Translate this page into:
Descending the reconstructive ladder: Salvage reconstruction by tissue expansion to revise a free flap-based forehead reconstruction
*Corresponding author: Christian M. Asher, Department of Plastic and Reconstructive Surgery, Addenbrooke’s Hospital, Cambridge University Hospitals NHS Foundation Trust, Cambridge, UK. christianasher@doctors.org.uk
-
Received: ,
Accepted: ,
How to cite this article: Asher CM, Oluboyede D, Mario AI, Malata CM. Descending the reconstructive ladder: Salvage reconstruction by tissue expansion to revise a free flap-based forehead reconstruction. J Cutan Aesthet Surg. 2025;18:123-6. doi: 10.4103/JCAS.JCAS_201_22
Abstract
Forehead defects pose a reconstructive challenge and multiple revisions are often required to achieve satisfactory outcomes. The case history of a 20-year-old woman undergoing radical resection of a forehead arteriovenous malformation and reconstruction with an anterolateral (ALT) free flap is described. Although free tissue transfer with an ALT was successful, its color and texture mismatch were unacceptable to the patient. The esthetic result and patient satisfaction were improved by subsequent tissue expansion of the contralateral forehead, removal of the free flap and advancement of the contralateral forehead skin. Complex reconstructions utilize a breadth of techniques. We illustrate a dynamic use of the reconstructive ladder, implementing a descending approach to achieve a satisfactory reconstruction objectively and subjectively from the patient perspective.
Keywords
Anterolateral thigh free flap
Arteriovenous malformation
Facial reconstruction
Free flap complications
Reconstructive ladder
Tissue expansion
INTRODUCTION
The forehead is one of the major esthetic subunits of the face, the entirety of which should be considered to ensure optimal outcomes.1,2 Reconstructing extensive, composite defects of the forehead after tumor ablation, trauma, infection, congenital defects or burns is challenging. Patient satisfaction is significantly less with forehead reconstruction compared to other craniofacial reconstructions.3 There is no consensus on the best approach and limited literature directed at improving patient-reported outcomes in forehead reconstruction.
We illustrate how the atypical approach of descent through the reconstructive ladder offered an aesthetically acceptable outcome to both patient and clinician.
CASE REPORT
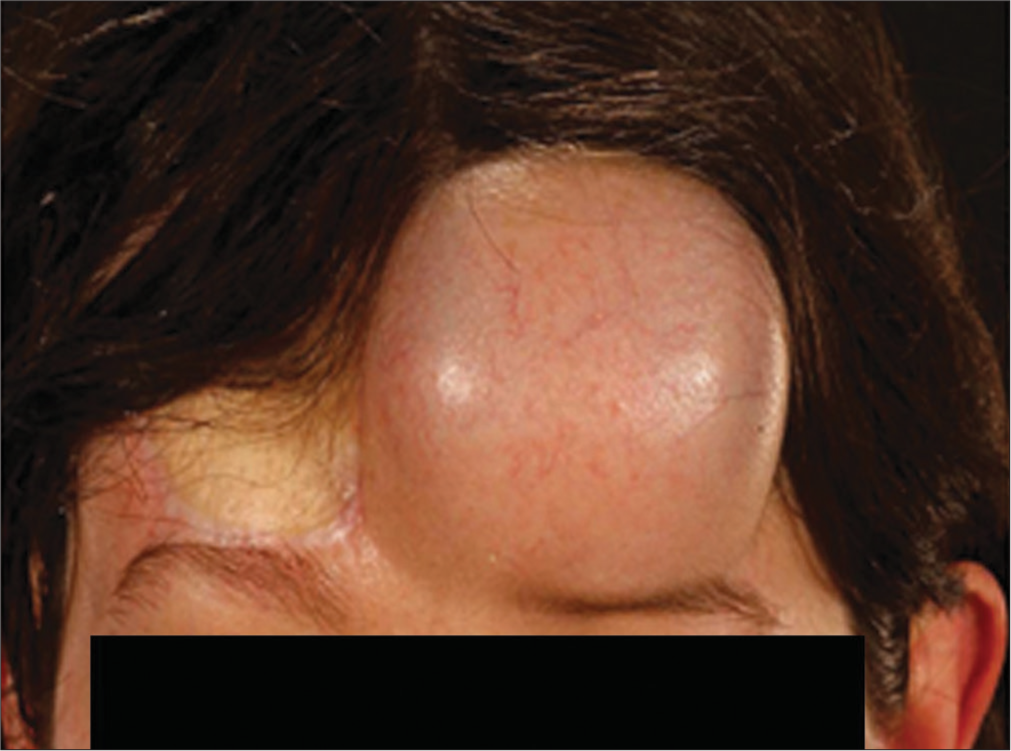
A 20-year-old was referred by the Neurosurgery Service to the Plastic Surgery Department for immediate reconstruction following Osteocutaneous resection of a recurrent arteriovenous malformation (AVM) of the forehead [Figure 1].

