Translate this page into:
Efficacy and safety of diode laser for facial hair reduction in hirsutism—a clinico-trichoscopic evaluation
Address for correspondence: Dr. Anil Budania, AIIMS Faculty Quarters, AIIMS, Jodhpur 342005, Rajasthan, India. E-mail: anilbuddy25@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Hirsutism is the presence of excessive terminal hair on androgen-dependent sites of the body. Lasers like Alexandrite, diode, and Nd:Yag lasers have been used for hair reduction with varying efficacy. Trichoscopy of hair is a simple noninvasive method of hair assessment. However, it has not been used in the assessment of diode laser hair reduction.
Objectives:
This study aimed to assess the efficacy and safety of diode laser hair reduction in skin color with the help of clinical and trichoscopic assessment.
Materials and Methods:
This prospective observational study included 73 patients of hirsutism recruited in 18-month period. All participants received sessions of 805 nm diode laser at monthly intervals up to six sessions. Clinical and trichoscopic evaluation along with photographs were obtained at each visit. Side effects, if any, were noted in every sitting.
Results:
All patients were females of Fitzpatrick skin types III–V. All clinical parameters showed statistically significant hair reduction when compared with baseline. Trichoscopic parameters of hair reduction like total hair count, terminal hair count, and terminal/vellus hair ratio showed reduction compared to baseline which was statistically significant (P < 0.05). The most common side effect noted in our study was pain followed by erythema and perifollicular edema.
Conclusions:
Diode laser is an effective and safe procedure for the reduction of unwanted facial hair, even in darker skin types. We also wish to emphasize that trichoscopy for the assessment of laser hair reduction is a recent, noninvasive, simple, and underutilized tool. No serious adverse events were noted in our study.
Keywords
Diode laser
laser hair reduction
trichoscopy
INTRODUCTION
Hirsutism is the presence of excessive terminal hair in androgen-dependent areas. It affects 5%–15% of reproductive-age group females. It can be classified into two types: androgen-induced and non-androgen-induced. Polycystic ovarian disease (PCOD) is the most common cause of androgen-induced hirsutism whereas idiopathic type is the most common cause of non-androgen-induced hirsutism.[1]
Commonly used methods to treat excessive facial hair include hormonal treatment, temporary physical methods of hair removal, and device-assisted hair removal like laser hair reduction.[2] Laser and light-based therapies have replaced traditional hair removal treatments because of their superiority in achieving long-term hair reduction. Lasers in the wavelengths of 600–1200 nm, including ruby (694 nm), diode (810 nm), Nd:YAG (1064 nm), alexandrite (755 nm), and intense-pulsed light, are effective in achieving hair reduction.
The efficacy of laser therapy can be assessed by comparing hair reduction from baseline, predominant hair type, and objective measures like hair counting, hair thickness assessment, and terminal to vellus hair ratio. Patient-reported improvement can also be assessed including percentage hair reduction and satisfaction scores.[3]
Adverse effects reported after laser-assisted hair reduction are generally mild and transient. A few of the common cutaneous side effects include pain, immediate erythema, and perifollicular edema. Severe side effects like burns, blistering, dyspigmentation, and permanent scarring may also occur rarely.[4]
Trichoscopy is a method of hair evaluation in hair disorders like alopecia. It uses a dermoscope to get a magnified image of hair and the surrounding skin. Trichoscopy can be used for evaluating the efficacy of lasers by assessing hair density, thickness, type of hair, etc.[56] But studies on trichoscopic assessment of the efficacy of lasers in skin of color are very limited. To the best of our knowledge, this would be the first study to assess diode laser hair reduction using trichoscopy. Moreover, this study might add efficacy and safety data of diode lasers in Indian skin color.
MATERIALS AND METHODS
Study design and subjects
It was a prospective observational study conducted on patients of hirsutism who attended the Dermatology OPD at a tertiary care Centre in Rajasthan during a period of 18 months (January 2020 to June 2021). The study was approved by the Institutional Ethics Review Board. Written informed consent was obtained from all participants prior to enrollment.
