Translate this page into:
Efficacy and safety of nanofractional radiofrequency in treatment of atrophic acne scars: A retrospective analysis of 5 years
*Corresponding author: Ishan Agrawal, Department of Dermatology, Maulana Azad Medical College, New Delhi, India. ishanagrawal1995@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kaur R, Sood S, Agrawal I, Ray A. Efficacy and safety of nanofractional radiofrequency in treatment of atrophic acne scars: A retrospective analysis of 5 years. J Cutan Aesthet Surg. doi:10.25259/jcas_3_24
Abstract
Objectives:
The objective of the study was to evaluate the efficacy of nanofractional radiofrequency in the treatment of acne scars.
Material and Methods:
In this 5-year retrospective study, adults with atrophic acne scars on their cheeks underwent four monthly sessions of nanofractional radiofrequency treatment (Venus Viva™, Venus Concept Inc., Toronto, Canada). Follow-up occurred 2 months after the last session. Clinical photographs were assessed by physicians and patients, and two dermatologists performed independent subjective analysis. Side effects, including pain, erythema, post-inflammatory pigmentation, and burning, were recorded after each session.
Results:
In the analysis, 65 patients were included, with a mean age of 27.6 ± 5.6 years. Among them, 67.7% had Fitzpatrick skin type IV. The mean satisfaction score at the end of the study was 7.33 ± 1.31, and 55.4% of patients scored >7. Of the 24 patients with scars lasting less than 6 months, 70.8% experienced >75% improvement. For patients with macular scars (11 in total), 72.7% saw >75% improvement. Transient pain and swelling were observed in all patients, while 32 out of 65 reported a burning sensation lasting <2 h.
Conclusion:
Nanofractional radiofrequency is highly effective, with positive responses in macular to mild scars. Scar duration is inversely related to treatment response. It is safe with transient, controlled side effects.
Keywords
Atrophic scars
Nanofractional laser
Acne scars
INTRODUCTION
Acne vulgaris is a chronic disorder of the pilosebaceous unit presenting with both inflammatory and non-inflammatory lesions commonly seen on the face. Prolonged cutaneous damage causes aberrant healing of the wound with increased tissue degradation and reduced biosynthesis of normal collagen. In about 80–90% of cases, this produces atrophic scars due to collagen destruction. Atrophic scars include ice pick scars, boxcar scars, and rolling scars. In atrophic scars, especially larger scars, there is fibrous anchoring of the dermis to subcutis, which is the target area of treatment.
Multiple resurfacing methods for treatment include laser resurfacing, dermabrasion, chemical peels, microneedling, and radiofrequency devices. At present, there is a higher demand for non-invasive procedures, which are outpacing surgical procedures.1
Our study utilizes a 160-pin/tip nanofractional radiofrequency device for the treatment of acne scars for evaluation of its efficacy and safety.
Aims and objectives
The objective of the study was to evaluate the efficacy of nanofractional radiofrequency in the treatment of acne scars.
MATERIAL AND METHODS
Study design and patient selection
This was a retrospective and single-center study done over 5 years duration among patients visiting a tertiary care center in North India from 2017 to 2022. We included all the patients above 18 years of age, diagnosed with atrophic acne scars over cheeks, previously treated with four procedure visits, and followed up at 2 months after the last sitting. Clinical photographs using Reveal® Imager version 6.1.1 were taken on each sitting in the same settings and lighting. These photos were analyzed at the end of the study (Physician assessment and patient self-assessment). The acne scars were graded using the Goodman and Baron Qualitative Global scarring grading system.
Macular: Erythematous, hypo- or hyperpigmented flat scars
Mild: Scars not visible at 50 cm or more and easily covered with make-up
Moderate: Scars visible at 50 cm or more and not easily covered with make-up. However, they can be flattened by manual stretching of the skin
Severe: Scars visible at 50 cm or more, which cannot be covered by makeup and do not flatten on manual stretching.
Patients with a history of sensitivity to topical anesthesia, local cutaneous infection, and patients with a history of keloids and herpes were excluded from the study.
