Translate this page into:
Efficacy of autologous platelet rich plasma with subcision vs platelet rich plasma with microneedling in atrophic acne scars: A single-center, prospective, intra-individual split-face comparative study
*Corresponding author: Prasoon Soni, Dermatology, Venereology and Leprosy, Sardar Patel Medical College, JNV Colony, Bikaner, Rajasthan, India. drprasooni@gmail.com
How to cite this article: Yadav MK, Soni P, Ghiya BC, Mehta RD, Arora A, Jangir VK, et al. Efficacy of autologous platelet rich plasma with subcision vs platelet rich plasma with microneedling in atrophic acne scars: A single-center, prospective, intra-individual split-face comparative study. J Cutan Aesthet Surg. 2024;17:184-8. doi: 10.4103/JCAS.JCAS_218_22
Abstract
Objectives:
Severe post-acne scarring has been implicated as a cause of considerable psychological distress, mainly among adolescents. Subcision and microneedling are treatment options available. In this study, we aimed to compare the efficacy of microneedling with platelet-rich plasma (PRP) against subcision with PRP in treating atrophic post-acne scars in a split-face study design.
Material and Methods:
Fifty patients with atrophic post-acne facial scars were included in this prospective interventional study. Group A (left side of the face) was managed by microneedling with PRP and group B (right side of the face) was subjected to subcision with PRP. Results were assessed based on Goodman and Baron qualitative and quantitative grading.
Results:
In our study, at the end of the treatment, on the left side, 5 (10%) had 1 grade of improvement showing good response, 35 (70%) had 2 grades of improvement showing very good response, and 10 (20%) had 3 grades of improvement showing excellent response. On the right side, 1 (2%) patient had no improvement in acne grade showing poor response, 9 (18%) had 1 grade of improvement showing good response, 25 (50%) had 2 grades of improvement showing very good response, whereas 15 (30%) had 3 grades of improvement showing excellent response.
Conclusion:
Both modalities showed statistically significant results individually, there was no significant difference in qualitative improvement of acne scars between the two groups.
Keywords
Acne scars
Microneedling
Platelet-rich plasma
Subcision
INTRODUCTION
Severe post-acne scarring has been implicated as a cause of considerable psychological distress, mainly among adolescents.1 Many treatment options are available, such as chemical peels, dermabrasion, lasers, punch techniques, silicone gels, cryotherapy, microneedling, and combined therapies for acne scars.2 The majority of these therapy methods, however, have the drawback of either having significant morbidity or only being sporadic effective. Subcision and microneedling are cutting-edge treatment options.
In this study, we aimed to compare the efficacy of microneedling with platelet-rich plasma (PRP) against subcision with PRP in treating atrophic post-acne scars in a split-face study design.
MATERIAL AND METHODS
Fifty patients of atrophic post-acne facial scars were included in this single-center, prospective, intra-individual split-face comparative study. Group A included the left side of the face managed by microneedling with PRP and group B included the right side of the face that was subjected to subcision with PRP.
Inclusion criteria
Patients aged between 18 and 45 years of age who have grade 2, 3, or 4 acne scars according to Goodman and Barons grading.
Patients who gave consent to undergo multiple sessions were included in the study.
Exclusion criteria
Patients with active infections like bacterial infections, herpes simplex, or warts.
Patients with active acne at the time of presentation.
Patients who are on oral retinoids or who have taken the same in the past 6 months.
Patients with bleeding tendencies.
Patients with keloid-forming tendencies.
Pregnant or lactating females.
For the preparation of PRP, a volume of 20 mL of whole blood was collected and separated into two sterile conical test tubes of 10 mL each containing acid-citrate dextrose and subjected to first centrifugation at 1200 rpm for 15 min. Three layers were formed in each tube: plasma, buffy coat, and red cell sediments. After discarding red cell sediments, the remaining solution was allowed for further centrifugation at 2000 rpm for 10 min, which resulted in a dense layer of platelet at the bottom and a clear fluid layer on the top. Most of the clear fluid (platelet-poor plasma) was removed, leaving behind a small solution which was PRP.
