Translate this page into:
Cutaneous horn with underlying squamous cell carcinoma complicating discoid lupus erythematosus of scalp: A hitherto unreported complication
*Corresponding author: Archana Singal, Department of Dermatology & STD, University College of Medical Sciences & GTB Hospital, New Delhi 110095, India. archanasingal@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bisherwal K, Singal A, Bhoi AK, Sharma S. Cutaneous horn with underlying squamous cell carcinoma complicating discoid lupus erythematosus of scalp: A hitherto unreported complication. J Cutan Aesthet Surg. doi: 10.4103/JCAS.JCAS_61_23
Abstract
Cutaneous horn, characterized by conical protrusion arising from the skin surface, comprises hyperkeratotic epidermis. It is commonly seen on photo-exposed body parts in elderly men and can arise from benign, premalignant, or malignant dermatoses. There are scarce reports of cutaneous horn developing in association with discoid lupus erythematosus (DLE). We report an interesting case of cutaneous horn with underlying well-differentiated squamous cell carcinoma (SCC) arising over chronic scarred lesion of DLE on the scalp.
Keywords
Cutaneous horn
DLE
SCC
INTRODUCTION
Cutaneous horns, also known as cornu cutaneum, resemble a spicule or corn in the shape of an animal horn. They commonly present as well-circumscribed, solitary lesions comprising compact keratin from the basal keratinocytes and can arise from a variety of benign, premalignant, and malignant conditions. Discoid lupus erythematosus (DLE) has been infrequently associated with cutaneous horn. Moreover, malignant transformation in DLE is also rare. Clinical and dermoscopic pointers toward underlying malignancy in cutaneous horn have been recently described. Herewith, we describe a case of cutaneous horn on the scalp arising over chronic scarred lesion of DLE with underlying well-differentiated squamous cell carcinoma (SCC) along with its histopathological and dermoscopic features.
CASE REPORT
A 60-year-old woman, known case of disseminated DLE with lupus nephritis for 15 years, presented with growth on the scalp of 3 years duration. The growth started as asymptomatic, small lesions, and progressively increased in size and coalesced to form a large painful exophytic growth. There was no history of preceding trauma, ulceration, or bleeding. She had not taken any medication in the last 3 years. Her general physical examination was normal. Cutaneous examination revealed multiple depigmented, atrophic plaques present over scalp, face, trunk, and extremities. A large cutaneous horn of size 6 cm and height 3 cm with raised, erythematous base was present in the center of a depigmented cicatricial plaque on the vertex. The base of the horn was fixed, indurated, and tender. Another small cutaneous horn was present posteriorly [Figure 1]. The rest of the mucocutaneous and systemic examination was normal. Polarizing dermoscopy showed structureless white areas, arborizing vessels, scaling, and the absence of a terrace pattern at the base [Figure 2]. An excision biopsy from the base of horn on hematoxylin and eosin-stained sections (40×) revealed well-delineated nests of tumor cells infiltrating the whole dermis. Multiple keratin pearls were seen on higher magnification (100×). The squamous cells were polyhedral with vesicular nucleus, abundant eosinophilic cytoplasm, and prominent intercellular bridges, indicating well-differentiated SCC [Figure 3]. Apart from microcytic hypochromic anemia, hematological and biochemical investigations including connective tissue disease profile were normal. Contrast- enhanced computerized tomography scalp did not show involvement of deeper structures. She was referred to the oncosurgery department for wide local excision with flap surgery and further management.

- Cutaneous horn with raised, nodular and erythematous base present in the center of depigmented cicatricial plaque on the scalp. Note another smaller cutaneous horn present posteriorly (arrow).
