Translate this page into:
Comparison of Two Types of Tapes for Taping After Breast Reconstruction Using Silicone Materials
Address for correspondence: Prof. Naohiro Ishii, Department of Plastic and Reconstructive Surgery, International University of Health and Welfare Hospital, 537-3 Iguchi, Nasushiobara City, Tochigi 329–2763, Japan. E-mail: ishinao0916@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Several kinds of tapes are used for postoperative wounds, which occasionally cause contact dermatitis and result in noticeable pigmentation. A comparison of the postoperative course between different tapes has not been reported. This study aimed at investigating the differences between two postoperative tapes used after breast reconstruction with silicone materials for simple mastectomy.
Materials and Methods:
Eighty-eight nonconsecutive patients undergoing tissue expander operation and 75 nonconsecutive patients undergoing tissue expander and silicone breast implant operations were included in this prospective study. Two postoperative tapes were used: a nonwoven surgical tape (Yu-ki ban®) or a hypoallergenic polyester-woven fabric tape (Atofine TM), which have different base materials, a removed keratinocyte area, and moisture permeability. We determined the differences in the incidence of skin complications, scar width, and aesthetic results with respect to scarring between the patients using Yu-ki ban and those using Atofine.
Results:
Statistically similar results were achieved for the patients who underwent reconstruction using either the tissue expander or silicone breast implant. Scar width was similar between the groups; however, the incidence of skin complications was significantly lower in patients using Atofine than in those using Yu-ki ban. Aesthetic results with respect to scarring were better in patients using Atofine than in those using Yu-ki ban, with a significant difference in the incidence of pigmentation between the groups.
Conclusion:
The tape with higher moisture permeability and a lower removed keratinocyte area should be used to reduce the incidence of contact dermatitis and achieve better aesthetic results with respect to scarring.
Keywords
Breast reconstruction
contact dermatitis
paper tape
taping
tissue expander
INTRODUCTION
The first study regarding postoperative taping, published in 1995, reported that a reduction in stretching forces to wounds using paper taping was effective in preventing hypertrophic scarring.[1] The scars treated with silicone materials significantly developed more hypertrophy than the scars treated with paper taping.[2] Further, a randomized controlled trial study provided evidence for the effectiveness of paper taping in reducing scar volume and preventing hypertrophic scar formation after cesarean section surgery.[3] Taping after plastic surgery is performed daily, and clinical consensus to its usefulness has been achieved.
To achieve a good aesthetic result in breast reconstruction, the creation of an acceptable reconstructed breast mound, as well as a fine scar, is required. In breast reconstruction using a tissue expander (TE) or a silicone breast implant (SBI) after simple mastectomy, the pectoral skin envelope is thin. Therefore, postoperative taping can cause contact dermatitis, which can lead to an infection of the TE or SBI.[4] Actually, we have experienced cases wherein contact dermatitis caused an infection of the TE, maintaining a full expansion. Subsequently, vacuum-assisted irrigation by saline perfusion was necessary to rescue the TE.
For postoperative taping after breast reconstruction in our institution, a nonwoven surgical tape (Yu-ki ban®), which was often used for postoperative wounds in domestic plastic surgery operations, had been widely used previously [Figure 1]. Currently, hypoallergenic polyester-woven fabric tape (Atofine TM) is widely used instead of this nonwoven surgical tape [Figure 2]. This hypoallergenic polyester-woven fabric tape is easily used without cutting and reduces skin irritation since it includes an adhesive material, showing a low removed keratinocyte area and high moisture permeability. Several kinds of taping are used for postoperative wounds; however, a comparison of the postoperative course regarding each tape has not been reported to date.
- Nonwoven surgical tape (®Yu-ki ban)

- Hypoallergenic polyester-woven fabric tape (®Atofine)
The purpose of this study was to investigate the differences between these two types of postoperative tape, regarding the incidence of skin complications, scar width, and aesthetic results with respect to scarring, following breast reconstruction (TE and SBI) after simple mastectomy.