Subcision was performed under topical anesthesia. Number 18- or 20-G needle or a Nokor needle (1.5 in, 18-G) was inserted adjacent to the scar with the bevel upwards parallel to the skin surface, into the deep dermis and moved back and forth in a fan-like motion under the scar to release fibrous bands at dermal or deep dermal subcutaneous plane. Haemostasis was maintained with pressure and ice application. Then, 3-4 mL of PRP was injected at the site of subcision.
Microneedling was carried out using a dermaroller studded with 192 microneedles in eight rows and 1.5 mm in length. Dermaroller was applied sequentially in horizontal, vertical, and diagonal directions till pinpoint bleeding occurred. The area was cleaned with normal saline and prepared volume (3-4 mL) of PRP was then applied over the treated area with a gentle massage. It was further followed up with another few rounds of microneedling.
The patients were thoroughly evaluated on each visit based on digital photographs and changes in grading of the acne scars based on qualitative and quantitative Goodman and Baron Scale. The patient received four to six sittings at the interval of 4 weeks in each group. At the end of all sittings, the scars were graded using the grading system as used in the beginning. Photographs of both sides of the face were taken under consistent background, position, and lighting. These pictures were compared with the pretreatment images. The patients were thoroughly evaluated on each visit based on photographs and changes in grading of the acne scars based on Goodman and Baron Scale.
The improvement was rated as follows: Excellent, improvement by three grades were considered as excellent; Very Good, improvement by 2 grades; Good, improvement by 1 grade; and Poor, no upgradation on assessment. All adverse effects that occurred due to the treatment were noted down.
