Translate this page into:
Correction of Areolar Protuberance During Augmentation Mammoplasty in Transfemale Patients
Address for correspondence: Dr. Emrah Kagan Yasar, Department of Plastic, Reconstructive and Aesthetic Surgery, Kocaeli University, Kocaeli, Turkey. E-mail: emrahkaganyasar@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Augmentation mammoplasty refers to “top surgery” for transfemale patients. Before this surgery, due to the hormonal treatment being taken, it may be encountered that there would be a glandular tissue of breast that seems to be similar to the simple tuberous breast disease, which is one of the diseases in female breast development. The presence of areolar protuberance in transfemale would of course undermine the cosmetic gain after augmentation mammoplasty operation. This situation, which can be difficult to diagnose before surgery especially in transfemale patients, will manifest itself clearly after the end of augmentation mammoplasty. As a precaution, resection of a part of glandular tissue equal to the protruding height of the areola from the posterior wall of the gland is an effective method both in terms of its simple applicability and not to use of an extra skin incision while performing augmentation mammoplasty.
Keywords
Areolar protuberance correction
augmentation mammoplasty
subglandular
transgender
AIM
Augmentation mammoplasty refers to “top surgery” for male-to-female transgender patients.[1] In this patient group, breast augmentation is a quality-of-life operation and not simply a cosmetic procedure,[2] so it is necessary to meet the expectations of transgender patients for this “top surgery” with precision. Maximum breast volume will be achieved in the second year with hormonal treatment only, and before surgery, but more than a half of transgender patients do not have a satisfactory volume.[3] However, during the change of glandular structure, either after hormonal therapy or augmentation mammoplasty, disproportionality in breast size, subareolar tissue volume, and nipple proportions can cause discomfort and dissatisfaction for patients.
The presence of a dense glandular structure below the areola in transgender patients may undermine the cosmetic gain after the augmentation mammoplasty operation. The combination of subareolar glandular structure density with an insufficiency of peripheral fat tissue in the neo-breast increases the selectivity of disproportionality, which becomes even more apparent after augmentation mammoplasty. The aim of this article is to present a novel approach that can be applied during the augmentation mammoplasty operation to eliminate or decrease this disproportion.
SURGICAL APPROACH
