Translate this page into:
Disposable circumcision suture device: A potential bedside tool for circumcision – A series of 18 cases
*Corresponding author: Yogesh M. Bhingradia, Department of Dermatology, Venereology and Leprosy, Shivani Skin Care and Cosmetic Clinic, Surat, Gujarat, India. yogeshbhingradia@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhingradia YM, Priya D, Pawar SB, Muthukumarasamy V, JP P. Disposable circumcision suture device: A potential bedside tool for circumcision – A series of 18 cases. J Cutan Aesthet Surg. doi: 10.25259/jcas_140_23
Abstract
Male circumcision (MC) is a well-established surgical procedure with a long history. It offers various health benefits, including protection against infections and diseases. The disposable circumcision suture device (DCSD) helps in faster wound healing which will result in reduced complications compared to other conventional circumcision methods. In this report, we share our experience with the stapler method in MC for various dermatological indications. The study emphasized the significance of circumcision in dermatological applications and its potential impact on clinical practice.
Keywords
Disposable circumcision suture device
Stapler circumcision device
Genital diseases
INTRODUCTION
Male circumcision (MC) is a surgical procedure that holds the distinction of being one of the oldest known surgeries in human history.1 In addition to promoting hygiene, this procedure plays a crucial role in protecting against various infections, including human papillomavirus, genital herpes, human immunodeficiency virus (HIV), and penile cancers.2
There are three frequently used surgical techniques for MC: The dorsal slit, the forceps-guided method, and the sleeve resection technique.3 The most common complications associated with these methods include peri/post-operative pain, bleeding, and infection.4
Recently, a circular stapler device is introduced to perform circumcisions.5 The disposable circumcision suture device (DCSD) is available in nine different models, each designed to accommodate various penile girths, including 10, 12, 14, 16, 18, 22, 26, 30, 32, and 34.6 In this report, we present our experience with the DCSD method of MC, which was performed on 18 patients with different genitalia related diseases. We thoroughly analyzed the perioperative and post-operative outcomes as well as complications associated with this method.
It is worth mentioning that the existing literature lacks similar studies specifically focusing on the dermatological applications of circumcision and the potential benefits that it can offer in our clinical management.
Material and methods
The study involved a retrospective analysis of MC cases which were performed in a private clinic in urban Gujarat between 2020 and 2023. All patients underwent routine blood investigations and written informed consent was obtained before the start of the procedure.
Procedure
Appropriate device size selected based on penile circumference using a stencil
Penis and surrounding area cleaned with betadine and spirit
Local anesthesia (2% lidocaine) infiltrated for ring block at penis base
Adjusting knob opened, inner ring removed
Foreskin stretched, inner bell inserted over glans
Dorsal slit given in phimosis/paraphimosis cases for easy passage
Plastic cable tie used to tie prepuce over inner bell shaft [Figure 1a]
Prepuce length assessed and adjusted; redundant length cut off
Outer bell placed over inner bell, adjusting knob tightened
The safety bolt was removed and trigger handle pressed for 1 min [Figure 1b]
Adjusting knob opened, outer bell removed, followed by inner bell [Figure 1c]
Ring secured at incision line for hemostasis [Figure 1d]
The dressing was applied with mupirocin ointment and self-adhesive tapes.

- (a) Clamping of foreskin after creating a dorsal slit (b) An outer bell is inserted and the trigger is pushed to perform cutting of excess foreskin, (c) Excess foreskin removed, (d) Post-circumcision appearance of penis, and (e) Appearance of penis two months post procedure.
Patients were prescribed oral antibiotics for 5 days, along with analgesics and topical antibacterial agents. Dressings were recommended every alternate day for a week. Subsequently, follow-up visits were scheduled every 2 weeks for 2 months.
CASE SERIES
The cases comprised 18 male patients aged between 20 and 60 years, with an average age of 40.44 years. Among the 18 patients, three had diabetes, and one had hypertension. The procedures were performed for various conditions, including phimosis (2), paraphimosis (5), lichen sclerosus atrophicus (3), condyloma acuminata (2), and recurrent candidal balanitis (6). The most common conditions observed were paraphimosis and recurrent candida balanitis. The time taken to perform the procedure was 15–20 min.
Complications observed in the study included edema in two patients. However, there were no instances of instrument malfunction, infection, hematoma, or scarring/adhesions observed in the patients. Bleeding was almost nil throughout the procedure and post-procedure. Wound healing time was documented to be 7–10 days post-procedure during when there was self-dislodgement of staplers.
DISCUSSION
Circumcision is the removal of foreskin and is frequently performed for various medical indications. Recently, the procedure has gained more importance due to its protection against HIV infection by reducing HIV receptors over the foreskin.7
In our analysis, we observed that the total time required to complete the DCSD technique was shorter compared to other conventional methods. This is particularly important for dermatologists who have a busy daily practice, as it helps save valuable time. In addition, the DCSD method resulted in minimal blood loss during and after the procedure. Patients who underwent the DCSD method experienced less pain post-procedure. This finding is supported by two meta-analysis studies performed by Fan, et al., and Huo, et al.8,9 One of the key advantages of the DCSD method was its notably shorter healing time. Since the device comes in a pre-sterilized disposable kit, the occurrence of post-operative infections and other complications is less frequent. The study observed that the only complication present was edema. However, it was resolved within 2 weeks following the procedure.