RESULTS
In this study, the age of patients ranged from 18 to 39 years. The mean age of males was 27.57± 6.01 years, while that of females was 26.13 ± 6.87 years. Overall, the mean age was 27.14 ± 6.15 years. In our study, there were 30% females and 70% males. The male-to-female ratio was 2.33:1. The predominant scar type was boxcar scars with 54% cases, while the remaining 46% cases had rolling scars. The acne grading into two groups was comparable at baseline (P-value = 0.45).
Over the left side of the face that was managed with microneedling with PRP, 36% had grade 1 scars and 64% had grade 2 scars at the completion of the study. A statistically significant improvement was noted on the left side of the face (P-value = 0.04) [Figures 1 and 2]. Over the right side of the face that was managed with subscision, 48% had grade 1 scars, 48% had grade 2 scars, and 4% had grade 3 scars at the completion of the study. A highly significant improvement was noted on the right side of the face (P-value = 0.001) [Figures 3 and 4], which was statistically even more than the left side.
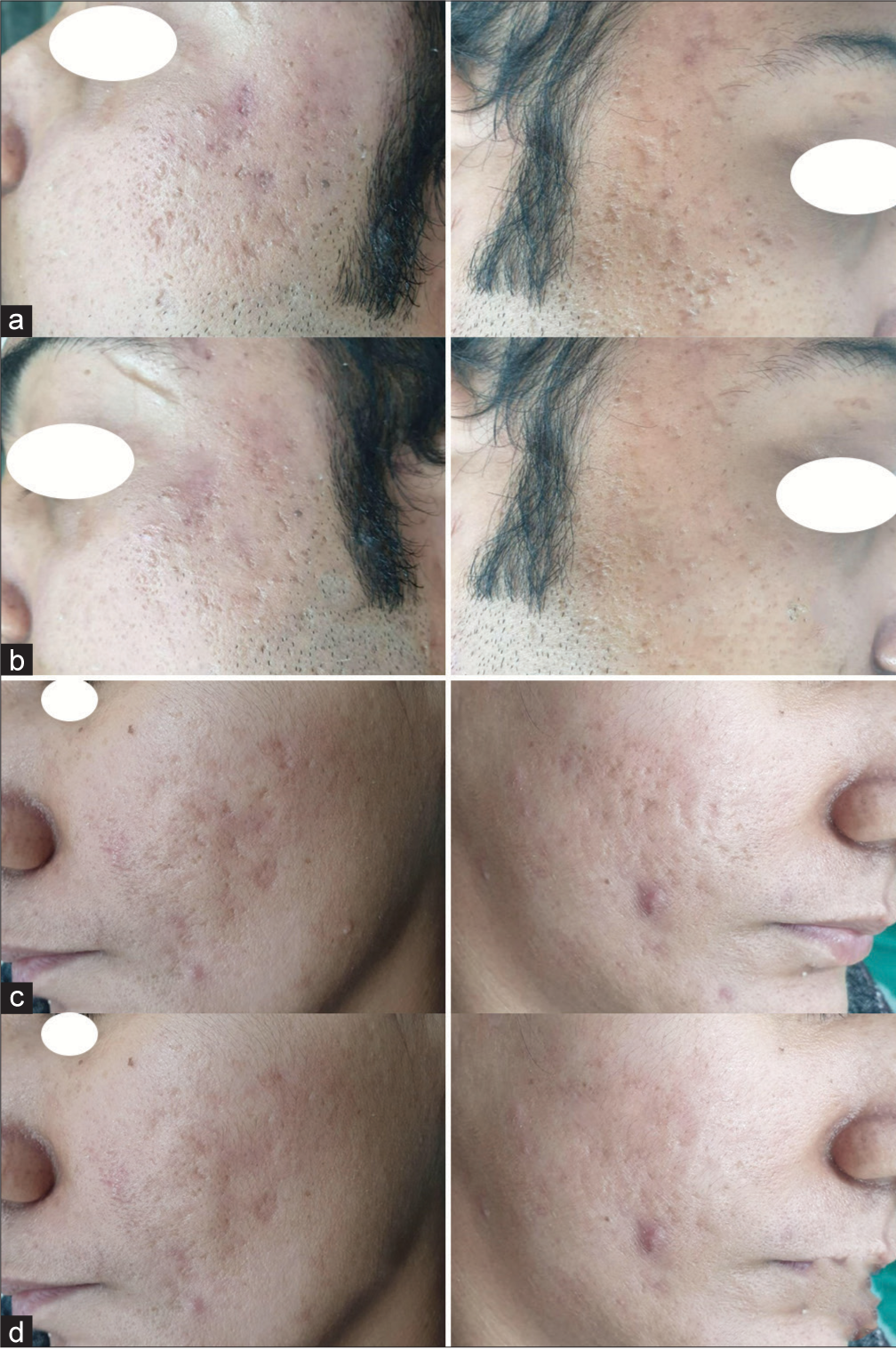
- Pre- and post-photographs of the patient showing improvement by (a) 2 grades after microneedling with platelet-rich plasma (PRP) on the left side of the face after 4 months of follow-up; (b) three grades after subcision with PRP on the right side of the face after 4 months of follow-up; (c) 1 grade after microneedling with PRP on the left side of the face after 4 months of follow-up; (d) 2 grades after subcision with PRP on the right side of the face after 4 months of follow-up.
