Translate this page into:
Confirmation of molluscum contagiosum diagnosis: Harnessing innovative testing techniques
*Corresponding author: Senkadhir Vendhan, Department of Dermatology, BAMH Central Railway Hospital, Mumbai, Maharashtra, India. vendhan100@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vendhan S, Vasudevan B, Neema S, Kashif A. Confirmation of molluscum contagiosum diagnosis: Harnessing innovative testing techniques. J Cutan Aesthet Surg. doi: 10.25259/jcas_35_24
Abstract
Molluscum contagiosum can mimic conditions like syringoma, warts, and closed comedones, making diagnosis challenging. Histopathological confirmation often causes delays in treatment. A bedside diagnostic approach involving dermoscopy and microscopy can rapidly confirm molluscum contagiosum. In this case, a 9-year-old boy with facial papules underwent enucleation of one lesion, followed by dermoscopy, which revealed white structureless areas and tortuous vessels, and microscopy, which identified molluscum bodies. This method allowed for quick confirmation without the need for histopathology.
Keywords
Molluscum contagiosum
Tissue smear
Molluscum bodies
Bedside tests
Dermoscopy
PROBLEM STATEMENT
Molluscum contagiosum is a clinical diagnosis most of the time. However, in certain situations, the lesions may mimic syringoma, other appendageal tumors, closed comedones, warts, cryptococcosis, and histoplasmosis.1 Quick bedside tests may help resolve diagnostic dilemmas in such situations. Histopathology will take 3–7 days, thus losing precious time.
RECOMMENDED SOLUTION
The solution to the problem is explained here with a case vignette. A 9-year-old boy presented with numerous shiny, dome-shaped umbilicated papules over his face for 2 weeks [Figure 1]. Dermoscopy revealed white, structureless areas with telangiectasias around the edges [Figure 2]. Enzyme-linked immunosorbent assay for human immunodeficiency virus was negative. For bedside confirmation of diagnosis, one of the papules was carefully and aseptically enucleated, and the enucleated lobule was directly examined with a dermoscope and a microscope. Dermoscopy of the enucleated body showed a white homogeneous substance with tortuous enlarged vessels, while microscopy revealed a homogeneous golden yellow structure with numerous linear and branched vessels [Figure 3 and 4]. Giemsa staining under ×1000 microscopy of the crushed smear of the enucleated lobule revealed numerous intracytoplasmic basophilic inclusion bodies called molluscum bodies with few keratinocytes showing peripherally pushed nuclei that were confirmative of molluscum contagiosum [Figure 5 and 6]. Histopathological analysis for confirming the bedside test accuracy showed epidermal indentation into the dermis, thickened epidermis, and intracytoplasmic Henderson-Peterson bodies [Figure 7]. Enucleation of the papules was performed, followed by the application of trichloroacetic acid, with no recurrence of lesions after 3 months of follow-up.

- Shiny dome-shaped umbilicated papules over the face.
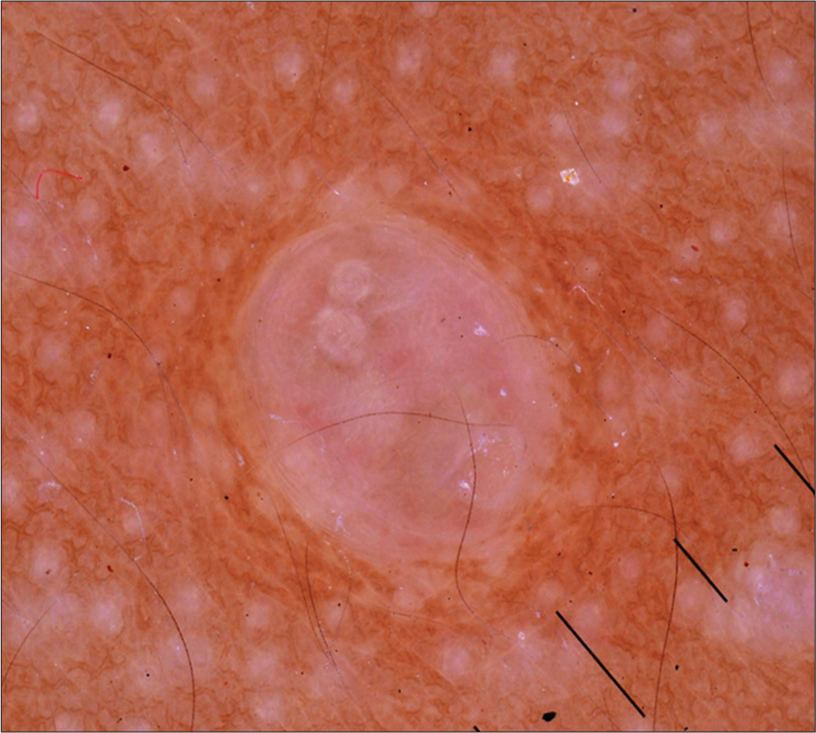
- Dermoscopy of lesion showing white structureless areas with peripheral telangiectasias.