Procedure
The treatment area was cleaned using an alcohol swab, and topical lignocaine cream was applied for 45 min before starting the procedure. All the patients received four sessions of nanofractional radiofrequency (Venus Viva™, Venus Concept Inc., Toronto, Canada) done monthly. The Viva™ hand piece has 160 pins/tips in a continuous design pattern. All patients were treated with similar parameters of 260–270 volts with 20 ms pulse duration for two passes done from lateral to medial side. After the procedure, patients were instructed to apply cold compresses physical sunscreen 3 times a day and avoid undue sun exposure. The patients were advised not to use any make-up for 72 hours. Patients were explained about the downtime and possible side effects of the procedure. In case of persistent erythema, the patient was advised to use mild corticosteroids for 2–3 days. Simultaneously, patients were prescribed Cap Doxycycline 100 mg and Azelaic acid 10% cream in case of inflammatory acne.
Outcome analysis
The primary analysis was done by two independent dermatologists who were not a part of the study using physician subjective analysis in terms of improvement on a quartile scale as 0–25%, 25–50%, 50–75%, and >75% improvement. Patient satisfaction score on a scale of 0–10 (0 indicated no improvement and 10 indicated excellent improvement) was recorded by the patient on assessing the photographic results.
Subjective analysis was also done by two independent dermatologists using the clinical photographs taken. All possible side effects, including pain, edema, erythema, post-inflammatory pigmentation, and burning, were recorded at each sitting.
Evaluation and statistics
Qualitative data were represented in the form of frequency and percentage. Quantitative data were represented using Mean ± Standard Deviation. The association between qualitative variables was assessed by the Chi-square test. The resultant values were analyzed using the statistical software Statistical Package for the Social Sciences (SPSS Version 23.0; SPSS Inc., Chicago, USA), and values <0.05 were considered significant at a 95% confidence interval.
RESULTS
A total of 65 patients were included in the final analysis. The mean age of patients was 27.6 ± 5.6 years, with 49 (75.4%) female patients and 16 (24.6%) male patients. Most of the patients had Fitzpatrick skin type IV (67.7% of patients). About 20.0% of patients had skin type III, and 12.3% of patients had skin type V. Based on qualitative grading according to Goodman and Baron Global Scarring System, 16.9% had macular scars, 24.6% had mild scars, 43.1% had moderate, and 15.4% had severe acne scars. The mean duration of acne scars was 17.8 ± 16.5 months.
Subjective physician evaluation score using a quartile scale is given in Table 1. Most of the patients had 25–50% improvement by 2nd follow-up and >75% improvement by 4th follow-up. The mean patient satisfaction score at the end of the study was 7.33 ± 1.31, with 36 (55.4%) patients with a score of more than 7 [Table 2].
| Improvement (%) | 2nd follow-up | 4th follow-up | ||
|---|---|---|---|---|
| 0–25 | 12 | 18.5% | 3 | 4.6% |
| 26–50 | 33 | 50.8% | 11 | 16.9% |
| 51–75 | 20 | 30.8% | 23 | 35.4% |
| >75 | 0 | 0.0% | 28 | 43.1% |
| Patient satisfaction score | Number of patients | Percentage of patients |
|---|---|---|
| <5 | 4 | 6.2% |
| 5–7 | 25 | 38.5% |
| >7 | 36 | 55.4% |
Out of all 24 patients who had scars of duration up to 6 months, 17 (70.8%) patients had >75% improvement. Among 17 patients with scar duration of 7–12 months, 8 (47.1%) patients had >75% improvement. Out of 12 patients with scar duration of more than 24 months, none of the patients had >75% improvement, and 6 (50%) patients had 50–75% improvement at the end of the 4th follow-up [Table 3].
| Duration of lesion (months) | Improvement (%) | Total | |||
|---|---|---|---|---|---|
| < 25 | 26–50 | 51–75 | >75 | ||
| ≤6 m | 0 | 2 | 5 | 17 | 24 |
| 0.0% | 8.3% | 20.8% | 70.8% | 100.0% | |
| 7–12 m | 0 | 3 | 6 | 8 | 17 |
| 0.0% | 17.6% | 35.3% | 47.1% | 100.0% | |
| 13–24 m | 1 | 2 | 6 | 3 | 12 |
| 8.3% | 16.7% | 50.0% | 25.0% | 100.0% | |
| >24 m | 2 | 4 | 6 | 0 | 12 |
| 16.7% | 33.3% | 50.0% | 0.0% | 100.0% | |
| Total | 3 | 11 | 23 | 28 | 65 |
| 4.6% | 16.9% | 35.4% | 43.1% | 100.0% | |
P=0.008
On analyzing the patient satisfaction score and its association with the duration of scars, out of 24 patients with scar duration up to 6 months, 17 (70.8%) patients had >75% improvement, and among 17 patients with scars with a duration of 7–12 months, and 12 (70.6%) patients had >75% improvement. About 50% of patients with scar duration of >24 months had a satisfaction score between 5 and 7, and 33.3% of patients had a satisfaction score of <5 [Table 4].