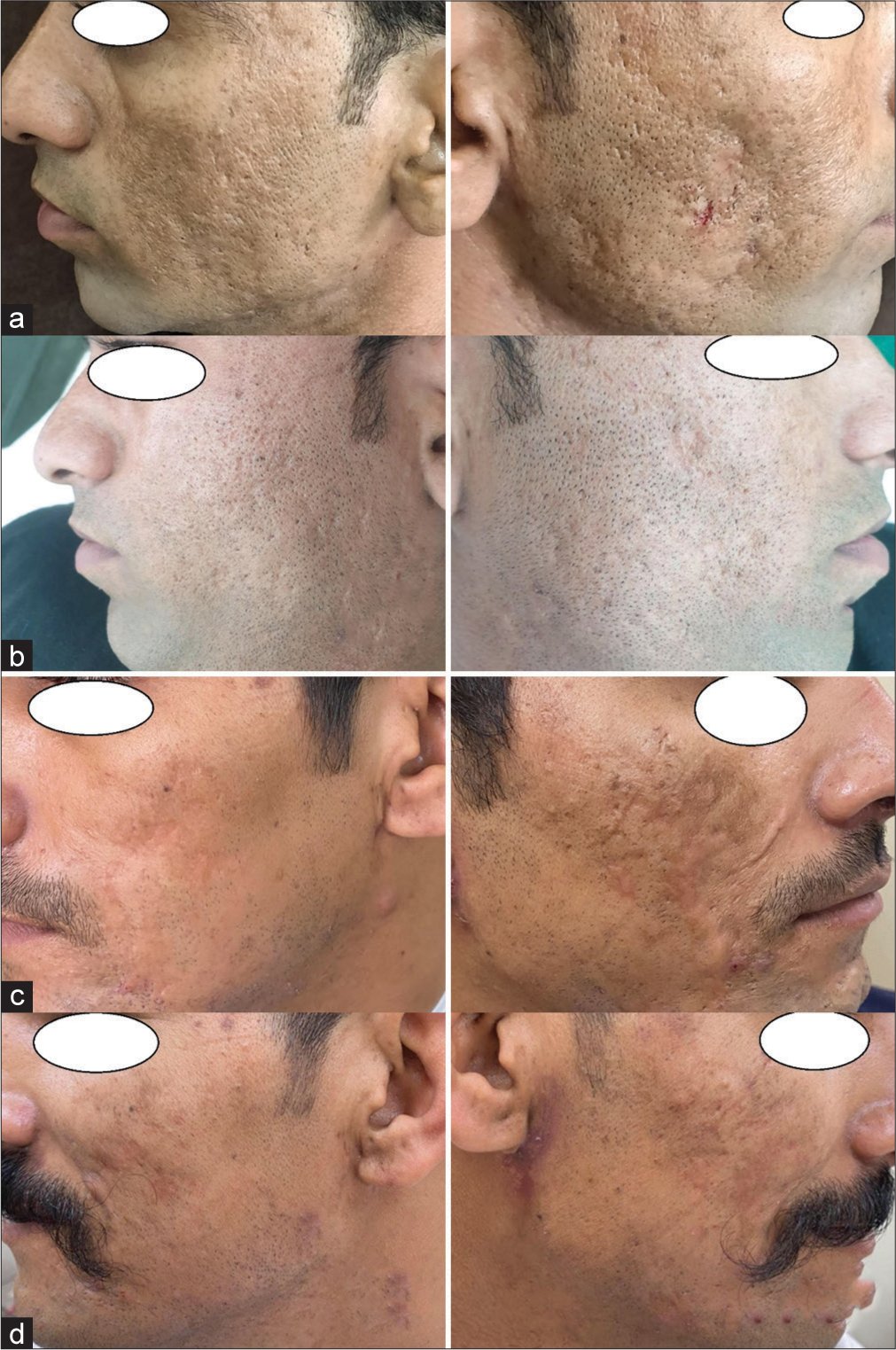
- Pre- and post-photographs of the patient showing improvement by (a) 1 grade after microneedling with platelet-rich plasma (PRP) on the left side of the face after 4 months of follow-up; (b) 2 grades after subcision with PRP on the right side of the face after 4 months of follow-up; (c) 1 grade after microneedling with PRP on the left side of the face after 4 months of follow-up; (d) 1 grade after subcision with PRP on the right side of the face after 4 months of follow-up.