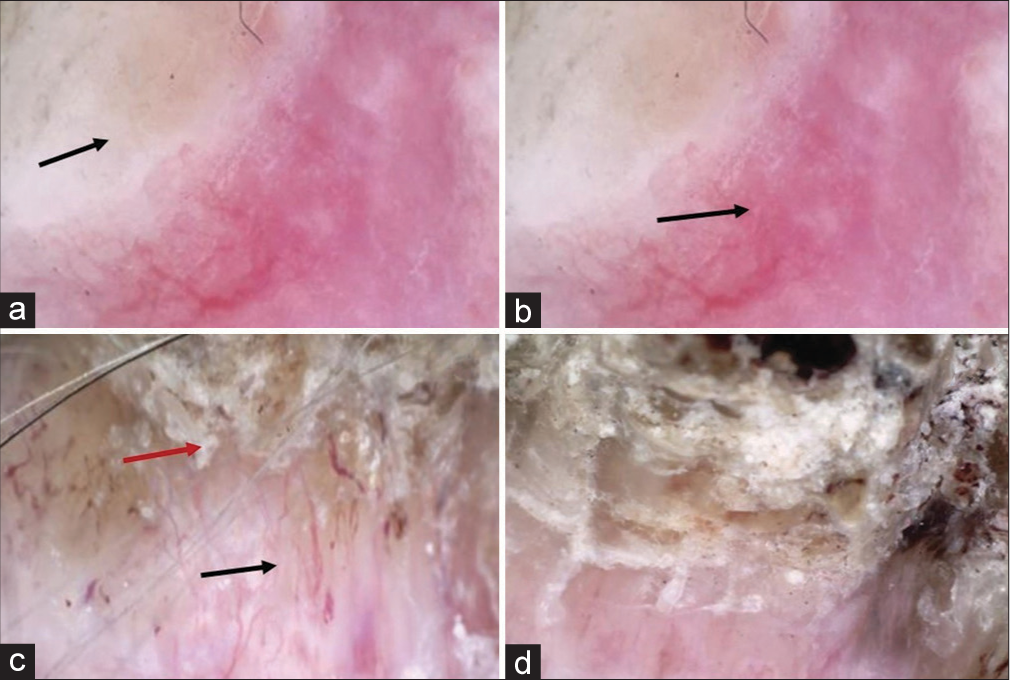
- (a) Dermoscopy of horn base showing structureless white areas (black arrow), (b) erythema (black arrow), (c)arborizing vessels (black arrow), and scaling (red arrow). (d) Dermoscopy of lateral surface of horn with absence of terrace pattern. (DermLite DL3, 10×, polarized).
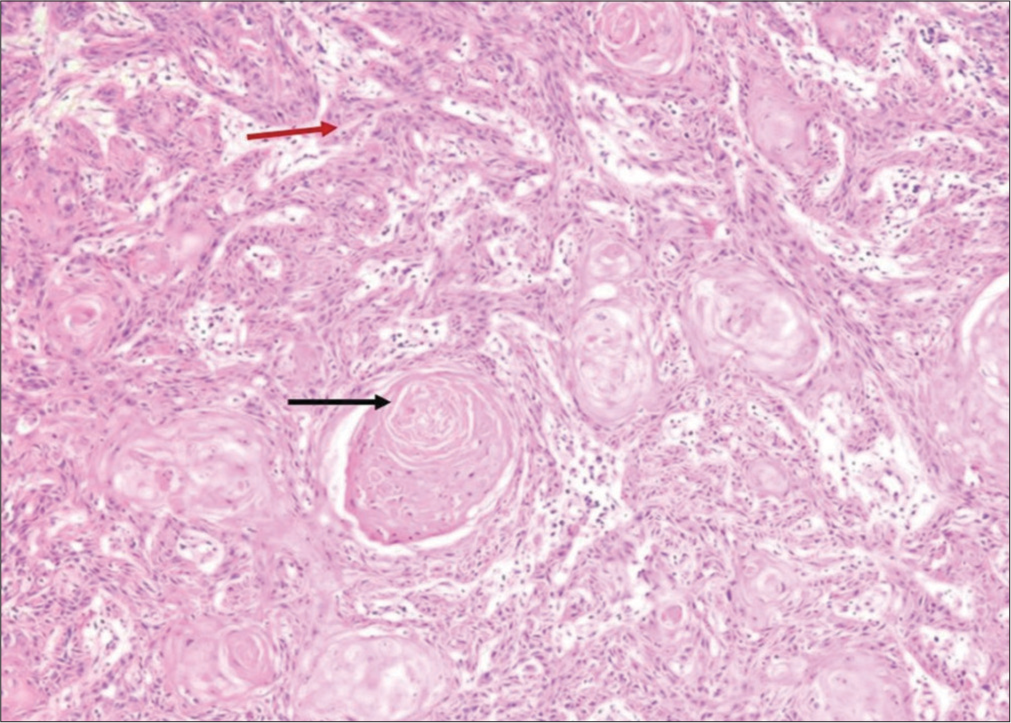
- Histopathology showing well-delineated nests of tumor cells infiltrating the whole dermis with multiple keratin pearls (black arrow). The squamous cells are polyhedral with vesicular nucleus, abundant eosinophilic cytoplasm, and prominent intercellular bridges (red arrow) (H&E, 100×). H&E = hematoxylin and eosin.
