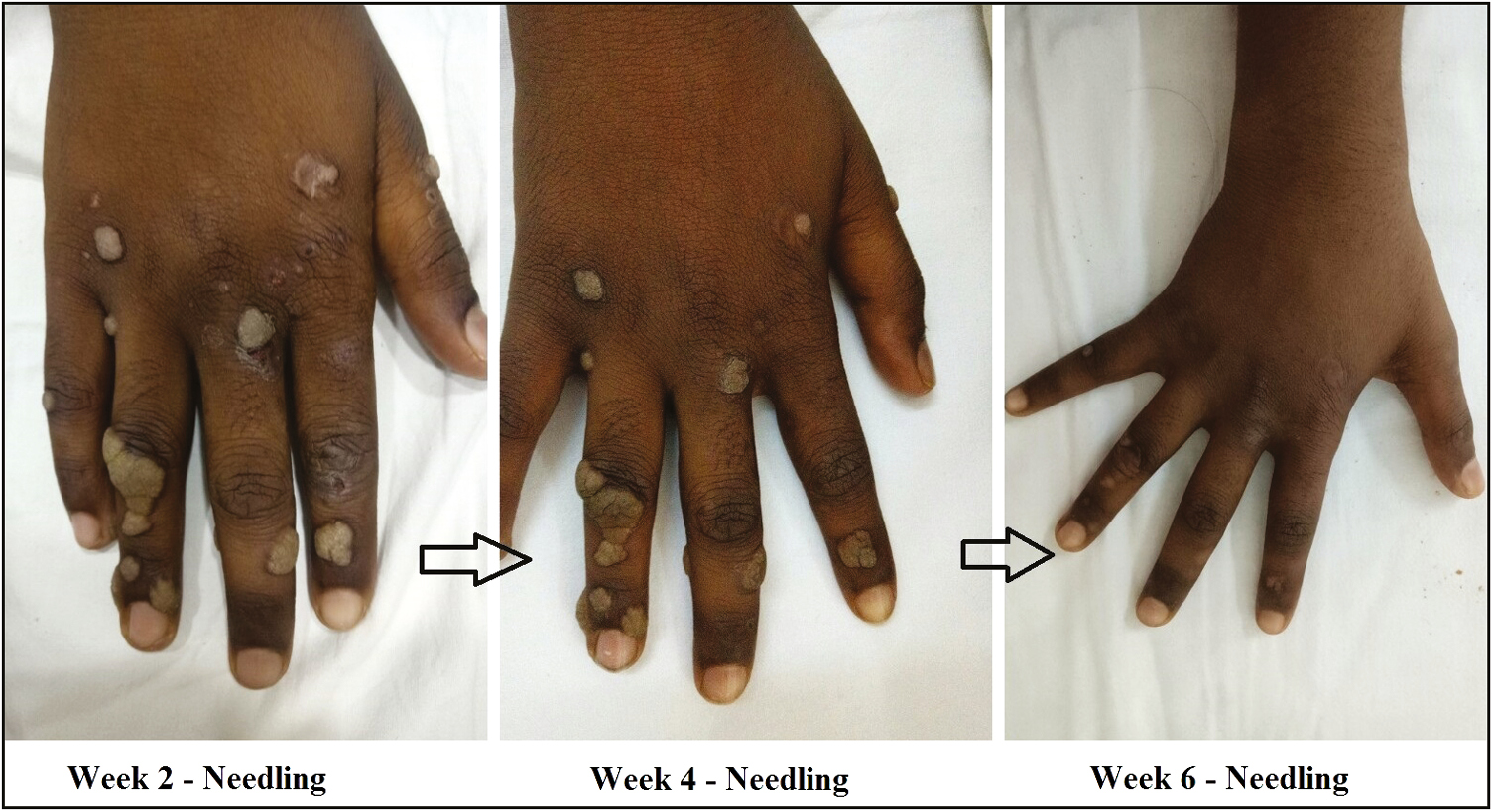
- Needling performed for warts on hands
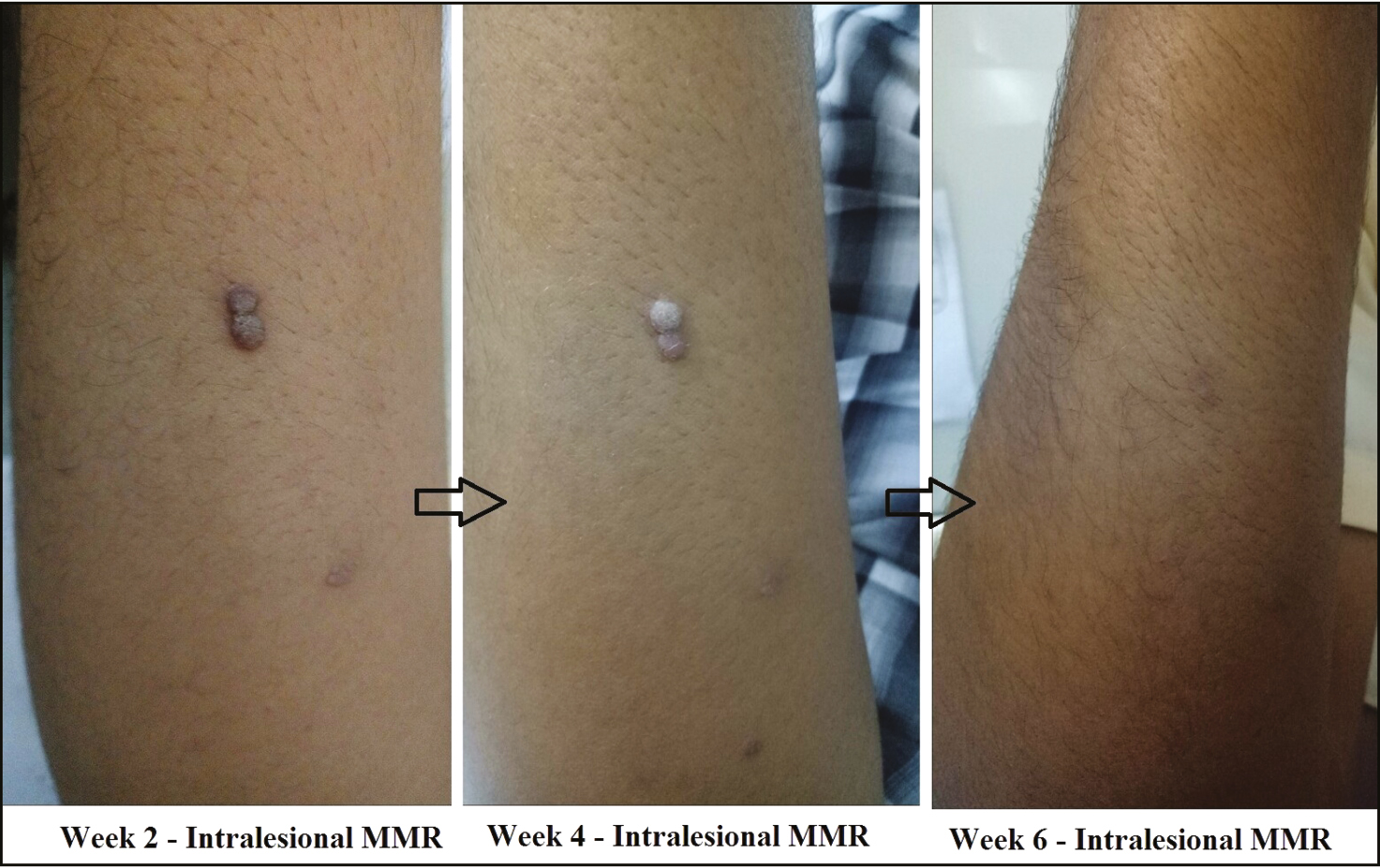
- Intralesional mumps, measles, rubella (MMR) vaccine for warts on arms
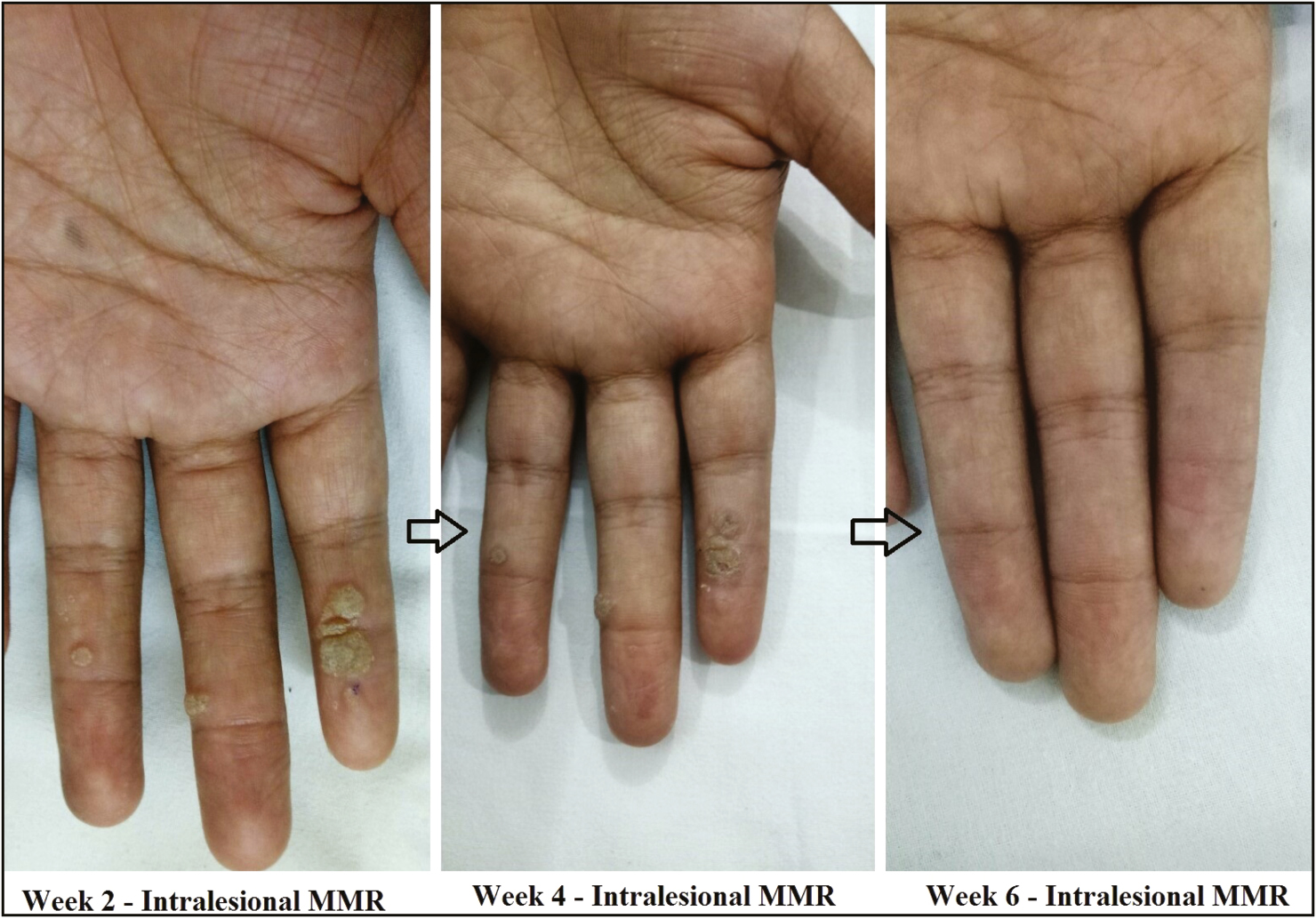
- Intralesional mumps, measles, rubella (MMR) vaccine for warts on palms
| Grades of improvement (%) | At 2 weeks | At 4 weeks | At 6 weeks | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| 0 | 9 | 45 | 5 | 25 | 3 | 15 |
| 1–49 | 4 | 20 | 2 | 10 | 1 | 5 |
| 50–99 | 3 | 15 | 4 | 20 | 1 | 5 |
| 100 | 4 | 20 | 9 | 45 | 15 | 75 |