MATERIALS AND METHODS
Between January 2013 and November 2017, we performed a prospective study of patients undergoing simple mastectomy with immediate TE insertion and replacement by SBI. Eighty-eight nonconsecutive patients undergoing TE operations and 75 nonconsecutive patients undergoing TE and SBI operations were identified and included. Atofine (Atofine TM, Nichiban, Tokyo, Japan) was used in 30 and 41 patients after a TE operation and an SBI operation, respectively (Atofine group). On the contrary, Yu-ki ban (Yu-ki ban®, Nitto Medical, Tokyo, Japan) was used in 58 and 34 patients after a TE operation and an SBI operation, respectively (Yu-ki ban group). Patients who underwent radiation therapy, had keloid diathesis, or had postoperative protracted wound healing were excluded. The same surgeons performed all surgeries.
Yu-ki ban was used until June 2016 and Atofine was used from July 2016 to date for postoperative taping, which was initiated the day after the sutures were removed and continued for four months according to the domestic guidelines.[4] As per each manufacturer’s recommendation, Yu-ki ban was changed every three days and Atofine was changed every one week. If patients were taped for less than four months, they were excluded from the study. Patients with contact dermatitis applied an ointment comprising a steroid or nonalcoholic skin barrier liquid (Remois-coat®, Alcare, Tokyo, Japan) and temporarily stopped taping according to the degree of dermatitis.
We measured the postoperative scar width and evaluated the postoperative scar by using the Vancouver Scar Scale,[56] five months after a TE operation and in one year after an SBI operation. A postoperative scar score (excluding the item of pigmentation) using the Vancouver Scar Scale was recorded. The average scar width (between the minimum and maximum widths) was recorded. We compared the width and scores of postoperative scars (including patients with contact dermatitis and those with pigmentation of the postoperative scar) between the Atofine group and the Yu-ki ban group.
Data were analyzed by using SPSS version 23 for Windows (IBM Corporation). The student’s t-test was used to compare the averages of continuous variables between groups, whereas Fisher’s exact test was used to compare independent categorical variables. For all statistical tests, P < 0.05 was considered statistically significant. The protocol of this study was approved by the relevant Institutional Review Board.
RESULTS
The characteristics of all patients included are shown in [Table 1]. Mean age, body mass index, and weight of resected tissue in mastectomy were all similar between the groups.
| Tissue expander | Silicone breast implant | |||
|---|---|---|---|---|
| Atofine group | Yu-ki ban group | Atofine group | Yu-ki ban group | |
| Cases | 30 | 58 | 41 | 34 |
| Age, years (range) | 48.7 (33–64) | 47.7 (18–71) | 47.4 (18–66) | 49.8 (31–71) |
| Body mass index, kg/m2 (range) | 21.9 (15.8–29.4) | 21.8 (15.8–28.5) | 21.7 (15.8–29.4) | 21.8 (15.8–27.3) |
| Weight of the resected tissue during mastectomy, g (range) | 308.0 (115–712) | 333.1 (73–768) | 298.7 (100–592) | 328.1 (73–706) |
Atofine group, patients using hypoallergenic polyester-woven fabric tape (®Atofine); Yu-ki ban group, patients using nonwoven surgical tape (®Yu-ki ban)
Results of scar width and scar score evaluated by the Vancouver Scar Scale are shown in [Table 2]. The scar width was similar between groups after either TE operation (P = 0.30) or SBI operation (P = 0.40). On the contrary, the scar score in the Atofine group was significantly higher than that in the Yu-ki ban group, after either TE operation (P < 0.05) or SBI operation (P < 0.05). In addition, the scar score, excluding the item of pigmentation, was similar between the groups after either TE operation (P = 0.49) or SBI operation (P = 0.88).
| Atofine group | Yu-ki ban group | P-value | |
|---|---|---|---|
| Scar width (TE), mm | 1.72 (1.0–3.0) | 1.85 (1.0–3.5) | 0.3 |
| Scar width (SBI), mm | 1.85 (1.0–3.5) | 1.97(1.0–2.5) | 0.4 |
| Scar Score (TE) | 2.27 (1–5) | 2.78 (0–5) | <0.05* |
| Scar Score (SBI) | 2.17 (0–5) | 2.79 (0–5) | <0.05* |
| Scar Score excluding the item of pigmentation (TE) | 2.13 (1–5) | 2.02 (0–5) | 0.49 |
| Scar Score excluding the item of pigmentation (SBI) | 1.95 (0–4) | 1.91 (0–5) | 0.88 |
* Statistical significance p<0.05; Atofine group, patients using hypoallergenic polyester-woven fabric tape (®Atofine); Yu-ki ban group, patients using nonwoven surgical tape (®Yu-ki ban); SBI, silicone breast implant; TE, tissue expander
After either a TE or an SBI operation, the number of patients with either contact dermatitis or pigmentation in the Atofine group was significantly lower than in the Yu-ki ban group (P < 0.05) [Figures 3 and 4].