The author prefers an inframamarian incision for augmentation mammoplasty surgery for male-to-female transgender patients. It is not important where to create the space for the prosthesis because subglandular or dual plane preference may vary from patient to patient. The decision concerning where to create this space can be made with the pinch test performed on the upper pole of the breast. After subglandular or subfascial dissection, the amount of protuberance is reconfirmed with the prosthesis sizer, perioperatively [Figure 1]. Evidently, the appearance of the areolar protrusion deformity increases after putting in the prosthesis.
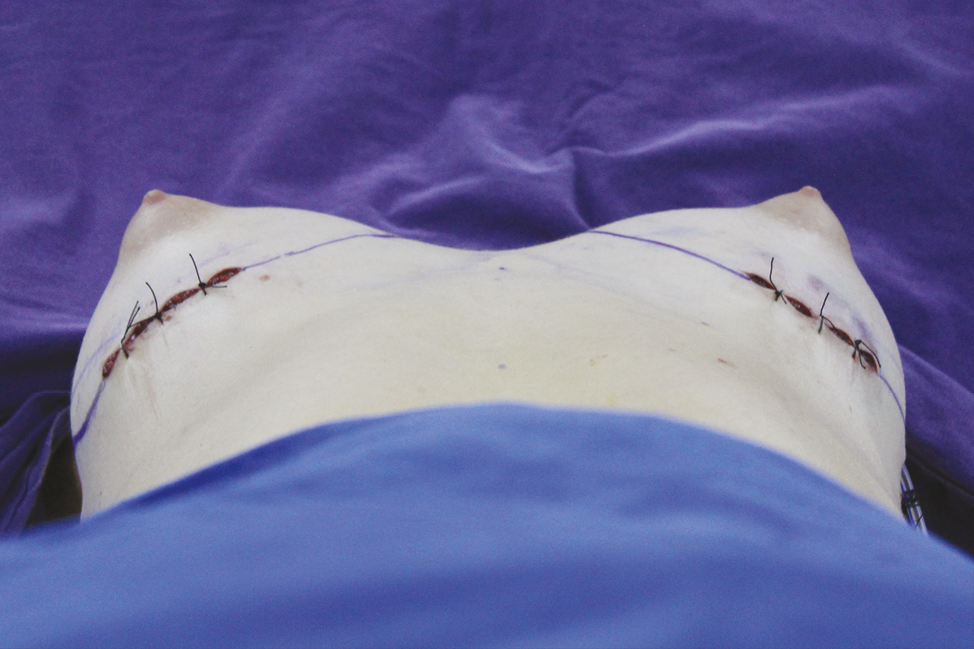
- After the inframamarian incisional approach for augmentation mammoplasty, the areolar protrusion becomes prominent with placement of the prostheses. It is best observed from the lateral and basal viewpoints
The main goal of the method is to remove a region of glandular tissue that equals the diameter of the areola (see the scheme in Figure 2). For this purpose, an incision is made at the place where the infra-areolar border projects onto the posterior wall of the gland, toward the fascia. First, a pocket is opened with this incision. The aim is to resect a rectangular shaped portion of tissue into this pocket; the edges of this rectangle should match the diameter of the areola. It is also important to resect this tissue so that its height equals the amount of areolar protrusion tissue height and not more, to prevent the sinking of the areola. Using monopolar cautery, after the upper face, sides, and lower face dissections are completed, the posterior edge of the slice to be removed is freed easily [Figure 3]. After the end of the resection and hemostasis, the approach incision on the glandular posterior wall can be repaired with polyglactin 3-0 interrupted sutures with reverse knotting toward the area of resection. Comparisons can be made with the opposite areolar deformity to confirm that the deformity has improved after resection on one side [Figure 4]. While doing this, temporary repair of the inframamarian incision is reasonable to enhance comparison. At the six-month postoperative evaluation of the patient, it is seen that the areolar protrusion that was present during the operation is no longer present [Figure 5].
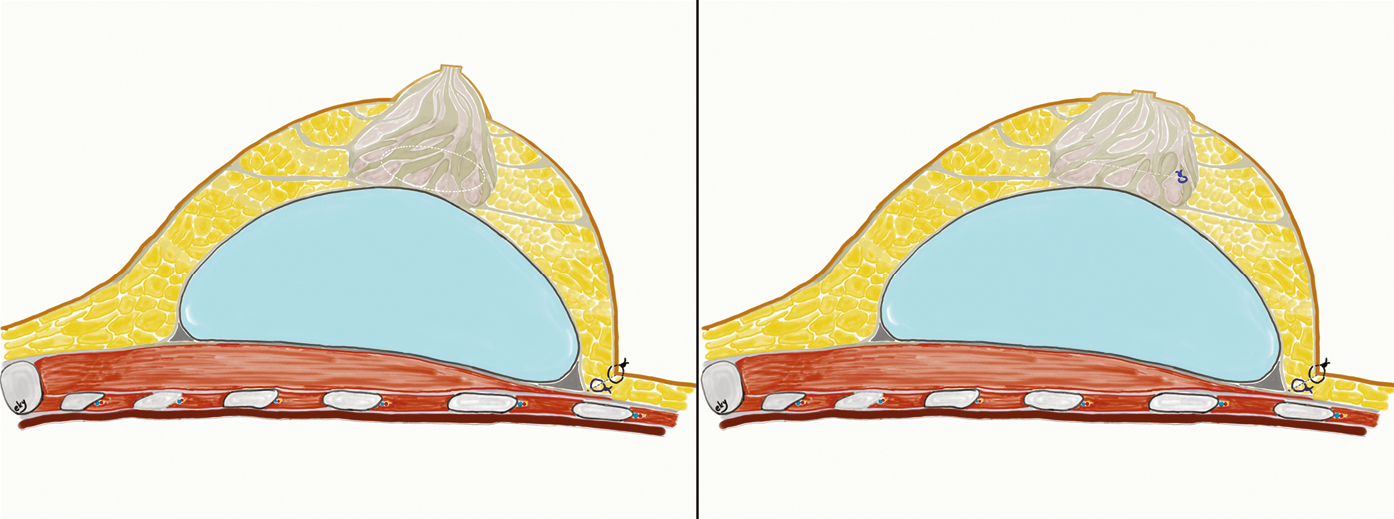
- As can be seen in the schematized version of the increased areolar bump, the glandular structure becomes more protruberant with the effect of the underlying prosthesis (top). Surgical approach is with an incision made on the fascia on the posterior wall of the gland, close to the lower border projection of the areola. In order to decrease the height of the areola, a partial glandular tissue resection is performed, which should match the width and height of the areola (below).
