Translate this page into:
Efficacy of fractional carbon dioxide laser-assisted drug delivery in the management of post-burn scars – A prospective study
*Corresponding author: Senkadhir Vendhan, Department of Dermatology, Bharat Ratna Dr Babasaheb Ambedkar Memorial Hospital, Mumbai, Maharashtra, India. vendhan100@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Neema S, Vendhan S, Vasudevan B, K L, Dakshinamurthy S. Efficacy of fractional carbon dioxide laser-assisted drug delivery in the management of post-burn scars – A prospective study. J Cutan Aesthet Surg. 2024;17:219-26. doi: 10.25259/jcas_181_23
Abstract
Objectives:
The objective of our study is to assess the efficacy of fractional carbon dioxide (CO2) laser-assisted drug delivery (LADD) in the management of post-burn scars.
Material and Methods:
It is a prospective study conducted from March 2021 to February 2022, with 32 patients ranging in age from 9 to 52 years. The scars lasted anywhere from 6 months to 18 years. The ethical clearance of the Institutional Ethics Committee was obtained. The patient’s median age was 22 (range, 09–52). Patients were assessed using a modified Vancouver scar scale (mVSS) score before and after receiving fractional CO2 laser at monthly intervals.
Results:
After one treatment, statistically significant improvements in pigment, thickness, and pliability were seen according to the mVSS scores, and these improvements persisted through the final laser session.
Conclusion:
Our study has demonstrated that fractional CO2 LADD seems to be an encouraging approach in the management of post-burn scars with good patient satisfaction.
Keywords
Burn scar
Fractional co2 laser
Fractional photothermolysis
Laser-assisted drug delivery
mVSS score
INTRODUCTION
Hypertrophic scarring (HTS) after a burn injury negatively impacts the quality of life due to related contractures, hypertrophic alterations, and keloid formation in addition to deformity. The fibroproliferative condition known as HTS is thought to be caused by excessive and disorganized collagen deposition as a result of abnormalities in the stages of inflammation, proliferation, and remodeling throughout the healing process.1 Up to 70% of burn survivors have HTSs, which are thicker and stiff with reddishness, pain, and pruritus. Typically, these scars appear within the first 2–4 months and gradually become less severe over the next 6–9 months.2
There have been several treatment approaches applied to control scar formation and contracture, including scar revision, compression therapy, tissue expansion, intralesional steroid injection, interferon injection, and laser treatment. However, all these treatment methods have their limitations.3 Recently, laser technology has gained much attraction in dermatology. Three main groups of lasers usually used to improve scars are the pulsed dye lasers, Q-switched neodymium: Yttrium aluminum garnet (Nd: YAG) lasers, and ablative and non-ablative fractional lasers.4 Fractionation of the beam of energy into several microbeams and the fractional carbon dioxide (CO2) laser has the potential for a range of ablative and non-ablative skin rejuvenation processes.5
Fractional CO2 laser has been used as a novel tool for the improvement of HTS, including burn scars. Lasers emit a beam of photons from a CO2 laser which is capable of emitting energy at 10,600 nm. With the introduction of fractional photothermolysis, laser technology has advanced rapidly to perform fractional resurfacing in traumatic scars and is found to be associated with substantial functional and cosmetic benefits. The residual thermal damage caused by the CO2 laser beam helps to ensure a dry field, limits blood loss, and swiftly induces the wound healing and tissue remodeling process. Several case series, and before and after studies have demonstrated the substantial improvement of cosmetic and functional outcomes with the treatment of this method.6-8
Aims and objectives
This study aimed to study the efficacy of fractional CO2 laser-assisted drug delivery (LADD) in the management of post-burn scars.
Inclusion criteria
Patients with post-burn scars who were willing to participate in the study after getting consent signed by the individual or guardian as required were included in the study.
Exclusion criteria
History of undergoing any types of laser treatment in the past, pregnant, or lactating women, any skin infections over the site of laser, keloidal tendency, hypersensitivity to lignocaine and prilocaine, and patients who received any form of treatment within the past 6 months (especially systemic retinoids) were excluded from the study.