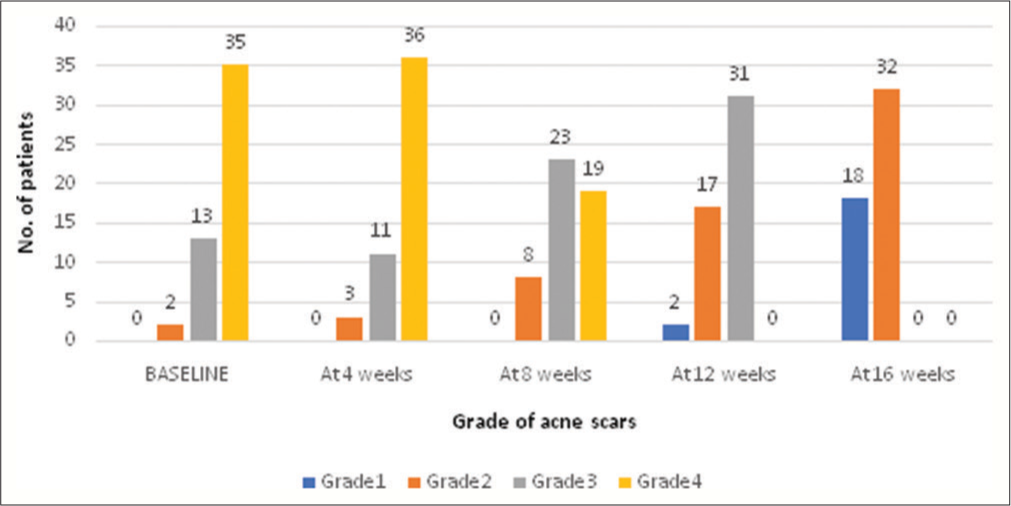
- Qualitative improvement on the left side of the face (microneedling with platelet-rich plasma (PRP)).
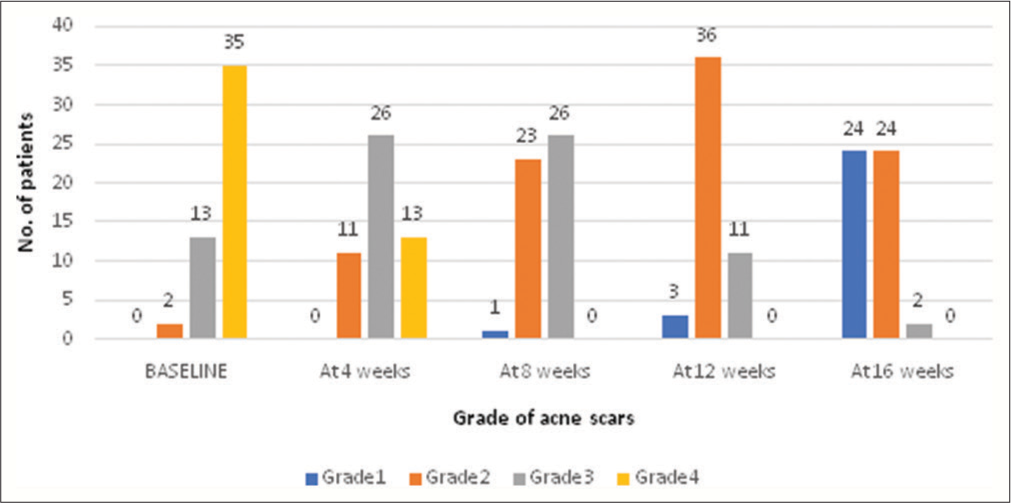
- Qualitative improvement on the right side of the face (subcision with platelet-rich plasma (PRP)).
In our study, at the end of the treatment over on the left side, 5 (10%) had improvement by 1 grade showing good response, 35 (70%) had 2 grades of improvement showing very good response, and 10 (20%) had 3 grades of improvement showing excellent response. While on the right side, 1 (2%) patient had no improvement in acne grade showing poor response, 9 (18%) had improvement by 1 grade showing good response, 25 (50%) had improvement by 2 grades showing very good response, while 15 (30%) had improvement by 3 grades showing excellent response [Table 1].
| Improvement grading | Left side | Right side |
|---|---|---|
| Excellent (reduction in acne scar by three grades from baseline) | 35 | 25 |
| Very good (reduction in acne scar by 2 grades from baseline) | 5 | 9 |
| Good (reduction in acne scar by 1 grades from baseline) | 0 | 1 |
| Poor (reduction in acne scar by 2 grades or more from baseline) | ||
| P-value | 0.2 | |
The change in the grade of acne scars was comparable between the two groups (P-value = 0.2). Thus, there was no significant difference in qualitative improvement of acne scars between the two groups.