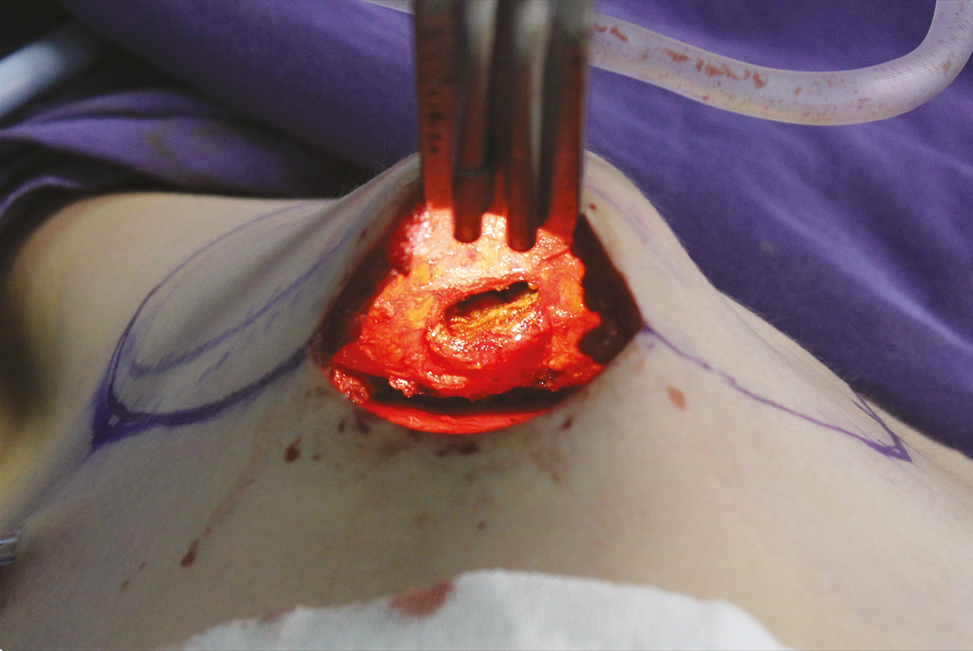
- The surgical approach to the posterior glandular area following inframamarian incision is shown. A perioperative view, just before fascial repair and after resection from the area opened by a horizontal incision to the fascia
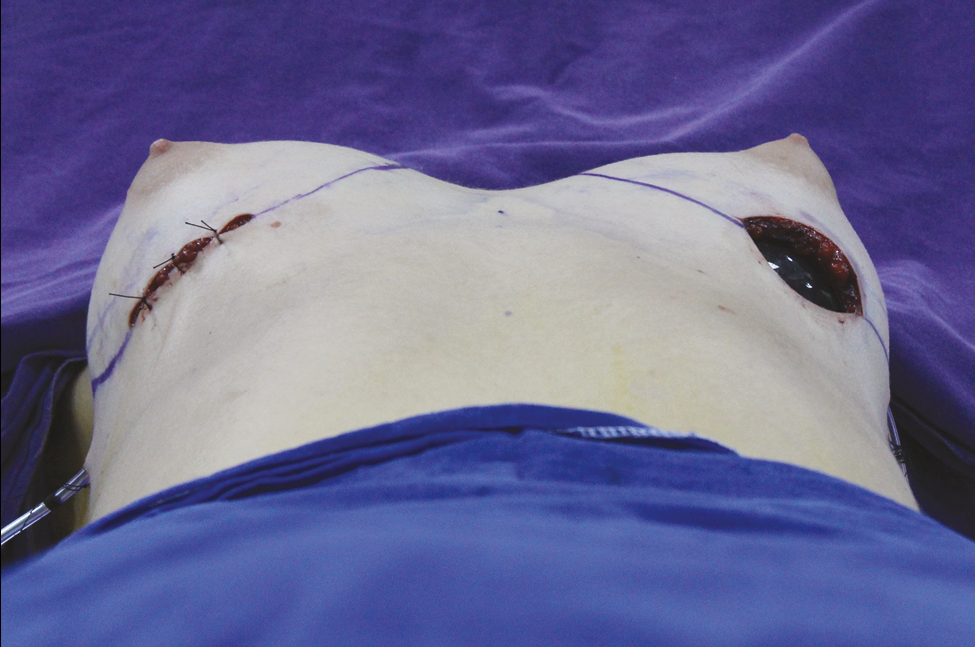
- The perioperative reduction in areolar protrusion is seen in the right breast. The decrease in height of the right areola, performed by posterior glandular reduction, is evident and can be compared with the unmodified left breast
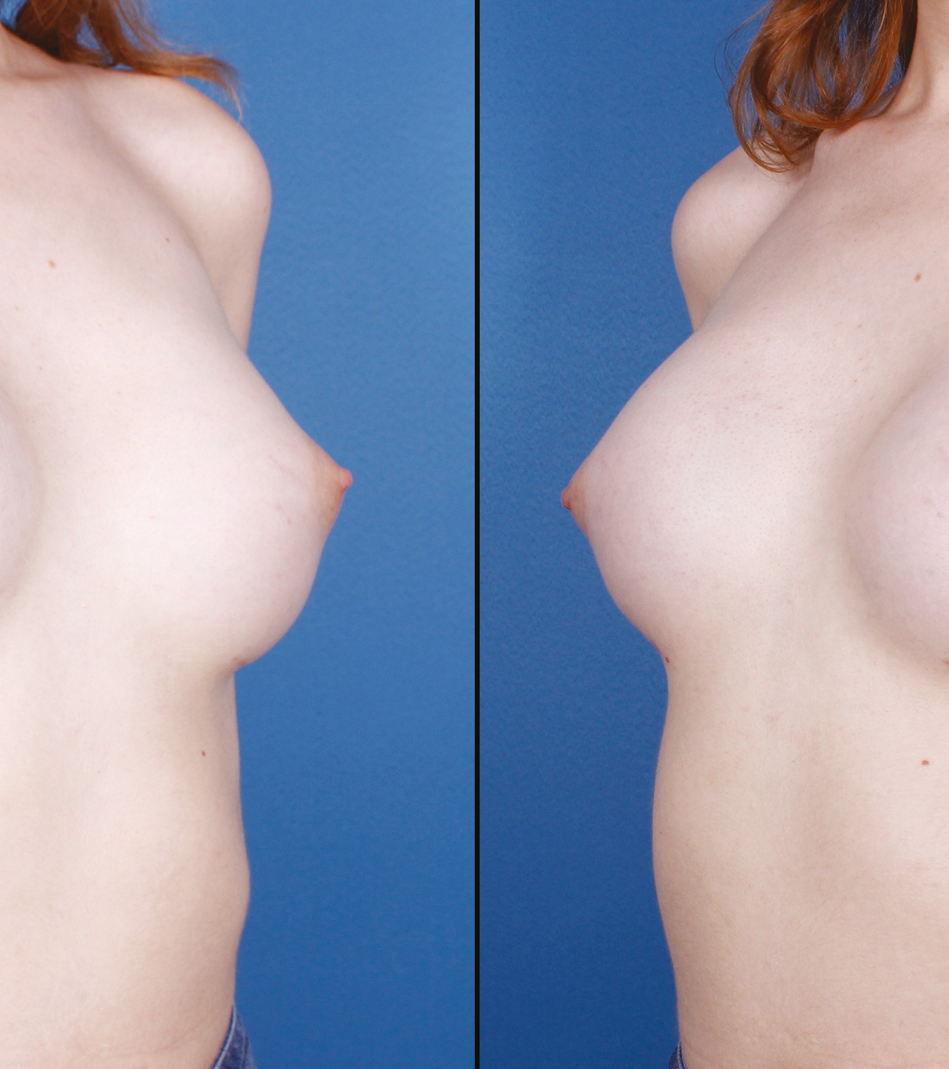
- The left areola (left) and the right areola (right) have no areolar protrusion appearance in the sixth month postoperatively
DISCUSSION
Isolated areolar protrusion with normal mammary base is also known as herniated areola. In this deformity, the areolar protrusion may become more apparent after manual compression.[4] Satisfactory breast development is possible with hormonal treatment that transgender patients may receive for years, but most patients complete this development with prosthetic repair.[3] In addition to deficiencies of glandular tissue development, there may be structural irregularities such as tuberous breast deformity. In women, simple areolar protrusion is a form of tuberous breast deformity (type 0) and is the result of an anatomical anomaly characterized by congenital structural weakness and lack of elasticity of the areola. It has also been suggested that an imbalance between estradiol and progesterone during the mammary growth phase may also lead to this type of anomaly.[4] A transgender patient, using exogenous and possibly supraphysiological hormone therapy, may also develop this kind of tuberous breast deformity. However, this anomaly may be difficult to perceive, especially with the untrained eye and for transgender patients.[5]
The inframamarian incisional approach for augmentation mammoplasty makes it easier to reach the posterior part of the gland. While reaching and dissecting the part of the glandular tissue that will be resected, the integrity of the deep layer of the superficial fascia is not affected. After the end of the resection, the horizontal incision in this fascia is repaired with absorbable sutures. The prosthesis should be prevented from contacting any extrafascial structures. Although there is no significant difference in prospective studies between subglandular or subfascial prosthesis application in terms of capsular contracture,[6] after much experience, the author prefers subfascial prosthesis application. It is possible to achieve the reduction of areolar protuberance vertically during augmentation mammoplasty, but an infra-areolar incisional approach for transgender patients has disadvantages due to the narrowness of areolar diameter.[7] It would be thought that there would be a low risk of glandular asymmetry, areolar irregularity due to asymmetric resection, and deep infection risk after posterior glandular resection. Asymmetry can be prevented by leaving equal tissue with symmetric or asymmetric resection in the line with bilateral evaluation of areolar protuberance. It is also thought that the risk of infection of gland and periprosthetic area is not increased too much because of the contact of the prosthesis and the glandular structure is prevented by repairing the prepectoral fascia after partial glandular resection.