DISCUSSION
Cutaneous horns are reactive cutaneous growths comprising of compact dead keratin arising from the basal keratinocytes.1 They are generally solitary, well- circumscribed lesions, frequently seen between 60 to 80 years of age.1 Photo-exposed and chronic sun-damaged sites such as head, dorsum of hands, and forearms are the favored sites. Cutaneous horn can arise from a variety of benign (seborrheic and lichenoid keratoses, human papillomavirus infection, molluscum, chronic irritation, hemangioma, sarcoidosis, juvenile xanthogranuloma, epidermal nevus, angiokeratoma, trichilemmoma, and sebaceous adenoma), premalignant (arsenical keratosis, micaceous balanitis, actinic keratosis, Bowen’s disease, and keratoacanthoma), and malignant (verrucous carcinoma, basal cell carcinoma, Kaposi’s sarcoma, and malignant melanoma) skin lesions.1
Cutaneous horn has a height of more than half the diameter of its base and is generally diagnosed clinically. The horn projection can be conical, cylindrical, pointed, or curved, whereas the base can be flat, nodular, or crateriform.1 Histopathology of the base is necessary to know the underlying pathology, which can be benign in 61.1%, premalignant in 23.2%, and malignant in 15.7% of cases.2 SCC has been found in 94% of cutaneous horns with malignant base. Male gender, advanced age, rapid growth, wider horn base, and photo-exposed sites are associated with premalignant and malignant pathology.3 Horn base erythema, pain, height of horn less than the diameter of base, and absence of terrace morphology (orderly structured horizontal contours on side of horn) on dermoscopy are reportedly markers for invasive SCC.4
DLE is characterized by well-demarcated plaques, often localized to the head and neck region, which heal with atrophy, scarring, and depigmentation. Only a small subset has disseminated lesions. DLE has been rarely associated with cutaneous horn and we could find only three such case reports in English literature [Table 1].2,5,6 However, none of these patients had an underlying malignancy. Malignant transformation in DLE is rare and can range from SCC and basal cell carcinoma to malignant fibrous histiocytoma and atypical fibroxanthoma.7 Malignant transformation in DLE to SCC has been reported in only 0.98%–6.9% of cases.8 The duration between DLE and SCC varies between 4 and 20 years. It commonly arises on photo-exposed and heavily scarred areas of face, scalp, and forearm.9 Chronic ultraviolet radiation exposure is the most important risk factor for SCC and most of the DLE-associated SCC develop in depigmented lesions on sun-exposed areas. Other predisposing factors include age more than 40 years, male gender, chronic scarring, human papillomavirus infection, and long-term immunosuppressive therapy.9 Persistent lesional local inflammation and subsequent scarring, depigmentation, and atrophy seen in DLE might lead to increased risk for SCCs in these patients.9
| Author, year | Age/gender | Duration of DLE | Site | Size | Histopathology of base |
|---|---|---|---|---|---|
| Dabski and Stoll,5 1985 | 38 years/M | 7 years | Nose | 3 × 4 cm | DLE |
| Fatani et al.,2 2014 | 28 years/F | – | Scalp | 8 × 2× 2 cm | DLE |
| Chowdhury et al.,6 2014 | 9 years/M | 3 years | Multiple, all over body except palms and soles | 3 mm–2 cm in height | DLE |
| Present case | 60 years/F | 15 years | Scalp | 6 × 6 × 3 cm | SCC |
DLE: Discoid lupus erythematosus, F: Female, M: Male, SCC: Squamous cell carcinoma
Our patient was an elderly female with a chronic depigmented scarred lesion on the scalp for over 15 years, which might have predisposed her for SCC.
Management of the cutaneous horn depends on the underlying primary pathology. Wide local excision is the treatment of choice, with preservation of margins for histological evaluation.1 The patients should be adequately followed up for recurrence and/or metastasis.
CONCLUSION
This case highlights the importance of the histopathological examination of the base of cutaneous horn and to have a high degree of suspicion for malignant change in DLE, especially in long-standing untreated lesions.
Authors’ Contributions
All the authors contributed to the research study. Kavita Bisherwal dealt with Definition of intellectual content. Archana Singal became the Guarantor. Kavita Bisherwal and Archana Singal: Concecepts, Design, Literature research, Data Acquisition, Data analysis, Manuscript preparation, Manuscript editing, Manuscript Review. Anil Kumar Bhoi and Sonal Sharma: Literature research, Data Acquisition, Manuscript preparation, Manuscript editing.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Cutaneous horn In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563280/
- [Google Scholar]
- Cutaneous horn arising from an area of discoid lupus erythematosus on the scalp. BMJ Case Rep. 2014;2014:bcr2013202322.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous horns: Clues to invasive squamous cell carcinoma being present in the horn base. Dermatol Pract Concept. 2013;3:3-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous horn arising in chronic discoid lupus erythematosus. Arch Dermatol. 1985;121:837-8.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple cutaneous horns due to discoid lupus erythematosus. Indian J Dermatol Venereol Leprol. 2014;80:461-2.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple squamous cell carcinomas arising in lesions of discoid lupus erythematosus. J Dermatol. 2004;31:73-5.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant potential of oral and labial chronic discoid lupus erythematosus: A clinicopathological study of 87 cases. Histopathology. 2011;59:292-8.
- [CrossRef] [PubMed] [Google Scholar]
- Discoid lupus erythematosus with squamous cell carcinoma: A case report and review of the literature in Indian patients. Lupus. 2015;24:1562-6.
- [CrossRef] [PubMed] [Google Scholar]