In our study, Goodman and Baron’s quantitative score assessment of acne scars revealed that after 4 weeks, 8 weeks, 12 weeks, and 16 weeks, the difference between the improvement of acne scars between the two groups was statistically insignificant (P-values = 0.76, 0.16, 0.27, 0.09) [Table 2].
| Baseline | At 4 weeks | At 8 weeks | At 12 weeks | At 16 weeks | |
|---|---|---|---|---|---|
| Left side (microneedling with PRP) | 25.2±6.8 | 24.4±6.8 | 23.8±6.4 | 21.2±6.6 | 20.0±6.5 |
| Right side (subcision with PRP) | 25.1±6.7 | 24±6.5 | 21.8±6.2 | 19.9±4.9 | ±4.7 |
| P-value | 0.76 | 0.27 | 0.09 |
PRP: platelet-rich plasma
The side effect profile was significantly better in patients treated with dermaroller + PRP than those treated with subscision with PRP. Erythema and pain were the most commonly reported side effects in both groups. Besides this, scarring and hematoma formation were also seen in group B.
DISCUSSION
Acne scars pose a major impact on patients’ quality of life, especially, in the first three decades of life. Often, these unsightly scars can be a source of even greater embarrassment than the acne itself. Goodman and Baron included all morphological varieties of post-acne scars and employed qualitative clinical evaluation as the instrument to grade the scars on a scale of severity.3 Qualitative Goodman and Baron scale for grading acne scars is as below:
Grade 1: Macular erythematous hypo or hyperpigmented scars.
Grade 2: Mild atrophy not obvious at a social distance of >50 cm or easily covered by facial makeup or beard hair.
Grade 3: Moderate atrophy obvious at a social distance of >50 cm; not easily covered by makeup or beard hair; but able to be flattened by manual stretching.
Grade 4: Severe atrophy not flattened by manual stretching of skin.
Goodman and Baron also gave a quantitative global scarring grading, in which different types of scars are given increasing scores: Macular or mildly atrophic (1 point), moderately atrophic (2 points), punched out or linear-troughed severe scars (3 points), and hyperplastic papular scars (4 points).
The multiplication factor for these lesion types is based on the numerical range wherein, for 1-10 scars, the multiplier is 1; for 11-20 it is 2; and for >20 it is 3.
There is a wide range of options available in the treatment armamentarium for acne scars.2 Subcision done using Nokor needle or an 18G needle has proven to be an effective modality. The principle of this procedure is to break the fibrotic strands, which tether the scar to the underlying subcutaneous tissue.4 Microneedling is also a good modality for acne scar management and can be done either using a dermaroller or a micropen. Depending on the length of the needles, the needles penetrate into the dermis and initiate a complex chemical cascade including numerous growth factors, such as fibroblast growth factor, platelet-derived growth factor, and transforming-growth factor alpha and beta, which result in an invasion of fibroblasts. This surge of activity inevitably leads to the production of more collagen and elastin by the fibroblasts.5 PRP acts by stimulating the collagen remodeling within the scar tissue and has been combined with various modalities for managing acne scars including subcision and dermaroller.6 Owing to the variable morphology of these atrophic acne scars, no single management is completely effective. Therefore, it has been rationalized that the combination of various modalities is effective for scarring.7
Our study intended to analyze the role of PRP with subcision and PRP with dermaroller for the management of acne scars.
In our study, we compared the two methods of treatment, namely subcision and microneedling with PRP as an adjuvant in both groups to compare their efficacy and safety for treating acne scars based on an improvement in the qualitative acne scar grading system. We analyzed the scars’ improvement with respect to their grading of severity before and after the treatment. Our observations on qualitative assessment depicted that there was a comparable improvement in both group A and group B with no significant difference between the two groups.