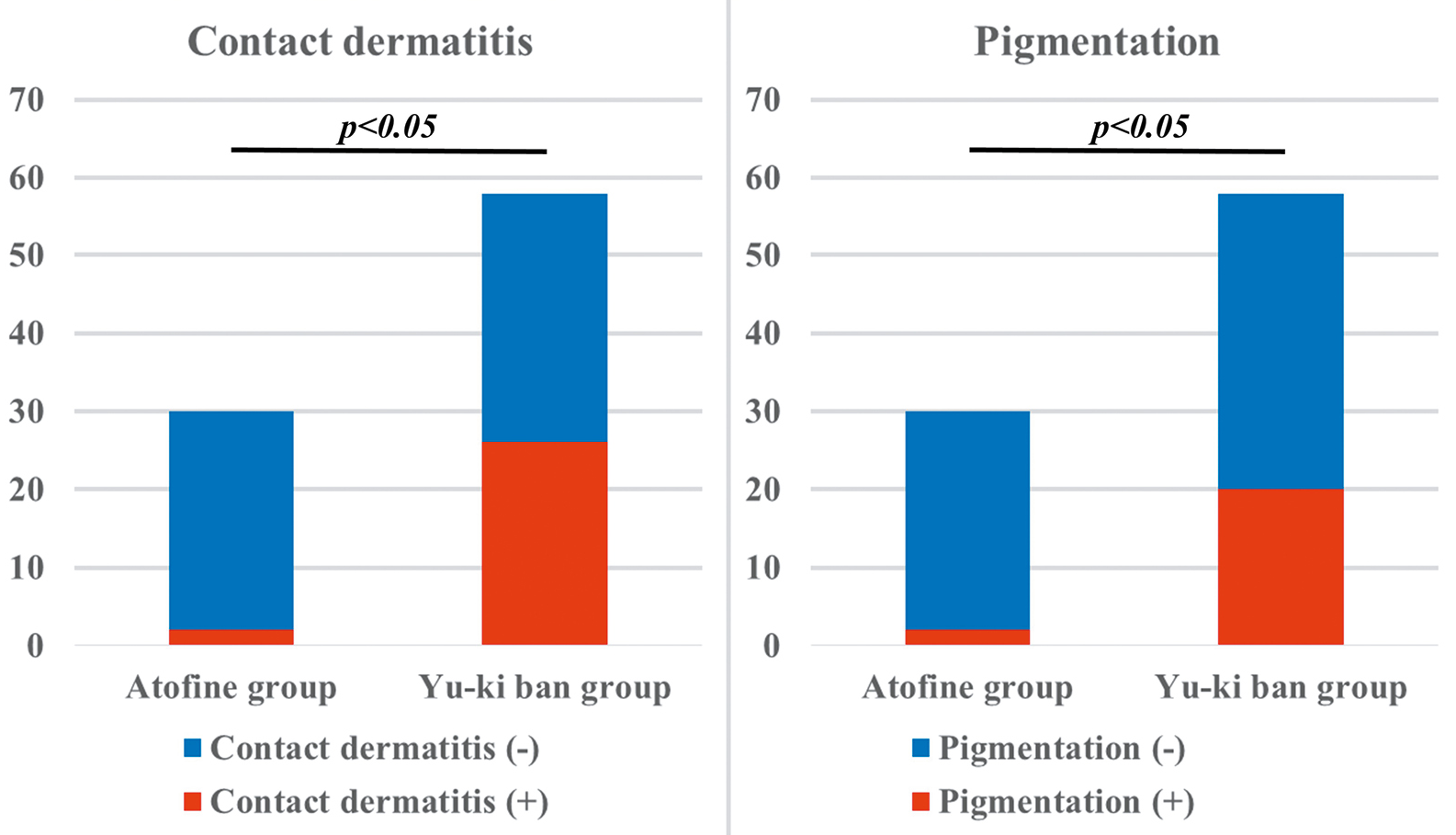
- Comparison of the number of patients with contact dermatitis and pigmentation in the scar after operation using the tissue expander between the Atofine group and the Yu-ki ban group
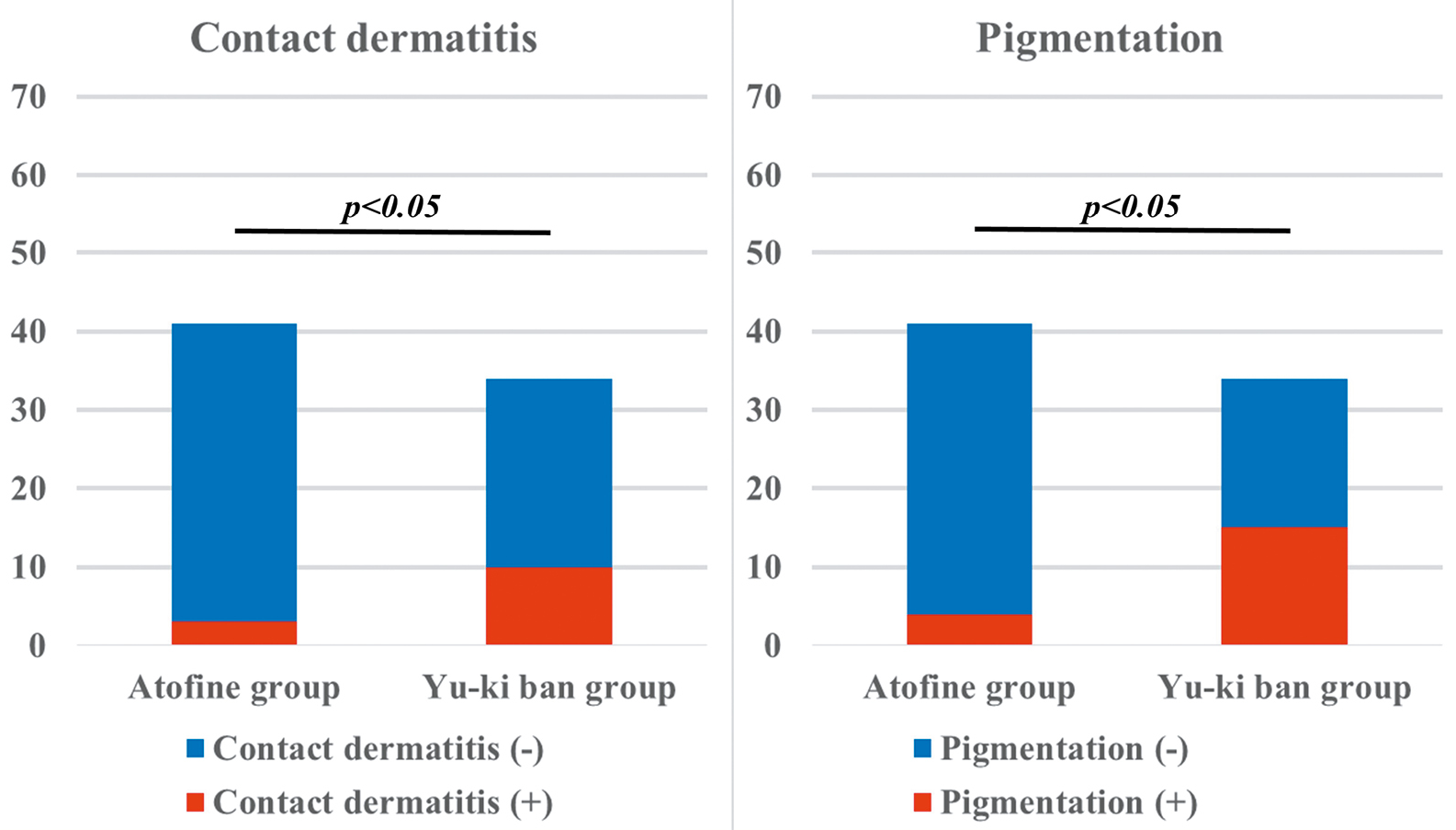
- Comparison of the number of patients with contact dermatitis and pigmentation in the scar after operation using the silicone breast implants between the Atofine group and the Yu-ki ban group
Severe complications were observed in two patients in the Yu-ki ban group after TE operation: They suffered from contact dermatitis, which caused infection of the TE, maintaining a full expansion [Figure 5A, B].