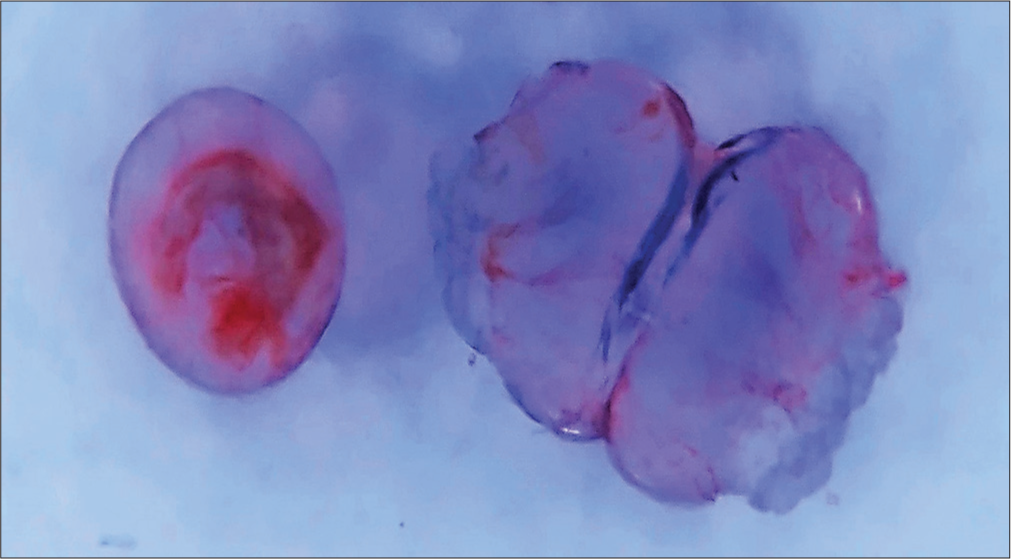
- Dermoscopy of the enucleated lobule.
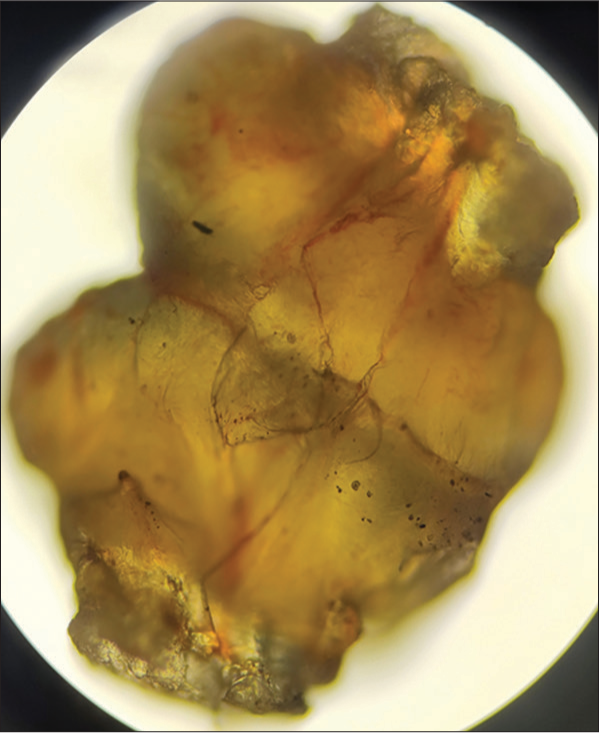
- Microscopic view (×10 ×10) of the enucleated lobule.