Conventional methods of circumcision have numerous disadvantages. The extended period required to acquire the skills to perform procedure poses a challenge in resource limited environments. The occurrence of complications like wound dehiscence, which is often observed with other methods, is less frequent with DCSD. However, it is essential to assess these factors through well-designed larger trials. Due to the absence of suturing, the DCSD does not result in a nodular appearance at the incision lines in the post-operative phase. The procedure results in a smooth incision line on healing [Figure 1e].
In addition to its efficacy in treating dermatological genital diseases, DCSD [Figure 2] also plays a role in the prevention of various sexually transmitted infections and recurrent infections associated with coexisting medical conditions. The primary drawback of DCSD lies in its high cost which limits its utilization in resource-limited areas.
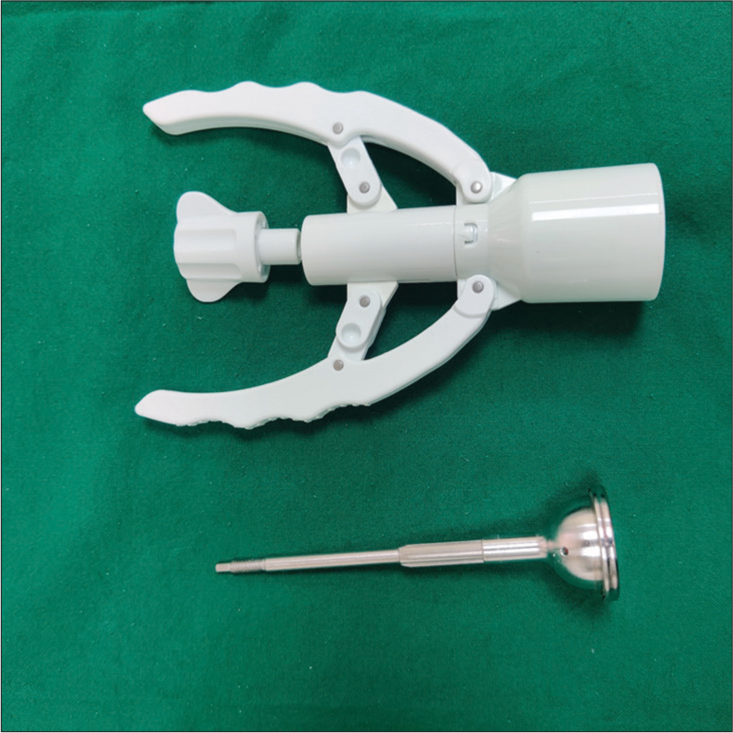
- Circumcision stapler device designed for single use.
The lack of available literature on the application of circumcision procedures in the field of dermatology has motivated this study, as we seek to explore the significant role that it can play in the daily practice of dermatologists.
CONCLUSION
The benefits of disposable circular staplers, including reduced operative time, improved wound healing, and lower complication rates, make them a preferred choice in circumcision procedures. However, further research is needed to validate these findings and explore the long-term outcomes associated with disposable circular staplers. As technology continues to advance, it is crucial to embrace innovative approaches that enhance the safety, efficiency, and patient satisfaction in surgical interventions like circumcision.
Authors’ contributions
Yogesh M. Bhingradia: Concept and design of study, Critical feedback, Drafting of the article, Final Approval. Devi Priya S: Data acquisition, Analysis, Image editing, Drafting of article, Final approval. Smit B. Pawar- Data Acquisition, Analysis, Final approval. Vivek Muthukumarasamy - Data acquisition, Critical feedback, Final approval. Pratibha J P: Critical feedback, Drafting of article, Final approval.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- History of circumcision: A religious obligation or a medical necessity. J Nephrol. 2011;24(Suppl 17):S100-2.
- [CrossRef] [Google Scholar]
- Male circumcision: Towards a World Health Organisation normative practice in resource limited settings. Asian J Androl. 2010;12:628-38.
- [CrossRef] [Google Scholar]
- Complications of circumcision in male neonates, infants and children: A systematic review. BMC Urol. 2010;10:2.
- [CrossRef] [Google Scholar]
- Adult male circumcision with a circular stapler versus conventional circumcision: A prospective randomized clinical trial. Braz J Med Biol Res. 2015;48:577-82.
- [CrossRef] [Google Scholar]
- A retrospective taiwanese-population-based clinical study on determining the efficacy and safety of disposable circumcision anastomat. J Clin Med. 2022;11:6206.
- [CrossRef] [Google Scholar]
- Abundant expression of HIV target cells and C-type lectin receptors in the foreskin tissue of young Kenyan men. Am J Pathol. 2010;176:2798-05.
- [CrossRef] [Google Scholar]
- The characteristics of circular disposable devices and in situ devices for optimizing male circumcision: A network meta-analysis. Sci Rep. 2016;6:25514.
- [CrossRef] [Google Scholar]
- Use of a disposable circumcision suture device versus conventional circumcision: A systematic review and meta-analysis. Asian J Androl. 2017;19:362-7.
- [CrossRef] [Google Scholar]