Seventy-three female patients with facial hirsutism, skin types III–V, and dark terminal facial hair were included. Females having pregnancy, keloidal tendency, history of skin malignancy, photosensitivity, or active skin infection over the treatment site were excluded from the study.
MATERIALS AND METHODS
Detailed history, examination, hormonal profile, and USG pelvis were done in all patients. Expected outcomes and complications were explained to patients before laser therapy. Patients were instructed to avoid sun exposure and hair removal for 1 month prior to the first treatment and during the study.
After removing hair from the treatment area with a razor, subjects underwent treatment with an 805 nm diode laser (Light Sheer Desire Light Model, Lumenis) using a 12 × 12 mm spot size and pulse duration of 30 ms. The diode laser was started with a fluence of 18–20 J/cm2 in the first session. On subsequent treatments, fluence was increased by 2–4 J/cm2 depending on the subject’s tolerance up to a maximum of 36 J/cm2. Laser shots were given with an overlap of 10%–20% of the surface area of hand piece tip. Mild erythema considered the end-point of the procedure. The treatment was repeated every 4 weeks up to six sessions. Clinical and trichoscopic evaluations along with photographs were obtained at baseline and every visit thereafter. Although our machine had an inbuilt cooling system, ice packs were used pre and post-procedure to minimize pain and swelling. Topical steroid cream was prescribed if excessive erythema, burns, or swelling was seen. The patient was advised to avoid sun exposure after the treatment and they were instructed to use sunscreen with sun protective factor 30 after each session.
Clinical parameters used were modified Ferriman–Gallwey (mFG) score of the face (0–4), percentage reduction (patient-reported), frequency of hair removal, and predominant hair type. Trichoscopy was done using Dermlite DL4 with a magnification of 10×. Trichoscopic parameters included total hair count, terminal hair count, vellus hair count, and terminal/vellus hair ratio (per field) done at four fixed sites including sidelocks, chin, upper lip, and submandibular area. Hair counting was done manually from prints of the photographs. Side effects if any are noted in every sitting and treated accordingly.
Statistical analysis
Data were entered in an Excel sheet and analyzed using Statistical Package for Social Sciences version 25. All quantitative variables were estimated using measures of central tendency (mean and median). Descriptive analysis was done for patient demographics, clinical, and side effects. As the data was not normally distributed, Friedman’s Test was done to compare trichoscopy and clinical parameters like mFG score. P < 0.05 were considered significant.
RESULTS
All the patients were females with facial hirsutism with ages ranging from 18 years to 43 years with a mean of 26.37 ± 5.825 years. The mean total duration of hirsutism was 4.08 ± 2.83 years. The frequency of hair removal (variable hair removal methods like shaving, tweezing, and threading) ranged from 0 to 60 days with a mean of 14.85 ± 13.33 days. Few patients received treatments (31.5%) including oral medications (20.5%), and lasers (16.4%). Some of them had to continue oral drugs (like oral contraceptive pills and spironolactone) in addition to laser (21.9%).
Menstrual cycles were irregular in 44 patients (60.3%) and regular in 29 patients (39.7%). However, Rotterdam’s criteria for PCOD were fulfilled in 41 patients (56.2%). Two patients had comorbidities like diabetes and hypothyroidism. Features of hyperandrogenism like acne, seborrhea, and alopecia were seen in 59 (80.8%) of patients. A family history of hirsutism was present in 19 patients (26%).
The majority of the patients were of Fitzpatrick skin type 4 (45 [61.6%]), followed by type 3 (19 [26%]), and type 5 (8 [11%]). Baseline hair assessment of the patient was done with an mFG score which ranged from 6 to 20 with a maximum number of people falling in the group of mild hirsutism (60 [82.2%]), followed by moderate hirsutism (11 [15.1%]). The most commonly involved sites were the chin followed by the upper lip, submandibular area, and sidelocks. Hormonal profile revealed high total testosterone levels in 8 patients (11%) whereas ultrasound pelvis showed features of PCOD like increased ovarian volume and polycystic ovaries in 23 patients (31.5%).