- Preoperative photograph showing the irregular 4 × 8 cm arteriovenous malformation (AVM) on the patient’s forehead, extending from the right brow into the frontal hairline.
Two years previously, she underwent resection of the AVM via a bicoronal approach with preservation of the overlying skin in another hospital. She developed a laser resistant recurrence angiographically unamenable to therapeutic embolization. Because of persistent ipsilateral headaches, with localized topical pain associated with the AVM, a decision was made to widely resect the lesion and underlying bone, eliminating any diploic connections.
The AVM was resected in a combined approach with the neurosurgeons and maxillofacial surgeons with simultaneous elevation of an anterolateral thigh (ALT) free flap by plastic surgeons. The underlying bone was hyperostotic with no visible connections to the AVM. The frontal bone was tangentially resected, leaving a shelf of inner cortical bone. The frontal sinus was inadvertently breached and therefore obliterated by mucosal stripping, packing with fat and ostium occluded with bone wax prior to reconstruction.
A chimeric ALT was harvested from the right thigh in the standard fashion with vastus lateralis muscle and inset into the defect. A small split thickness skin graft (SSG) was used to cover the vastus lateralis muscle over the vascular pedicle to prevent tight wound closure and compression of the pedicle. Her postoperative course was uneventful [Figure 2].

- (a) Early postoperative image of the flap prior to revisional surgery. The skin graft is visible lateral to the skin paddle. (b) Following revision to reduce bulk and excise the split thickness skin graft (SSG). Lateral postoperative appearance showing no contour deformity. (c) Magnified view of the flap illustrating the color and texture mismatch.
After two months, she underwent revision surgery to debulk the reconstruction and excise the SSG overlying the vascular pedicle [Figure 2]. Despite a satisfactory contour [Figure 2a], she was unhappy with the color mismatch to neighboring skin and the distribution of hair growth [Figure 2b]. Tissue expansion with a 100 mL, 4 × 4 cm rectangular tissue expander (Nagor TCR 100, Nagor UK Ltd, Isle of Man) to the left forehead was pursued with instillation of 53 mL over 8 weeks [Figure 3] followed by excision of the ALT and resurfacing the defect with expanded skin of the adjacent forehead at 4 months [Figure 4].
- Maximally inflated expander prior to resection of the anterolateral thigh (ALT).

- (a) At 6-month follow-up following excision of the anterolateral thigh (ALT) and inset of expanded contralateral skin of the forehead. There is an improved color and texture match. (b) A lateral view illustrating good contour with a preserved hairline and brow position.
DISCUSSION
The reconstructive ladder aides the reconstructive approach,4,5 is typically used in an escalating sequence, and the next step will be more extensive than the former.
Local flaps provide an ideal color and texture match; however, there are limited options for forehead defects.4-6 In this case, they were precluded by the size and volume of the expectant composite defect. Tissue expansion has been described successfully in facial reconstruction where skin color and texture match are important, but it was unsuitable for reconstructing an Osteocutaneous defect primarily.1,4,7 A free flap-based reconstruction was therefore the next most appropriate option.
There are no “ideal” free flaps for forehead defects. Those typically used vary in composition and texture, and include the radial forearm, groin, parascapular, ALT, latissimus dorsi (LD), and rectus abdominis flaps.2,4,5 Parascapular and LD provide good color match but prevent simultaneous resection and flap harvest. The radial forearm is a versatile and reliable flap, quick to harvest, thin, and pliable. It did not offer enough substance for the planned contour defect created by the composite resection and the patient objected to the likely color mismatch and readily visible donor site scarring. A rectus abdominis flap in a 22-year- old was unfavorable due to associated morbidity with rectus muscle harvest. The ALT offered a robust, reliable reconstruction, capable of filling an extensive defect and would allow simultaneous resection and harvest, while providing a relatively well-concealed donor site.
Inadequate color match, contour, bulkiness, and unwanted hair growth are described as aesthetic pitfalls in facial reconstruction.2,5,8 Revision procedures to enhance the aesthetic outcome of these reconstructions, particularly with free tissue transfer, is common practice. This includes scar revision, contouring procedures through fat transfer, liposuction, and debulking excision.1,2,8 Dermabrasion, epilation procedures, and laser may also have their uses.