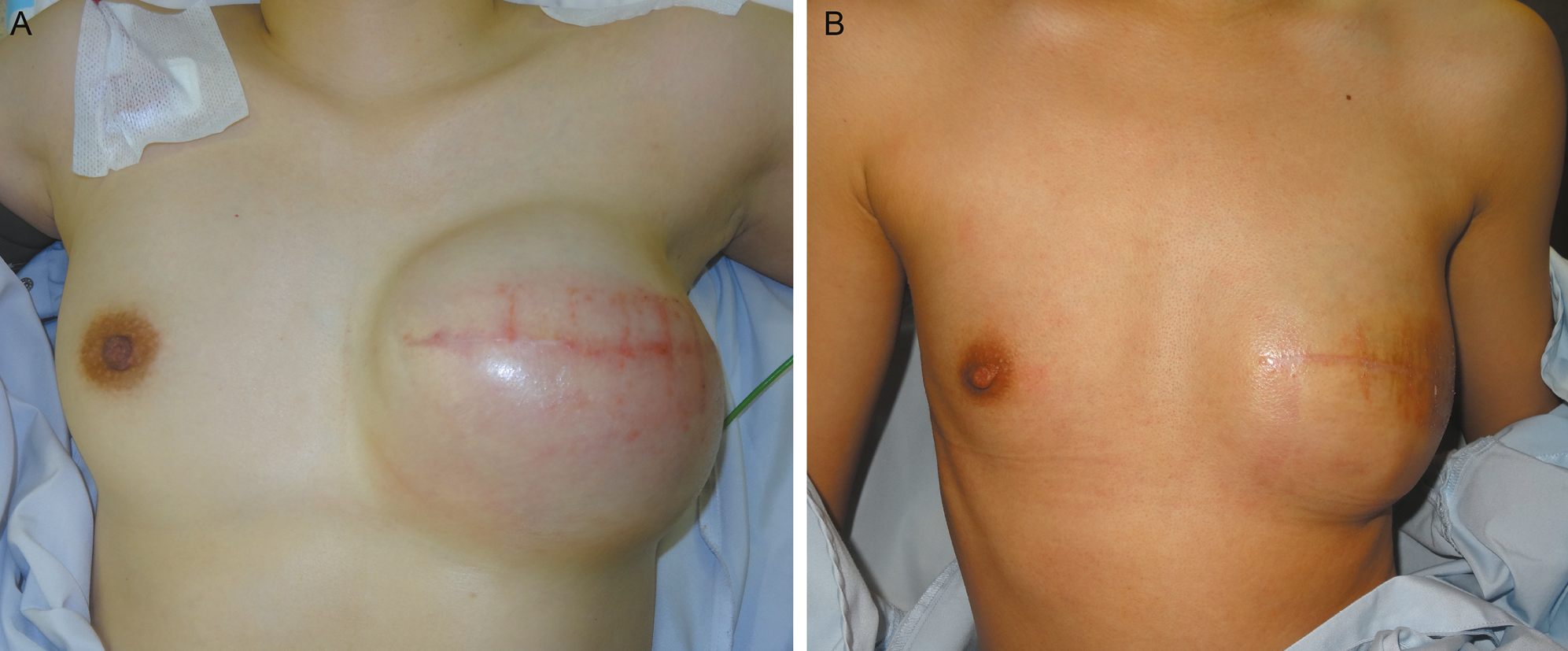
- Two cases in the Yu-ki ban group showing severe contact dermatitis, which caused infection of the tissue expander while maintaining a full expansion. (A) A 37-year-old woman undergoing a simple mastectomy of the left breast. (B) A 19-year-old woman undergoing a simple mastectomy of the left breast
DISCUSSION
We investigated the differences in the incidence of skin complications, scar width, and scar scores of aesthetic scars between two patient groups by using two kinds of postoperative tapes (Atofine and Yu-ki ban) after breast reconstruction with silicone materials for simple mastectomy. The results in either TE or SBI operations showed that scar width was similar between the groups; however, the incidence of skin complications in the Atofine group was significantly lower than that in the Yu-ki ban group. Aesthetic results with respect to scarring were better in the Atofine group than in the Yu-ki ban group, showing a significant difference in the incidence of pigmentation. Consequently, after breast reconstruction using silicone materials for simple mastectomy, we recommend Atofine rather than Yu-ki ban for postoperative taping.