| Duration of lesion (months) | Patient satisfaction | Total | ||
|---|---|---|---|---|
| <5 | 5–7 | >7 | ||
| ≤6 m | 0 | 7 | 17 | 24 |
| 0.0% | 29.2% | 70.8% | 100.0% | |
| 7–12 m | 0 | 5 | 12 | 17 |
| 0.0% | 29.4% | 70.6% | 100.0% | |
| 13–24 m | 0 | 7 | 5 | 12 |
| 0.0% | 58.3% | 41.7% | 100.0% | |
| >24 m | 4 | 6 | 2 | 12 |
| 33.3% | 50.0% | 16.7% | 100.0% | |
| Total | 4 | 25 | 36 | 65 |
| 6.2% | 38.5% | 55.4% | 100.0% | |
P=0.001
Out of 11 patients who had macular scars, 8 (72.7%) patients had >75% improvement, and among 16 patients with mild scars, 10 (62.5%) patients had >75% improvement. Out of 10 patients with severe scars, only 1 patient had >75% improvement, and 4 (40%) patients had 25–50% improvement at the end of the 4th follow-up [Table 5].
| Grade of lesion | Improvement (%) | Total | |||
|---|---|---|---|---|---|
| <25 | 26–50 | 51–75 | >75 | ||
| Macular | 0 | 1 | 2 | 8 | 11 |
| 0.0% | 9.1% | 18.2% | 72.7% | 100.0% | |
| Mild | 1 | 2 | 3 | 10 | 16 |
| 6.3% | 12.5% | 18.8% | 62.5% | 100.0% | |
| Moderate | 0 | 4 | 15 | 9 | 28 |
| 0.0% | 14.3% | 53.6% | 32.1% | 100.0% | |
| Severe | 2 | 4 | 3 | 1 | 10 |
| 20.0% | 40.0% | 30.0% | 10.0% | 100.0% | |
| Total | 3 | 11 | 23 | 28 | 65 |
| 4.6% | 16.9% | 35.4% | 43.1% | 100.0% | |
P=0.007
On analyzing the patient satisfaction score and its association with the type of scars, out of 11 patients with macular scars, 10 (90.9%) patients had a score of more than 7 and among 16 patients with mild scars, and 9 (56.3%) patients had >75% improvement. About 60% of patients with severe scars had satisfaction scores between 5 and 7, and 20% of patients with severe scars had a score of less than 5 and more than 7 each [Table 6].
| Grade of lesion | Patient satisfaction | Total | ||
|---|---|---|---|---|
| <5 | 5–7 | >7 | ||
| Macular | 0 | 1 | 10 | 11 |
| 0.0% | 9.1% | 90.9% | 100.0% | |
| Mild | 0 | 7 | 9 | 16 |
| 0.0% | 43.8% | 56.3% | 100.0% | |
| Moderate | 2 | 11 | 15 | 28 |
| 7.1% | 39.3% | 53.6% | 100.0% | |
| Severe | 2 | 6 | 2 | 10 |
| 20.0% | 60.0% | 20.0% | 100.0% | |
| Total | 4 | 25 | 36 | 65 |
| 6.2% | 38.5% | 55.4% | 100.0% | |
P=0.037
All the side effects reported by the patients are given in Table 7. None of the patients had any serious side effects [Figures 1-4].
| Side effect | Number of patients affected | Average duration |
|---|---|---|
| Pain | 65/65 | 1–2 h |
| Edema | 60/65 | 1–2 h |
| Erythema | 65/65 | 2 days |
| Post-inflammatory pigmentation | 0/65 | - |
| Burning sensation | 32/65 | 1–2 h |
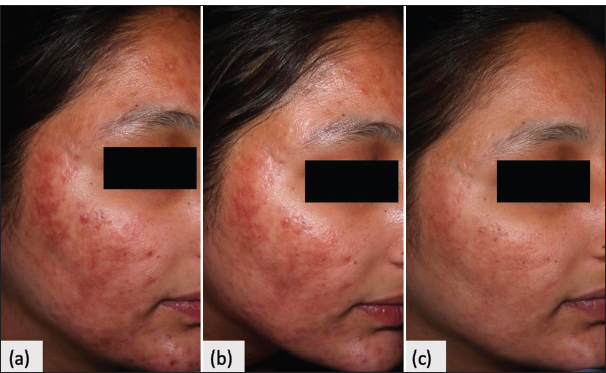
- Clinical photo. (a) Baseline moderate scars. (b) 25–50% improvement at 2nd follow-up. (c) >75% improvement at 4th follow-up.