The initial revision surgery improved the contour of the flap, but the patient was still dissatisfied. The ALT skin behaved in keeping with tissue originating from the thigh, exposed to more ultraviolet (UV) light on the face, in addition to its pattern of hair distribution mirroring its origin. The pathogenesis of the peau d’orange appearance in the flap is unclear and may be related to changes in vascularity following tissue transfer. Interference with lymphatic drainage could have conceivably been caused by a subclinical infection from the exposed neighboring skin grafted area over the pedicle. In the senior author’s experience, this problem has not been previously encountered.9
The quest for aesthetic excellence in flap-based reconstructive surgery is not new. Millard urged that the ultimate goal should not just be average normal but rather, if possible, the ideal beautiful normal (eighth principle).10 To aesthetically salvage this patient’s forehead reconstruction and improve her satisfaction, we modified our use to the traditional approach, descending down the reconstructive ladder using tissue expansion to deliver a patient-centered outcome [Figure 5].
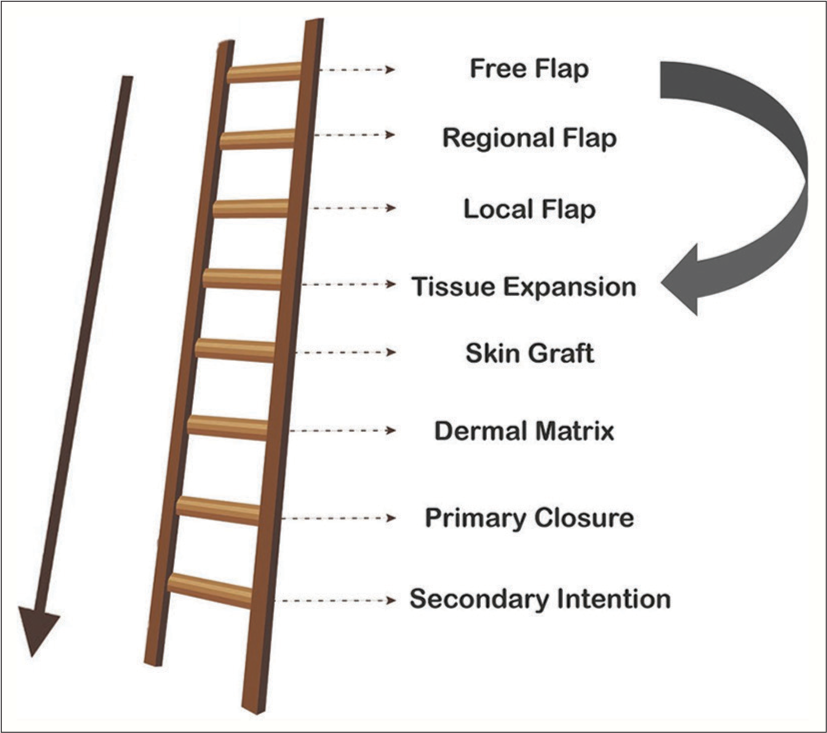
- The reconstructive ladder illustrating our implementation of a descending approach to achieve a satisfactory reconstruction.
CONCLUSION
The reconstructive ladder is a guiding framework. Within cosmetically sensitive regions, a dynamic approach is necessary to heighten the aesthetic outcome and meet patient expectations. An ascending approach, and in the context of salvage reconstruction, a descending approach both offer a modern and flexible perspective to reconstructive surgery.
Acknowledgment
This work was supported by the NIHR Cambridge Biomedical Research Centre.
Authors’ Contributions
All the authors contributed to the research study. Christian M. Asher: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review. Daniel Oluboyede: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review. Avelina I. Mario: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review. Charles M. Malata: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Forehead reconstruction with microvascular flaps: Utility of aesthetic subunits. J Reconstr Microsurg. 2012;28:319-26.
- [CrossRef] [PubMed] [Google Scholar]
- The fusion of craniofacial reconstruction and microsurgery: A functional and aesthetic approach. Plast Reconstr Surg. 2014;134:760-9.
- [CrossRef] [PubMed] [Google Scholar]
- Aesthetic and oncologic outcome after microsurgical reconstruction of complex scalp and forehead defects after malignant tumor resection: An algorithm for treatment. Plast Reconstr Surg. 2010;126:460-70.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstruction of the forehead and scalp. Facial Plast Surg Clin N Am. 2019;27:85-94.
- [CrossRef] [PubMed] [Google Scholar]
- Scalp and forehead reconstruction. Semin Plast Surg. 2018;32:90-4.
- [CrossRef] [PubMed] [Google Scholar]
- Achievements in scalp reconstruction. Curr Opin Otolaryngol Head Neck Surg. 2014;22:127-30.
- [CrossRef] [PubMed] [Google Scholar]
- Systematic review of tissue expansion: Utilization in non-breast applications. Plast Reconstr Surg Glob Open. 2021;9:e3378.
- [CrossRef] [PubMed] [Google Scholar]
- Microsurgical forehead reconstruction: An aesthetic approach. Plast Reconstr Surg. 1995;95:647-51.
- [CrossRef] [PubMed] [Google Scholar]
- Versatility of the anterolateral thigh free flap: The four seasons flap. Eplasty. 2012;12:e21.
- [Google Scholar]