Another option for the correction of areolar protuberance is periglandular fat injection. In this application, gradually large amounts of fat injections may be required, which also requires a large volume of donor sites. If the body mass index (BMI) of patients is higher than 25 kg/m2, the probability of areolar protrusion caused by hormonal treatment is already low for transfemale patients. But if areolar protuberance is existing, fat grafting may solve the problem. Sometimes it is possible that transfemale patients are likely to try to lose excessive weight with the desire to be favored. Like the case used in this innovative study, the patients with low BMI have low chance of using fat graft due to low volumes of fat graft donor site. Therefore, the innovative technique described in the study provides simultaneous treatment of this group of patients.
Two-stage reconstruction procedure may be preferred rather than one-stage reconstruction, especially for skinny patients who have low breast skin laxity.
It is not thought that the application of subpectoral or prepectoral expander will make a significant difference in transfemale patients. Of course, it is a well-known thing that the pectoral muscle can improve the upper pole contour. The muscle can be used in both sessions. And also it is not necessary to put the prosthesis at the same level as the expander in the second session. It is possible to change the plane from prepectoral plane to dual plane in the second session. Therefore, preparing and using the pectoral muscle for augmenting the upper pole is possible in both sessions. However, due to the risk of animation deformity, it is thought that prepectoral applications may give good results especially for sportive patients, and this is also the author’s preference.
Transfemale patients may rarely have asymmetric breasts, and fat grafting,[8] asymmetric resection of glandular tissue,[9] and asymmetric prosthesis application[10] as performed in XX females are the options for correction. In cases where only an asymmetric areolar protrusion is present, it is thought that an asymmetrical glandular resection may be a suitable solution after calculating the vertical height difference bilaterally. Perioperatively, bilateral application of prosthesis sizers, which have the same volume and tightness, increases the success rates of correctly calculating the volume of glandular tissue requiring resection.
This technique was performed for only one case of a special group of patients, which means that it is the biggest reason for the limitation of this study. Therefore, there is a need for studies comparing the late results of alternative applications that can be applied in similar patients.
Even before transfemale augmentation mammoplasty surgery who are receiving hormonal therapy, a finding of tuberous breast anomaly should not be overlooked. It should be kept in mind that a good cosmetic gain may easily be achieved by performing partial glandular resection with the same skin incision to be used for augmentation mammoplasty, resulting in improved quality of life for this group of patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Breast augmentation for transfeminine patients: Methods, complications, and outcomes. Gland Surg. 2020;9:788-96.
- [Google Scholar]
- Patient satisfaction with breasts and psychosocial, sexual, and physical well-being after breast augmentation in male-to-female transsexuals. Plast Reconstr Surg. 2013;132:1421-9.
- [Google Scholar]
- Endocrine treatment of transsexual people: A review of treatment regimens, outcomes, and adverse effects. J Clin Endocrinol Metab. 2003;88:3467-73.
- [Google Scholar]
- Tuberous breast: Revised classification and a new hypothesis for its development. Aesthetic Plast Surg. 2013;37:896-903.
- [Google Scholar]
- The incidence of tuberous breast deformity in asymmetric and symmetric mammaplasty patients. Plast Reconstr Surg. 2006;118:1667.
- [Google Scholar]
- Is there a breast augmentation outcome difference between subfascial and subglandular implant placement? A prospective randomized double-blinded study. Aesthetic Plast Surg. 2019;43:1429-36.
- [Google Scholar]
- Chest surgery for transgender and gender nonconforming individuals. Clin Plast Surg. 2018;45:369-80.
- [Google Scholar]
- Refining aesthetic approaches to tuberous breast using combined minimally invasive approaches to treat moderate asymmetric tuberous breast. J Surg Case Rep. 2020;2020:rjaa373.
- [Google Scholar]
- Correction of small volume breast asymmetry using deep parenchymal resection and identical silicone implants: an early experience. Aesthet Surg J. 2015;35:394-401.
- [Google Scholar]
- Asymmetric implants for breast asymmetry. J Plast Reconstr Aesthet Surg. 2012;65:1580-3.
- [Google Scholar]