Though six sessions were planned, not all patients were able to complete follow-up. Fifty-five patients completed three sessions and 25 patients completed all six sessions. mFG score on the face reduced with repeated sessions. The median at the first, third, and sixth sitting are 3, 2, and 1, respectively. The reduction of facial mFG score from baseline was statistically very significant (P < 0.01) [Figure 1]. Also, the proportion of patients having predominantly terminal hair was 86.3%, 69.1%, and 48% at the first, third, and sixth visit, respectively. The reduction in the proportion of patients having terminal hairs compared to baseline was statistically very significant (P value = −0.002). Also, Hair removal frequency reduced from once in 13.16 days at baseline to once in 52.8 at the third visit and once in 69.8 days at the sixth visit. Hair removal frequency reduction from baseline was statistically very significant at the third visit (P < 0.01) and the sixth visit (P < 0.01).
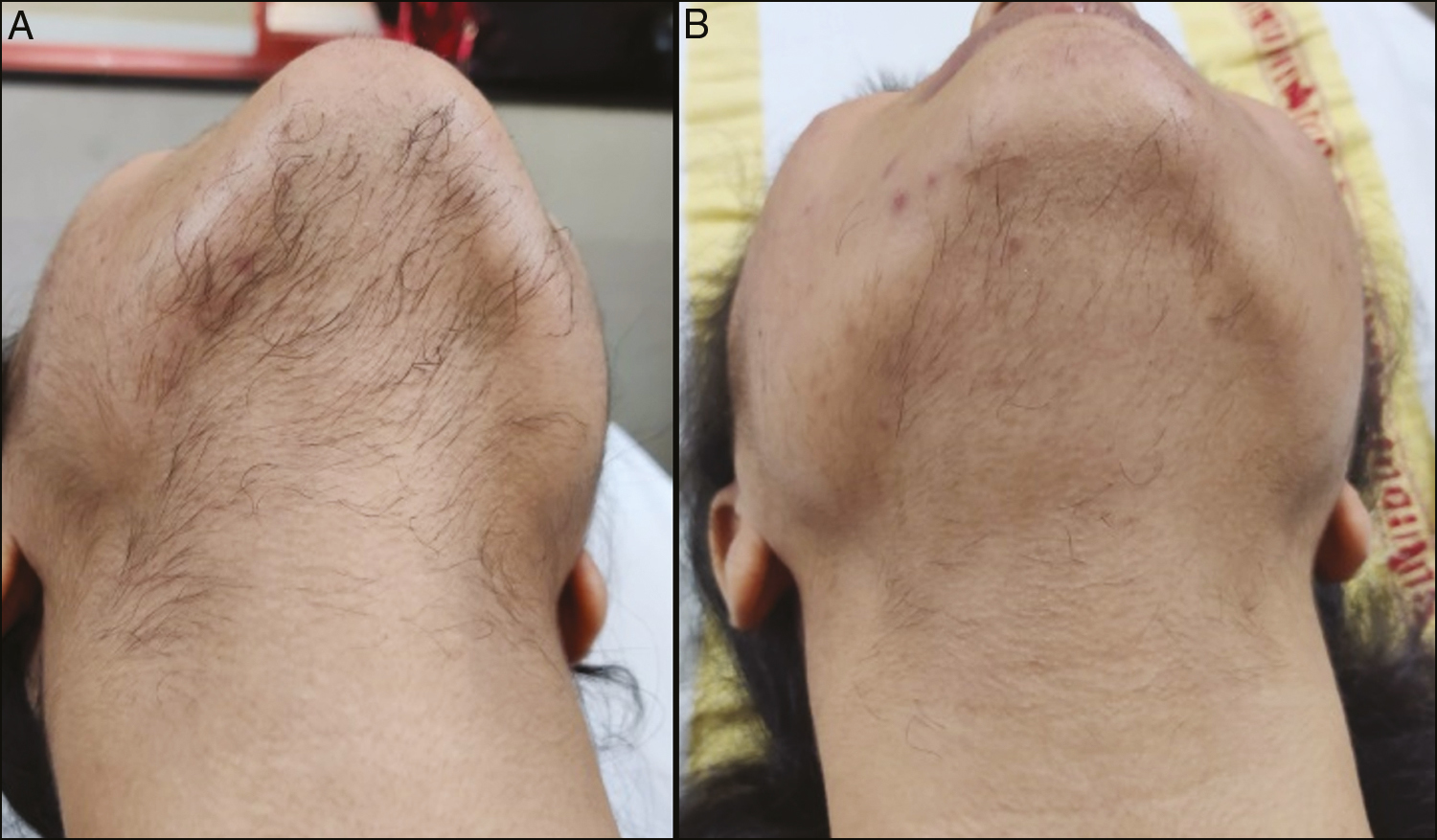
- (A) Facial hair at baseline and (B) after 6 sessions of diode laser
In our study, all trichoscopic parameters like total hair count, terminal hair count, vellus hair count, and terminal/vellus hair ratio were reduced with repeated laser sitting [Figure 2]. The mean total hair count per cm2 at chin at baseline, third, and