A statistically significant improvement was noted on the left side of the face treated with microneedling and PRP (P-value = 0.04) in our study. Similar results were reported by Yaseen et al.8 In their study, out of 15 grade 3 scars, 8 (53.3%) improved by grade 1, 7 (46.6%) improved by 2 grades, whereas 8 (100%) grade 2 cases improved to grade 1. All the patients in their study were highly satisfied with their results.
A highly significant improvement was noted on the right side of the face treated with subcision and PRP (P-value = 0.001), which was statistically even more than the left side (P-value = 0.04). Our observations on qualitative assessment depicted that there was a comparable improvement in both group A and group B with no significant difference between the two groups. Deshmukh et al.9 also found that a combination of PRP and subcision showed greater improvement (32.08%) in acne-induced atrophic scars. Asif et al.10 also observed 62.20% improvement in acne scars on Goodman’s quantitative scale with a combination of PRP with dermaroller.
The side effect profile was significantly better in patients treated with dermaroller and PRP than those treated with subcision with PRP (P-value = 0.04). In a study, by Garg et al.11 transient post-inflammatory dyspigmentation and aggravation of acne was noted in 6% of subjects. Even in a study by Barman et al.,12 the most common adverse event was post-inflammatory hyperpigmentation and erythema in both groups. However, unlike us, no other significant adverse event was noted in any of their cases.
CONCLUSION
Till date, no other study has compared the two modalities head-to-head with adjuvant PRP in both groups. There was no significant difference in qualitative improvement of acne scars between the two groups. Our study, therefore, found that both modalities were equally effective in managing acne scars with no significant difference.
Authors’ contributions
All the authors contributed to the research study. Manoj Kumar Yadav, Prasoon Soni, Bhikam Chand Ghiya, Rajesh Datt Mehta, Aakanksha Arora, Vishnu Kumar Jangir, Rajesh Khokhar, Sumiti Pareek: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal.
The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Psychosocial impact of acne vulgaris: Evaluating the evidence. Skin Therapy Lett. 2004;9:1-3, 9
- [Google Scholar]
- Interventions for acne scars. Cochrane Database Syst Rev. 2016;4:11946.
- [CrossRef] [PubMed] [Google Scholar]
- Postacne scarring: A qualitative global scarring grading system. Dermatol Surg. 2006;32:1458-66.
- [CrossRef] [PubMed] [Google Scholar]
- Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg. 1995;21:543-9.
- [CrossRef] [PubMed] [Google Scholar]
- Microneedling therapy for atrophic acne scars: An objective evaluation. J Clin Aesthet Dermatol. 2015;8:36-42.
- [Google Scholar]
- Combined use of skin needling and platelet-rich plasma in acne scarring treatment. Cosmet Dermatol. 2011;24:177-83.
- [Google Scholar]
- Standard guidelines of care for acne surgery. Indian J Dermatol Venereol Leprol. 2008;74:S28-36.
- [Google Scholar]
- Combination of platelet rich plasma and microneedling in the management of atrophic acne scars. Int J Res Dermatol. 2017;3:346-50.
- [CrossRef] [Google Scholar]
- Platelet-rich plasma augments subcision in atrophic acne scars: A split-face comparative study. Dermatol Surg. 2019;45:90-8.
- [CrossRef] [PubMed] [Google Scholar]
- Combined autologous platelet-rich plasma with microneedling verses microneedling with distilled water in the treatment of atrophic acne scars: A concurrent split-face study. J Cosmet Dermatol. 2016;15:434-43.
- [CrossRef] [PubMed] [Google Scholar]
- Combination therapy in the management of atrophic acne scars. J Cutan Aesthet Surg. 2014;7:18-23.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative evaluation of microneedling alone versus combined subcision and microneedling in post acne scars. Gulf J Dermatol Venereol. 2021;2:24-33.
- [Google Scholar]