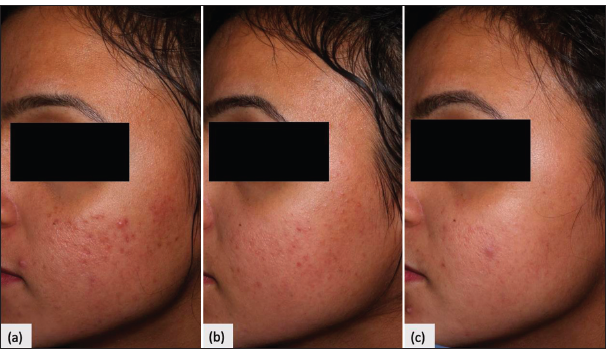
- Clinical photo. (a) Baseline macular scars. (b) 50–75% improvement at 2nd follow-up. (c) >75% improvement at 4th follow-up.
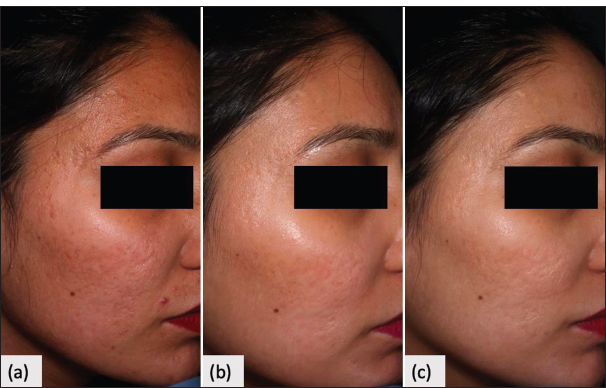
- Clinical photo. (a) Baseline moderate scars. (b) 25–50% improvement at 2nd follow-up. (c) 50–75% improvement at 4th follow-up.
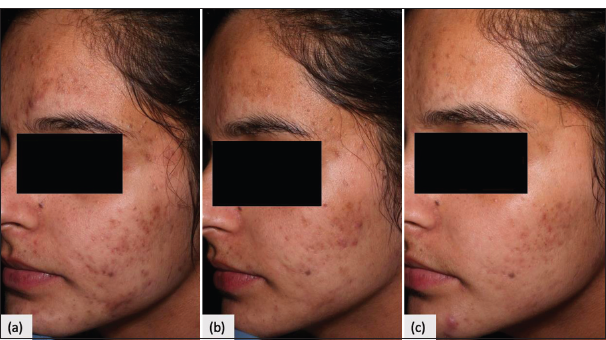
- Clinical photo. (a) Baseline mild scars. (b) 50–75% improvement at 2nd follow-up. (c) >75% improvement at 4th follow-up.
DISCUSSION
Acne vulgaris is a ubiquitous problem, and altered healing response results in scarring. The dermis is tethered to the underlying subcutis by fibrous strands with net collagen destruction over the affected area. Correction of the subdermal component is the focus of treatment.2
Energy-based devices are becoming increasingly popular, and they have been long established as a useful therapeutic modality in the improvement of skin laxity, with effective treatment of conditions related to aging.