sixth visit was 38.16, 25.68, and 23.68, respectively. The mean total hair count per cm2 at sidelocks, upper lip, and submandibular area also showed a decreasing trend with repeated visits which was statistically significant. Similarly, the mean terminal hair count at the chin at baseline, third, and sixth visit were 17.48, 9.2, and 5.56, respectively. Reduction in terminal hair count from baseline was statistically very significant in all four areas. Terminal/vellus hair ratio were reduced with repeated laser sittings and was statistically significant in all four areas [Figure 3 and Table 1].
| Sites | Total | Terminal | Vellus | t/v | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (first) | Mean (sixth) | P value | Mean (first) | Mean (sixth) | P value | Mean (first) | Mean (sixth) | P value | Mean (first) | Mean (sixth) | P value | |
| Sidelocks | 39.5 | 25.45 | <0.01 | 12.92 | 4.16 | <0.01 | 25.48 | 21.12 | <0.01 | 0.47 | 0.61 | 0.012 |
| Chin | 38.16 | 23.68 | <0.01 | 17.48 | 5.56 | <0.01 | 20.68 | 17.04 | 0.331 | 0.98 | 0.39 | <0.01 |
| Upper lip | 39.92 | 23.56 | <0.01 | 18.56 | 5.84 | <0.01 | 21.36 | 17.72 | 0.057 | 0.98 | 0.29 | <0.01 |
| Submandibular area | 29.16 | 16.88 | <0.01 | 11.2 | 3.48 | <0.01 | 17.96 | 13.44 | 0.224 | 0.76 | 0.29 | <0.01 |
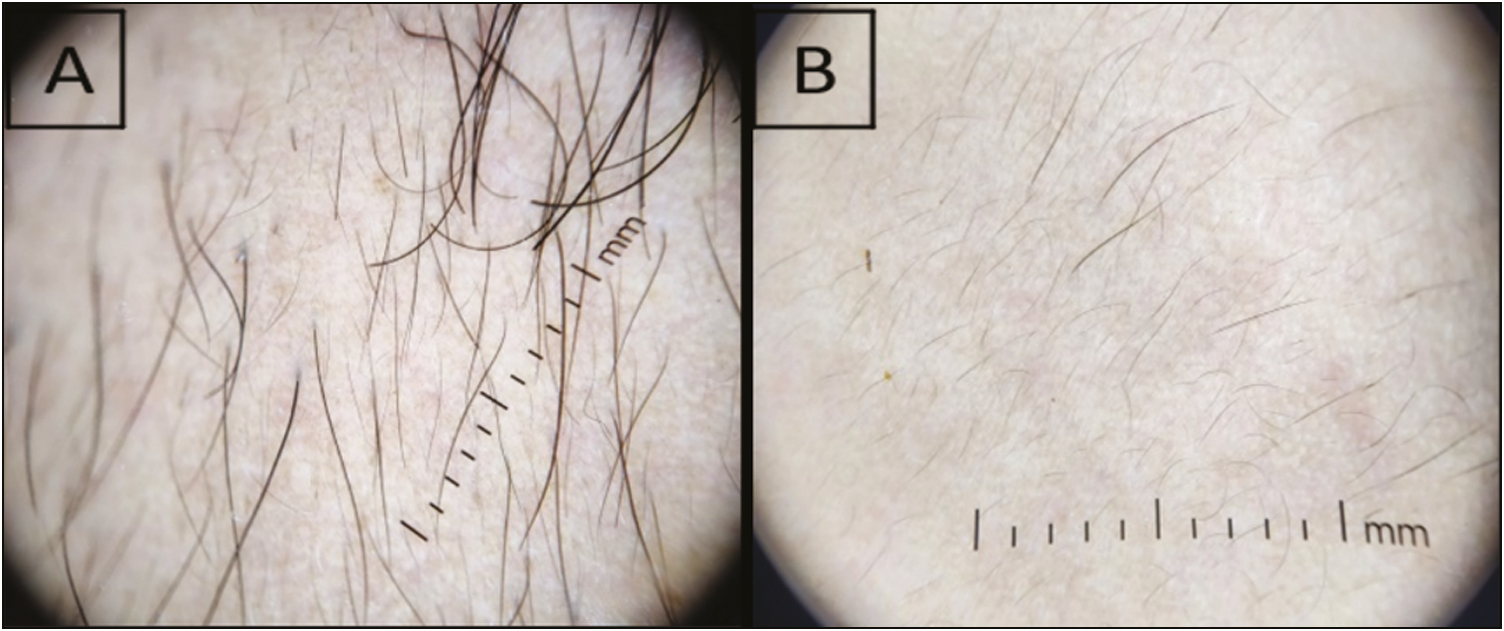