Long-term postoperative taping occasionally causes contact dermatitis and, consequently, noticeable pigmentation.[4] Particularly, the skin envelope of patients undergoing breast reconstruction by using TE or SBI after simple mastectomy is often thin. Therefore, an appropriate kind of tape should be selected while considering the occurrence of contact dermatitis to prevent infection to the TE or SBI. However, a comparison of the incidence of skin complications and aesthetic results with respect to scarring between the different tapes has not been reported to date, and the appropriate selection of tape remains unresolved.
Internal data about the characteristics of four different tapes provided by Nichiban Co., Ltd. are shown in [Table 3]: hypoallergenic polyester-woven fabric tape (Atofine®), Surgical tape 1 (Yu-ki ban®), Surgical tape 2 (Micropore 3M®, 3M, Minnesota, United States), and Silicone tape (Mepitac®, Mölnlycke Health Care, Tokyo). Adhesive strength to a phenolic resin plate was measured by the Tensilon tensile test machine in accordance with Japanese Industrial Standards Z 0237. A specimen of 25 mm x 70 mm in the longitudinal direction was affixed to a phenolic resin plate. Twenty minutes after crimping the specimen, the peeling force was measured three times at a peeling angle of 180° and a peeling speed of 300 mm/min. The adhesive strength to the phenolic resin plate was calculated from the average values. The Micropore 3M had the strongest adhesive strength, those of Atofine and Yu-ki ban were moderate, and that of Mepitac was weak. Moisture permeability was measured as follows: The specimens were affixed on the hygroscopic agent and placed in a thermostatic chamber at 40°C and 90% RH. Time and mass changes were plotted on the graph, and the increase in mass per hour was calculated from the slope to calculate the moisture permeability. A tape with high moisture permeability easily removes moisture from scars. The moisture permeabilities of Yu-ki ban and Mepitac were lower than that of Atofine. The removed keratinocyte area was measured as follows: A 15 mm x 70 mm specimen was applied to the inside of the forearm for 24 hours. The specimen was removed from the skin, and the adhesive surface of the specimen was immersed in the cationic staining solution for 5–10 minutes. The removed keratinocyte area on the adhesive surface was calculated by taking pictures with a video microscope. The removed keratinocyte area after removing the tape was low using Atofine and Mepitac, whereas it was high using Micropore 3M. The cost was low using Yu-ki ban and Micropore 3M, moderate using Atofine, and high using Mepitac. All tapes can be obtained through online shopping.
| Hypoallergenic polyester-woven fabric tape (Atofine™) | Surgical tape 1 (Yu-ki ban®) | Surgical tape 2 (3M™ Micropore™) | Silicone tape (Mepitac®) | |
|---|---|---|---|---|
| Base material | Polyester woven | Nonwoven | Nonwoven | Knitted fabric and polyurethane film |
| Adhesive | Acrylic | Acrylic | Acrylic | Silicone |
| Adhesive strength to phenolic resin plate, N/25 mm | 2.6 | 2.54 | 3.96 | 1.24 |
| Moisture permeability, g/m2/24 h | 14520 | 1500 | 7710 | 200 |
| Removed keratinocyte area, % | <10 | 10-15 | 30-40 | <10 |
| 10% tensile strength in long axis, N/25 mm | 46.9 | 48.4 | 42 | 46.2 |
| 10% tensile strength in short axis, N/25 mm | 30.1 | Rupture | 15.1 | 19.9 |
| Shape | Flat and wave | Roll | Roll | Roll |
| Cost, dollars | 51 | 7 | 7 | 240 |
Cost; charge of postoperative taping (15 cm in length) during 4 months for the scars
Tensile strength was measured by the Tensilon tensile test machine in accordance with Japanese Industrial Standards K 7113. Cloth adhesive tape No. 123 made by Nichiban Co., Ltd. was applied to both ends of the test specimen cut to 25 mm x 40 mm in the short or long direction. It was set in the testing machine so that the distance between the chucks was 25 mm, and pulled at 300 mm/min, and the strength of the specimen when it was stretched by 10% was calculated. Overall, 10% tensile strength in both long and short axes was higher by using Atofine, since the base material of this tape is woven polyester, which hardly stretches. Therefore, Atofine is taped along the scar direction without several cuttings. This characteristic, including being wave-shaped [Figure 1], allows Atofine to disperse physical stress to the scar, thereby decreasing skin irritation. On the contrary, 10% tensile strength using other tapes is low in the short axis. Therefore, the other tapes should be cut approximately 5 cm long and taped vertically along the scar direction, and the assembly of these tapes measuring 5 cm in length should cover the whole scar. This characteristic allows these tapes to exert a physical stress vertical to the scar direction; hence, these tapes may increase skin irritation. Further, application of these tapes may be time-consuming since they require several cuttings, unlike Atofine.