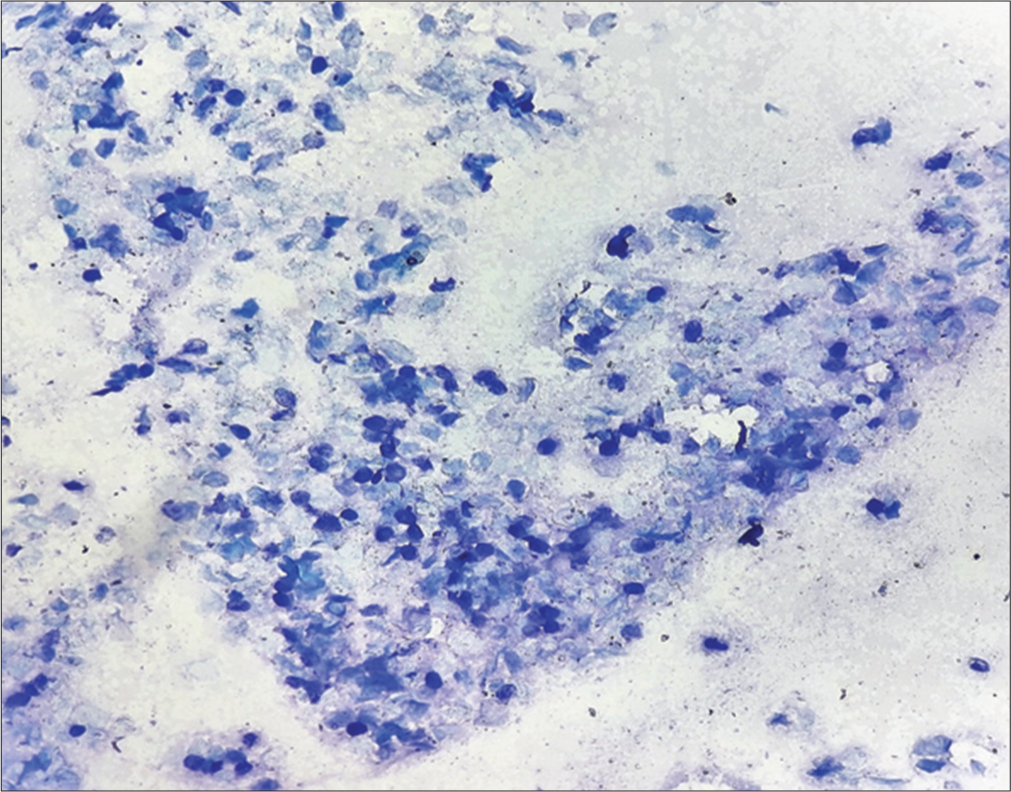
- Tissue smear of the enucleated lobule showing numerous intracytoplasmic basophilic inclusion bodies in low power (×10 ×10).
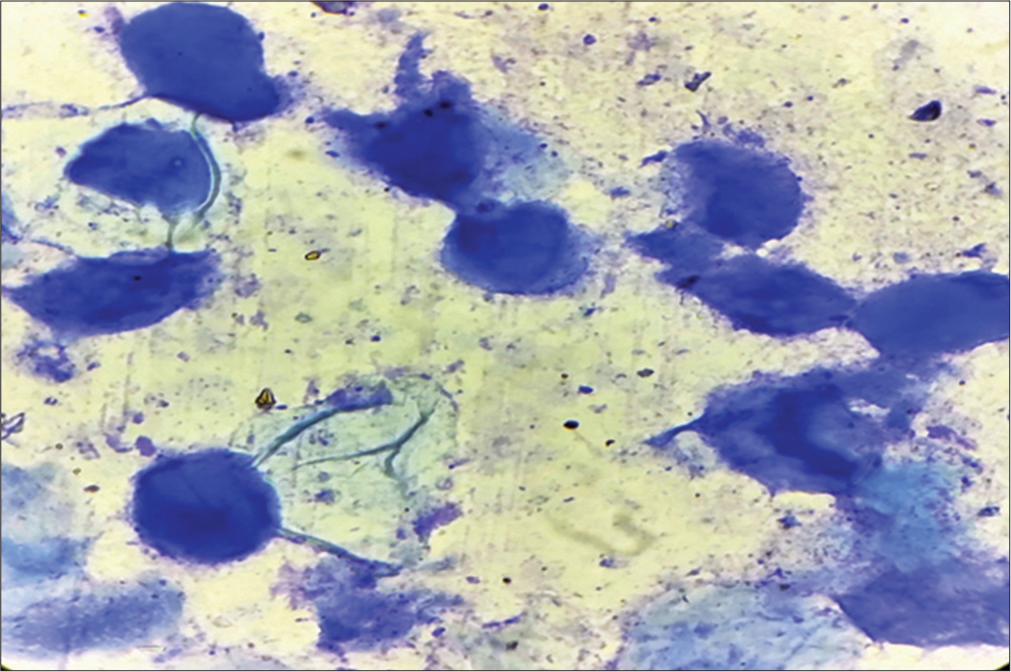
- High-power (100 × 10) view of intracytoplasmic inclusion bodies (Molluscum bodies).