- (A) Trichoscopic assessment of facial hair at baseline and (B) after 6 sessions of diode laser
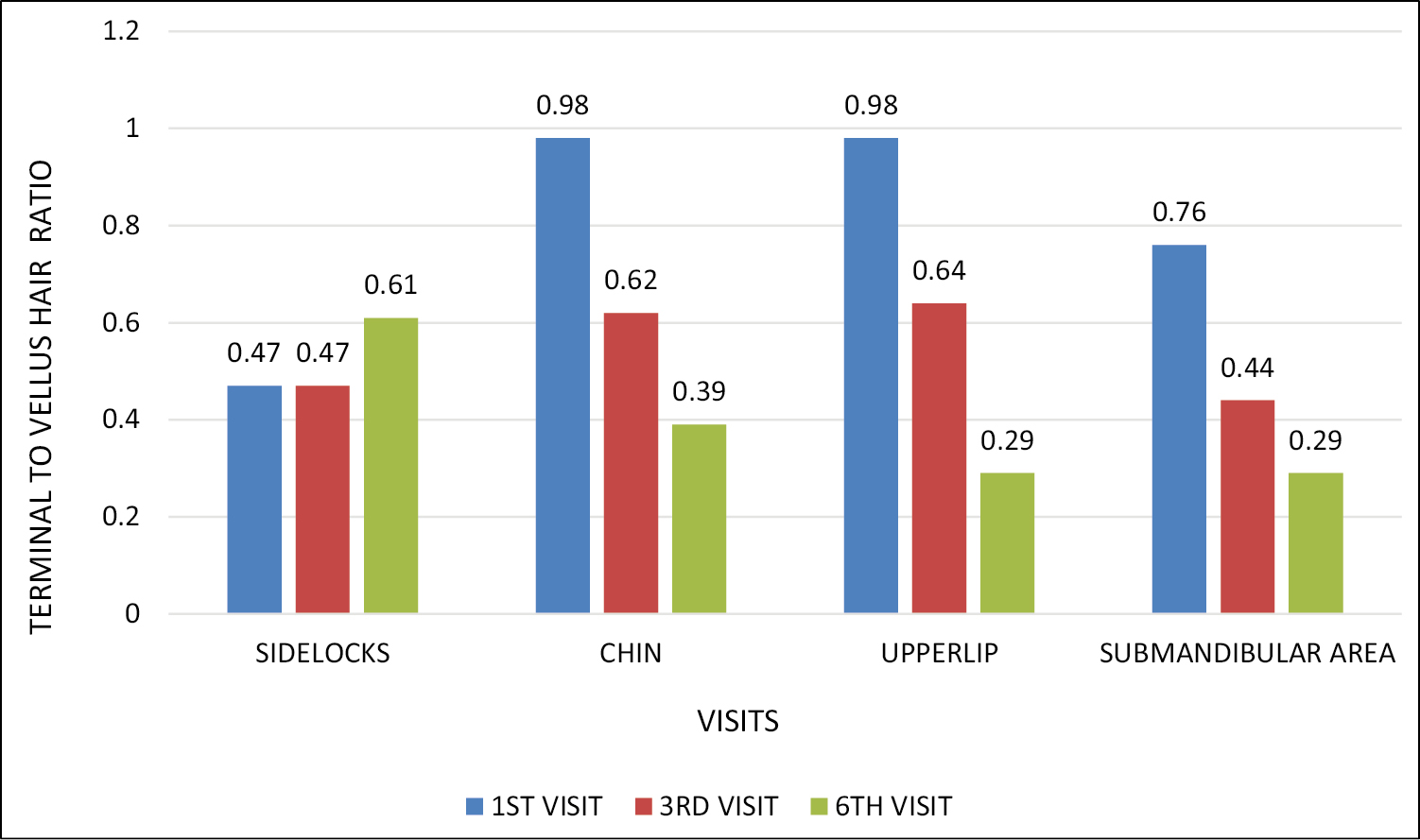
- Comparing terminal/vellus hair count at baseline and at follow-up visits
The most common side effect noted in our study was pain (71 [97.3%]) followed by erythema (65 [89%]) and perifollicular edema (61 [83.6%]). Mild superficial burns (8 [11%]) followed by hyperpigmentation (5 [6.8%]) were noted in a few patients mostly in Fitzpatrick skin types IV and V. Pigmentary changes resolved either spontaneously or with mild depigmenting agents within 1–2 months in all patients. Paradoxical hair growth in the form of multiple small vellus hairs was seen in 2 patients. Acneiform eruption and herpes labialis were seen in 1 patient each [Figure 4].
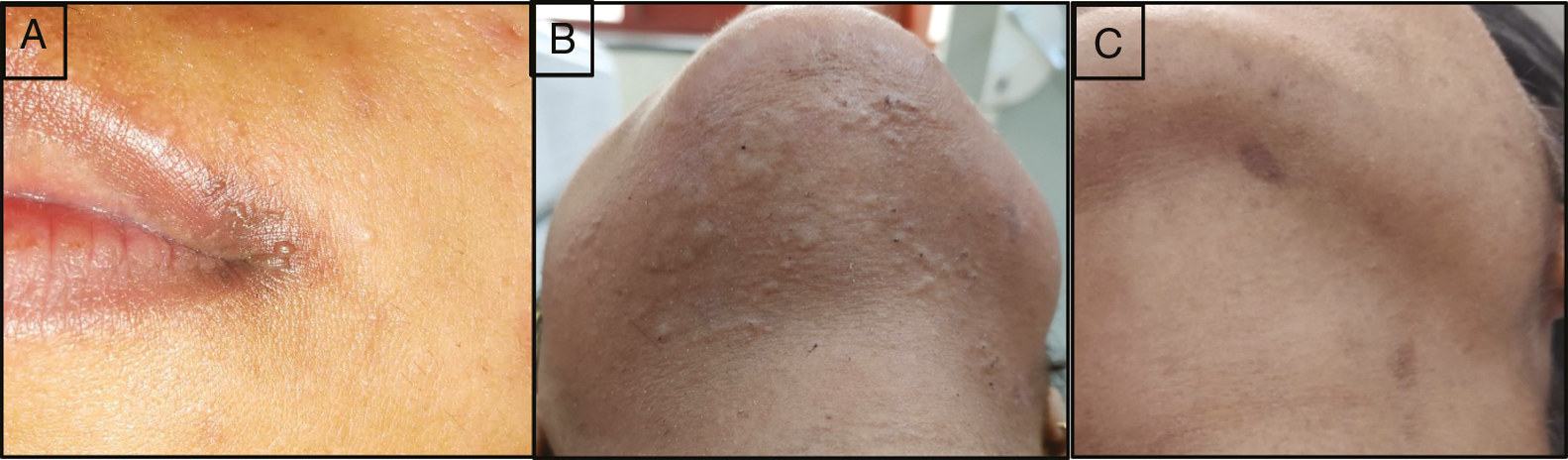
- (A) Adverse effects after laser sessions-herpes labialis, (B) perifollicular edema, and (C) hyperpigmentation
DISCUSSION
About 5%–15% of all women develop some degree of hirsutism.[1] Increased hair growth has a strong negative psychological effect on the well-being of the women. For this reason, various methods of hair removal have been practiced. Multiple lasers and light-based technologies are available for hair removal. Most studies conducted using lasers present decreased efficacy and an increase in side effects in darker-skinned patients.