MATERIAL AND METHODS
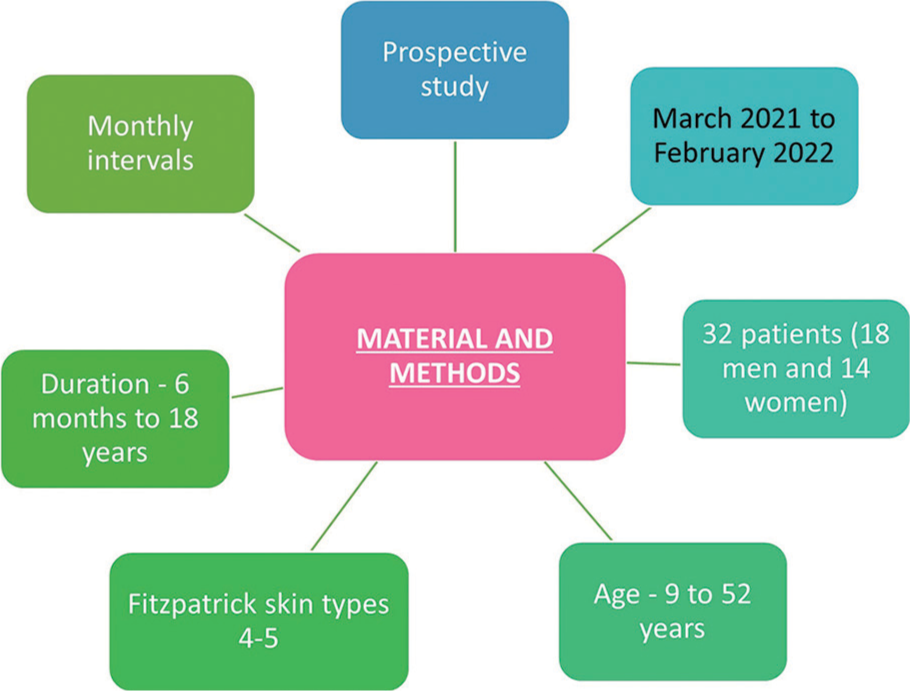
The present study is a prospective study conducted over 1 year period from March 2021 to February 2022 on 32 patients (18 men and 14 women). The patient’s ages ranged from 9 to 52 years and had Fitzpatrick skin types 4–5. The scars of the patients in our study ranged in duration from 6 months to 18 years. Lasers were performed at least 6 months after the initial injury, performed at monthly intervals until the treating physician and the individual or guardian agreed that maximal improvement was made, or 6 sessions were done. Scars were assessed before each treatment by taking clinical photographs and using a validated, comprehensive scale, the modified Vancouver scar scale (mVSS). This scale scores on four domains; pigmentation, vascularity, pliability, and height [Figure 1]. During every subsequent session, documentation was done using clinical photographs and mVSS and compared with the pre-treatment score. Demographic and clinical data collected for each patient included age, sex, Fitzpatrick skin type, and relevant medical history. Information on side effects and responses of patients was collected at each follow-up visit. Clinical evaluations by three blinded dermatologists were obtained using photographs at baseline and at 6 months after the final treatment through mVSS score.
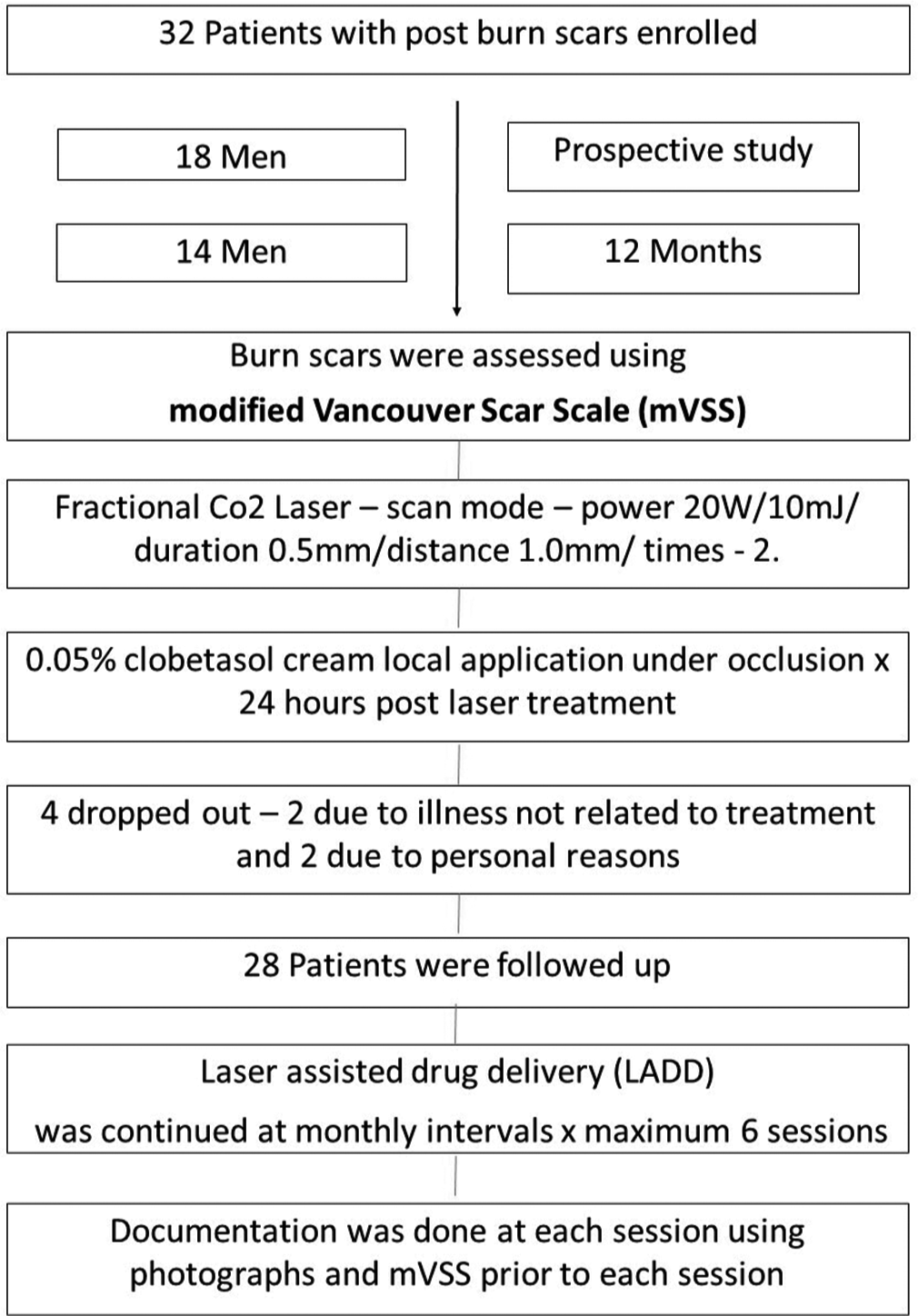
- Image showing the methodology of the study, CO2: carbon dioxide.