| Grades of improvement (%) | At 2 weeks | At 4 weeks | At 6 weeks | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| 0 | 12 | 60 | 9 | 45 | 6 | 30 |
| 1–49 | 6 | 30 | 7 | 35 | 4 | 20 |
| 50–99 | 1 | 5 | 3 | 15 | 5 | 25 |
| 100 | 1 | 5 | 1 | 5 | 5 | 25 |
MMR = measles, mumps, rubella
| Grades of improvement (%) | Needling | MMR | ||
|---|---|---|---|---|
| n | % | n | % | |
| 0 | 5 | 25 | 9 | 45 |
| 1–49 % | 2 | 10 | 7 | 35 |
| 50–% | 4 | 20 | 3 | 15 |
| 100 | 9 | 45 | 1 | 5 |
MMR = measles, mumps, rubella
| Grades of improvement (%) | Needling | MMR | ||
|---|---|---|---|---|
| n | % | n | % | |
| 0 | 3 | 15 | 6 | 30 |
| 1–49 | 1 | 5 | 4 | 20 |
| 50–99 | 1 | 5 | 5 | 25 |
| 100 | 15 | 75 | 5 | 25 |
MMR = measles, mumps, rubella
DISCUSSION
Warts are viral infections caused by HPV belonging to the Papillomaviridae family. Although warts can affect any of the individuals, a few epidemiological variables are known. Age group between 9 and 16 years is at highest risk. The peak age is seen to be 14.5 years for males and 13 years for females.[5] HPV infections are extremely common but the vast majority of them are asymptomatic, with a prevalence ranging from about 1% to 20%. Three main types of cutaneous warts are recognized: common, plantar, and flat warts, each representing approximately 70%, 25%, and 5% of the lesions, respectively.