[78] Out of the various laser systems used for hair reduction, longer-wavelength lasers like diode laser penetrate deep into the dermis, thus causing less epidermal absorption and sufficient hair follicle damage.
Dermoscopy of hair is a new, noninvasive, sensitive, specific, and underutilized investigation that can be used for assessing the response of hirsutism to laser hair reduction. The hand-held dermoscope with 10-fold magnification may give an easy and quick evaluation of hair.[6]
In our study, seventy-three patients were recruited for diode laser hair reduction from the Dermatology, Venereology, and Leprology OPD at AIIMS, Jodhpur over a period of 18 months.
Among the 73 patients recruited, most patients had Fitzpatrick skin type IV (61.6%), followed by type III (26%). There were very few studies of lasers on darker skin types due to the increased incidence of adverse events. Few studies like Agarwal et al.,[9] Mustafa et al.,[10] and Adrian et al.[11] have studied the effect of lasers on darker skin types and concluded that lasers can be safely used in darker phenotypes. When compared to previous studies like that of Sadick et al.,[12] which used percentage hair reduction as the primary efficacy parameter, our study used multiple clinical efficacy parameters like facial mFG score, percentage hair reduction, predominant hair type, and frequency of hair removal. This helps in better quantification of clinical response and more objective assessment.
Our study also assessed trichoscopic parameters like total hair count, terminal hair count, vellus hair count, and terminal/vellus hair ratio. They were assessed at four sites including sidelocks, chin, upper lip, and submandibular area. Studies like Mohamed et al.[6] and Nabi et al.[5] used trichoscopic parameters to assess Nd:YAG laser hair reduction. Mohamed et al[6] studied trichoscopic changes in the hair during the treatment of hirsutism with Nd:Yag laser using trichoscan software. Trichoscopy done over the chin showed that total hair count per cm2 at baseline, third, and sixth visit was 73.7, 48.3, and 27.1, respectively. Also, the terminal to vellus hair ratio at baseline, third, and sixth visit was 72.5, 55.1, and 31.8, respectively. Similarly, Nabi et al.[5] did a comparative study of the clinico-trichoscopic response to the treatment of hirsutism with Nd:YAG laser in idiopathic hirsutism and polycystic ovarian syndrome patients. The trichoscopic features were assessed before each laser session, which showed decreased hair shaft thickness, decreased hair shaft color, decreased terminal to vellus hair ratio, and decreased density of hair per cm2 at the chin in both groups with successive sessions.