Energy-based devices, though popular due to their noninvasive nature, are limited by their side effects of increased downtime and post-inflammatory hyperpigmentation. These side effects are, however, limited by fractional technology, which creates evenly spaced microthermal zones that recover fast and with less pigmentation.3
Radiofrequency devices deliver energy through chromophore-independent mechanisms, which ensure outcomes regardless of the subject’s skin type. Fractionated radiofrequency energy creates columns of controlled energy delivery, which stimulates a homogenous, uniform, and physiological healing response. Recovery of the affected skin area yields a desirable end result of skin healing with matrix reconditioning, volume restoration, and desired re-epithelialization. Nanofractional radiofrequency creates smaller microcolumns with limited wounding, which reduces the downtime and reduces the side effects.4 Statistically, there is no significant difference between the outcome of acne scar treatment between fractional radiofrequency and ablative laser, with a similar effectiveness between the both. Relatively more pain, with considerably longer downtime and a higher incidence of cutaneous adverse effects, has been noted with ablative lasers.5
Our study showed that 43% of patients showed over 75% improvement according to physician evaluation. Improvement was noted with refinement in the depth and texture of the scars. Among patients showing >75% improvement, 70.8% had scars for up to 6 months. Side effects were primarily post-procedural redness, swelling, and pain, which were transient and effectively controlled with the use of mild topical corticosteroid creams for 2 days. No post-inflammatory hyperpigmentation was seen in our patients, with skin types between III and V. Almost 68% of our patients had Fitzpatrick skin type IV. A comparable safe profile of nanofractional radiofrequency was noted by Goel and Gatne in their study of acne scar treatment, where no pigmentary defect was noted in darker skin types.3
Similar results were noted by Nitayavardhana et al. with MNRF, where similar parameters were used with Fitzpatrick III-V skin types. Their study has a longer follow-up period with marked improvement seen at 6 months in about 48% of patients. In their study, 13% of patients showed postinflammatory hyperpigmentation (PIH), which was not seen in our patients, possibly due to post-treatment corticosteroid use. The authors suggested customized parameter adjustment depending on skin type and scar type to control PIH occurrence. An additional improvement in skin laxity with facial contouring was observed in their study.4 Overall, a desirable improvement in acne scars was seen in our patients, which was achieved by the more precise power control and duration of energy pulse with fractional radiofrequency.6
Our patient showed considerably high satisfaction levels, >7 in 55.4%, with just four sessions of radiofrequency. As this is a cosmetic procedure, patient satisfaction is an important gauge of assessing treatment effectiveness. About 43% of patients in our study had >75% improvement. In cases with >75% improvement, 72% had macular scar, and 62.5% had mild scars; 70% had scars for <6 months duration. These patients also had a higher satisfaction score, which mirrored the improvement rates noted by study investigators. The only side effects noted were pain and swelling, which did not last beyond 1–2 h and redness, which was transient and well-controlled with topical steroids. Considering these findings, we found that nanofractional radiofrequency is an excellent modality of treatment, especially in milder and younger scars, with good patient satisfaction and transient side effects.
Limitations
The objective quantitative analysis of the individual scars was not done. The efficacy of the therapy was not compared to any other standard mode of therapy in the acne scar treatment.
CONCLUSION
Nanofractional radiofrequency technology is an effective and safe treatment option for the treatment of atrophic acne scars. It helps in improving the depth and the surface texture of the scars. The macular to mild scars respond favorably to the therapy, and the duration of scars is inversely proportional to the response to therapy.
Authors’ contributions
Ramandeep Kaur and Seema Sood contributed in conception or design. Ishan Agrawal and Arunima Ray contributed in acquiring and analyzing data, drafting the manuscript. Ramandeep Kaur and Arunima Ray reviewed the work, and approved the final version.
Ethical approval
Institutional Ethics committee approval was not taken for this study as it involved analysis of the existing recorded data, and the done procedure for acne scars is an already approved treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Subject satisfaction following treatment with nanofractional radiofrequency for the treatment and reduction of acne scarring and rhytids: A prospective study. J Cosmet Dermatol. 2021;20:3475-34.
- [CrossRef] [PubMed] [Google Scholar]
- Acne scarring-pathogenesis, evaluation, and treatment options. J Clin Aesthet Dermatol. 2017;10:12-23.
- [Google Scholar]
- Use of nanofractional radiofrequency for the treatment of acne scars in Indian skin. J Cosmet Dermatol. 2017;16:186-92.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy and safety of fractional radiofrequency nanoneedle system in the treatment of atrophic acne scars in Asians. J Cosmet Dermatol. 2020;19:1636-41.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and efficacy of fractional radiofrequency for the treatment and reduction of acne scarring: A prospective study. Lasers Surg Med. 2022;54:74-81.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective, pilot evaluation of the performance of nanofractional radiofrequency for improvement of skin texture via skin resurfacing. J Cosmet Dermatol. 2018;17:61-5.
- [CrossRef] [PubMed] [Google Scholar]