The therapies for the wart treatment are divided into two groups: destructive and immunomodulators. Destructive techniques constitute most of the traditional interventions such as trichloroacetic acid, 5-fluorouracil, podophyllin, podophyllotoxin, glutaraldehyde, bleomycin, retinoids, and contact sensitizers (formaldehyde and cantharidin), and physical modalities such as surgical excision and lasers.[6] Immunomodulators include agents such as interferon, imiquimod, cidofovir, and intralesional vaccines.
HPV proteins act by inhibiting immune responses by activating T-suppressor cells. Frazer[7] concluded that induction of cell-mediated immunity by exposure to early proteins of HPV has proven helpful as a therapeutic approach. There is a lack of immune response against the virus, so stimulating immune response against HPV is an emerging treatment strategy.[7]
Falknor[8] first described direct needling procedure as a treatment for warts. His method comprised anesthetizing the area, followed by thrusting the needle in a darting manner, so as to penetrate the full depth of the wart and exiting through the base of the capsule into the fat.[8] Needling stimulates immune system resulting in clearance of the verrucous lesions, in several patients. Introduction of HPV-infected keratinocytes into the subcutaneous layer probably facilitates a desired immune response. Intralesional antigen therapy can induce strong cell-mediated immunity, which could help to clear treated and also distant warts. Overall, the results of this study are quiet promising. Needling performed for just one lesion often produced a “cascade” effect, whereby the remaining untreated lesions also resolved in a number of patients. Thus, it can be observed that introducing HPV-infected particles into the subcutaneous layer facilitates a desired immune response.
MMR viral vaccine accelerates the clearance of virus and viral-infected cells by stimulation of cell-mediated and humoral immunity. It has been used in a dose of 0.5 mL injected into each cutaneous wart once in 2 weeks for up to five sittings to produce 63% complete resolution by Nofal et al.[9] Pain, itching, erythema, and flulike symptoms were the side effects noted.[9] Another study by Na et al.,[10] which involved 136 patients of warts, showed more than 50% reduction in the size of wart in 51% patients whereas only 5.6% had complete resolution. The only adverse event noted was pain at the injection site. Of 40 patients with multiple plantar warts, complete resolution was noted in 87% within three sittings by Gamil et al.[11] In a study conducted by Shaheen et al.,[12] the rate of lesional and distal resolution was 60% each with purified protein derivative (PPD), 80% and 40% with MMR, and 0% with saline, comparing MMR vaccine with intralesional PPD and saline in 10 patients each.
In our study, needling was found to be a better treatment modality as compared to intralesional MMR vaccine at the end of 4 and 6 weeks. More number of sessions were required in the intralesional MMR vaccine group for complete clearance of the lesions as compared to needling. Overall, the response was better and faster in the needling group as compared to the intralesional MMR group.
Hence, we concluded that needling was a safe, effective, faster, and cheaper modality of treatment for recurrent warts.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Surgical management of giant genital Condyloma acuminata by using double keystone flaps. Case Rep Urol. 2016;2016:4347821.
- [Google Scholar]
- Intralesional mumps, measles and rubella vaccine in the treatment of cutaneous warts. Indian J Dermatol Venereol Leprol. 2016;82:343-5.
- [Google Scholar]
- Effect of measles mumps rubella vaccine in treatment of common warts. Indian J Drugs Dermatol. 2017;3:14-9.
- [Google Scholar]
- Evidence-based review of management of nongenital cutaneous warts. Cutis. 2003;71:213-22.
- [Google Scholar]
- Therapy of cutaneous human papillomavirus infections. Dermatol Ther. 2004;17:441-8.
- [Google Scholar]
- Interaction of human papillomaviruses with the host immune system: A well evolved relationship. Virology. 2009;384:410-4.
- [Google Scholar]
- Treatment of recalcitrant warts with intralesional measles, mumps, and rubella vaccine: A promising approach. Int J Dermatol. 2015;54:667-71.
- [Google Scholar]
- Two-year experience of using the measles, mumps and rubella vaccine as intralesional immunotherapy for warts. Clin Exp Dermatol. 2014;39:583-9.
- [Google Scholar]
- Intralesional immunotherapy of plantar warts: Report of a new antigen combination. J Am Acad Dermatol. 2010;63:40-3.
- [Google Scholar]
- Intralesional tuberculin (PPD) versus measles, mumps, rubella (MMR) vaccine in treatment of multiple warts: A comparative clinical and immunological study. Dermatol Ther. 2015;28:194-200.
- [Google Scholar]