Our study showed significant trichoscopic reduction of hair in treated areas which can be used as an additional tool for assessing the efficacy of lasers. Multiple trichoscopic parameters were used like total hair count, terminal hair count, vellus hair count, and terminal/vellus hair count helping in objective assessment of the response. Our study would be the first study to assess trichoscopic response to diode laser treatment.
The most common side effect noted in our study was pain (97.3%) followed by erythema (89%) and perifollicular edema (83.6%). They were mild and transient which resolved immediately after the procedure. This was in line with the studies by Jo et al.,[13] Greppi et al.,[14] and Royo et al.[15] Also, mild superficial burns were seen in 8 patients, which later became hyperpigmented in 5 patients. Paradoxical hair growth in the form of multiple small vellus hairs was seen in 2 patients. Acneiform eruption and herpes labialis are seen in one patient each. Similar side effects were noted in studies by Nabi et al.[5] and Royo et al.[15] Although a larger number of side effects are reported with lasers in darker skin types, our study showed that laser therapy can be done safely in the Indian population. Minimal side effects were noted, most of which were mild and transient. Fewer side effects in our study may be due to using appropriate laser parameters (fluence and pulse duration), effective cooling, and immediate intervention after adverse events.
A combined analysis of these results showed that all clinical parameters of hair reduction were statistically significant when compared to the baseline. Our study included multiple clinical parameters like facial mFG score, predominant hair type, and frequency of hair removal. ADditionally including trichoscopy helped in better hair assessment. Compared to previous studies, more trichoscopic parameters and more facial sites were assessed. Results showed that total hair count, terminal hair count, and terminal-to-vellus hair ratio had statistically significant reductions in all four sites compared to the baseline.
Although various previous studies tried to assess the efficacy of diode lasers, our study was unique due to the inclusion of trichoscopic assessment and multiple clinical parameters. This may have increased the effectiveness of our study results. Studies on the safety of diode lasers in Indian skin color were limited and have mostly used lower fluences (less than 25 J/cm2). However, we concluded that diode laser therapy is safe in Indian skin color even at higher fluences (up to 36 J/cm2) and may help to reduce apprehension among dermatologists to use LHR over darker skin types.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Modified Ferriman-Gallwey score in hirsutism and its association with metabolic syndrome. Int J Trichology. 2017;9:7-13.
- [Google Scholar]
- Comparative study of the clinico-trichoscopic response to treatment of hirsutism with long pulsed (1064 nm) Nd:YAG laser in idiopathic hirsutism and polycystic ovarian syndrome patients. Lasers Med Sci. 2022;37:545-53.
- [Google Scholar]
- Trichoscopic changes in hair during treatment of hirsutism with 1064-nm neodymium:yttrium-aluminum-garnet laser. J Cosmet Dermatol. 2016;15:31-5.
- [Google Scholar]
- Diode laser 805 hair removal side effects in groups of various ethnicities—Cohort study results. J Lasers Med Sci. 2020;11:132-7.
- [Google Scholar]
- Efficacy of a low fluence, high repetition rate 810nm diode laser for permanent hair reduction in Indian patients with skin types IV–VI. J Clin Aesthet Dermatol. 2016;9:29-33.
- [Google Scholar]
- Comparison of alexandrite and diode lasers for hair removal in dark and medium skin: Which is better? J Lasers Med Sci. 2014;5:188-93.
- [Google Scholar]
- 800 nanometer diode laser hair removal in African American patients: A clinical and histologic study. J Cutan Laser Ther. 2000;2:183-90.
- [Google Scholar]
- The use of a new diode laser for hair removal. Dermatol Surg. 2003;29:30-3; discussion 33.
- [Google Scholar]
- Efficacy and safety of hair removal with a long-pulsed diode laser depending on the spot size: A randomized, evaluators-blinded, left-right study. Ann Dermatol. 2015;27:517-22.
- [Google Scholar]
- Six-month follow-up multicenter prospective study of 368 patients, phototypes III to V, on epilation efficacy using an 810-nm diode laser at low fluence. Lasers Med Sci. 2011;26: 247-55.
- [Google Scholar]