Adhesive strength to the phenolic resin plate is related to the scar width, and the moisture permeability and removed keratinocyte area are related to the occurrence of contact dermatitis. The adhesive strength of Atofine is similar to that of Yu-ki ban; however, the moisture permeability of Atofine is higher than that of Yu-ki ban, and the removed keratinocyte area of Atofine is lower than that of Yu-ki ban. Supposedly, these results can support those of this study.
In postoperative taping, a tape providing higher adhesive strength, higher moisture permeability, and a lower removed keratinocyte area should be used. Further, a careful follow-up of the postoperative scar in breast reconstruction using silicone materials is required since the pectoral skin envelope is thin, and contact dermatitis may cause severe infection to the silicone materials. Atofine can provide moderate adhesive strength, high moisture permeability, and a low removed keratinocyte area. Further, it is a hypoallergenic polyester-woven fabric tape and exerts a low physical stress on the scar. Therefore, the incidence of contact dermatitis was low, and we suppose postoperative taping with Atofine was appropriate for breast reconstruction using silicone materials after simple mastectomy, although it requires moderate costs.
The amount of skin envelope, as well as skin elasticity dependent on age, may cause differing tension in the skin envelope and affect the scar width after simple mastectomy. However, the patient’s characteristics were similar between groups, and we suppose that these differences may be minimal. A further study comparing scars after using multiple tapes should be performed.
CONCLUSION
We investigated the differences in the incidence of skin complications, scar width, and aesthetic results with respect to scarring between the two postoperative tapes that have different base materials, a removed keratinocyte area, and moisture permeability, after breast reconstruction using silicone materials. The results showed that the tape with higher moisture permeability and a lower removed keratinocyte area should be used to reduce the incidence of contact dermatitis and achieve better aesthetic results. A careful follow-up of scarring after postoperative taping in breast reconstruction using silicone materials is warranted considering the development of contact dermatitis.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form/forms, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgments
The authors would like to thank Editage (www.editage.com) for English language editing.
REFERENCES
- Prevention of hypertrophic scars by long-term paper tape application. Plast Reconstr Surg. 1995;96:1715-8.
- [Google Scholar]
- The use of silicone occlusive sheeting (sil-K) and silicone occlusive gel (epiderm) in the prevention of hypertrophic scar formation. Plast Reconstr Surg. 1998;102:1962-72.
- [Google Scholar]
- A randomized, controlled trial to determine the efficacy of paper tape in preventing hypertrophic scar formation in surgical incisions that traverse langer’s skin tension lines. Plast Reconstr Surg. 2005;116:1648-56; discussion 1657-8.
- [Google Scholar]
- Scar in exposed sites. In: Kiyokawa K, ed. Clinical practice guideline for plastic and reconstructive surgery (Section 2:Acute wound, scar, and keloid) (1st ed.). Tokyo: Kanehara Publishers; 2015. p. :167.
- [Google Scholar]
- The vancouver scar scale: An administration tool and its interrater reliability. J Burn Care Rehabil. 1995;16:535-8.
- [Google Scholar]
- Standardized assessment of breast cancer surgical scars integrating the vancouver scar scale, short-form mcgill pain questionnaire, and patients’ perspectives. Plast Reconstr Surg. 2005;116:1291-9.
- [Google Scholar]