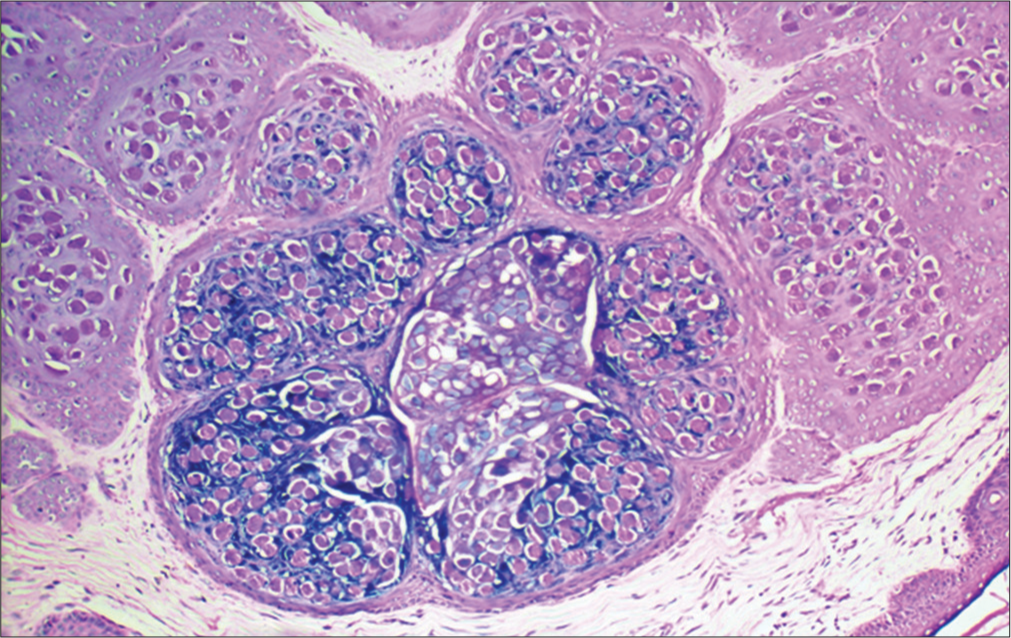
- Histopathological examination showing altered keratinocytes with numerous intracytoplasmic eosinophilic inclusion bodies.
Molluscum contagiosum can mimic conditions such as syringoma, other appendageal tumors, closed comedones, warts, cryptococcosis, and histoplasmosis; dermoscopy of molluscum reveals central umbilication, white-to-yellow polylobular amorphous structures, and peripheral crown vessels, while microscopy shows golden yellow structures with linear and branched vessels and basophilic molluscum bodies.2 Syringomas present as yellowish papules under dermoscopy and exhibit epithelial nests in the dermis on microscopy, while appendageal tumors show variable dermoscopic and microscopic features based on the tumor type. Closed comedones appear as uniformly white or yellowish papules dermoscopically, filled with keratin on microscopy, whereas warts display finger-like projections and hemorrhagic puncta dermoscopically, with hyperkeratosis and koilocytes histologically. Cryptococcosis and histoplasmosis show non-specific dermoscopic findings, with microscopy revealing encapsulated and intracellular yeasts, respectively. Differentiation relies on the unique presence of molluscum bodies, central umbilication, and specific dermoscopic and microscopic characteristics, with these bedside tests enabling quick, accurate diagnosis and avoiding the delays associated with histopathology. Dermoscopy expertise may not be present in all dermatologists, and it’s a need for a trained eye to discern the features as also the findings may be mimicked by other conditions. Histopathological examination requires time for reporting and may lead to a delay in treatment. Therefore, the presence of molluscum bodies that are enucleated can be confirmed by doing a Tzanck smear after crushing the bodies between two sterile glass slides like a tissue smear. Dermoscopy can also be done of the enucleated bodies to confirm the diagnosis as described in the case above. Failure to identify these bodies could cause these lesions to be mistaken for the other differential diagnosis, as mentioned previously. This obviates the need for a histopathological diagnosis.3 Thus, dermoscopy and microscopic examination of the enucleated molluscum body helps us in confirming the diagnosis of molluscum contagiosum.
Authors’ contributions
Senkadhir Vendhan: Concepts, definition of intellectual content, data acquisition, literature search, manuscript preparation. Biju Vasudevan: Concepts, definition of intellectual content, manuscript editing and review. Shekhar Neema: Concepts, manuscript preparation. A. W. Kashif: Histopathological images, manuscript editing.
Ethical approval
The authors confirm that they have obtained institutional ethics committee approval. Armed Forces Medical College, PG/2020/P3/5, dated 02/08/2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- A retrospective study of the pattern of sexually transmitted infections from a tertiary care hospital of Rajasthan. Indian J Sex Transm Dis AIDS. 2017;38:147-51.
- [CrossRef] [Google Scholar]
- Dermoscopic patterns of molluscum contagiosum: A study of 211 lesions confirmed by histopathology. An Bras Dermatol. 2011;86:74-9.
- [CrossRef] [Google Scholar]
- Cytologic diagnosis of molluscum contagiosum in scrape samples from facial lesions. Diagn Cytopathol. 2003;29:84.
- [CrossRef] [Google Scholar]