Procedure
Before laser treatment, topical anesthetic cream (lignocaine with prilocaine) was applied under occlusion and kept for 1 h. After cleaning the laser treatment area, a fractional CO2 laser was done over the scar. Laser parameters used in our patients include (Dermindia fractional CO2 laser) – scan mode – power 20 W/10 mJ/duration 0.5 mm/distance 1.0 mm/times – 2. Treatment was applied in two passes over the scars. For small scars, the laser area was reduced and a pass was given. Immediately post fractional CO2 passes, 0.05% clobetasol cream was applied over the laser-created microchannels as LADD and was kept under occlusion. The patients were advised to remove the occlusive dressing after 24 hours.
Follow-up
The patients were reviewed after 1 month of the prior session, photographed, and assessed using the mVSS score. This study was conducted per the Declaration of Helsinki 1975 and was approved by the Institution’s Ethics Committee. All patients provided written informed consent to undergo laser treatment and photography.
Statistical analysis
All data was collected and entered in a Microsoft Office Excel sheet. The statistical analysis was performed using the Statistical Package for the Social Sciences 19.0 software. Paired t-test was used for statistical analysis.
RESULTS
In our study, there are 18 males and 14 females [Figure 2], with ages ranging from 09 to 52 years with a mean age of 27 years (Standard deviation [SD] = 10.76). The majority of our patients belonged to Fitzpatrick skin type 5 (17 patients). The duration of scars ranged from 6 months to 18 years, with a median duration of 4 years [Figure 3].
- Image showing the methodology of the study.
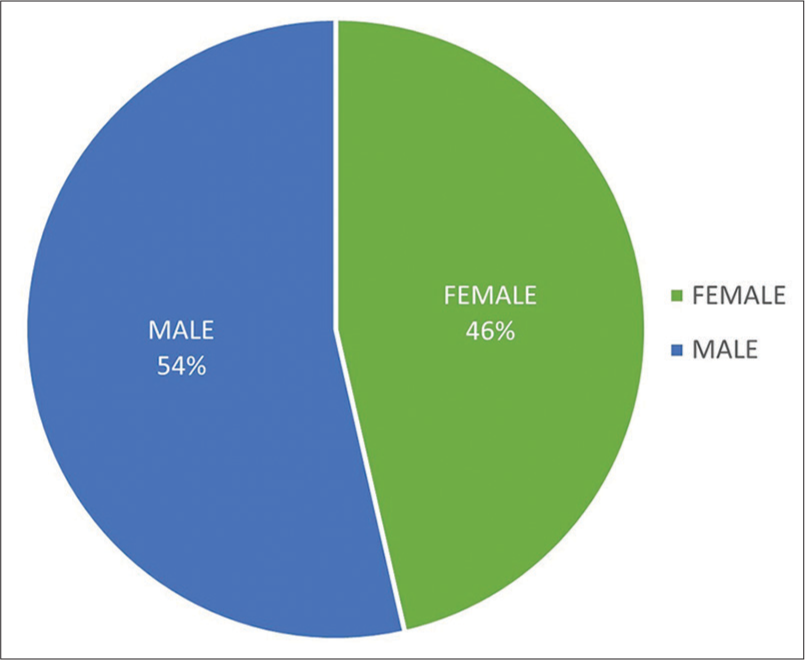
- Pie chart showing male and female distribution.
Among the study group of 32 patients, four patients dropped from the study and did not complete at least four sessions of fractional CO2 laser treatment. Among the four patients, two discontinued due to illness not related to the treatment, and two patients discontinued due to personal reasons not related to the treatment.
Various sites of scars treated in our patients are shown in Figure 4. The forearm was the commonest site with 28% (n = 8) which was treated followed by the hand with 21% (n = 6). Therapeutic response in patients before and after treatment with fractional CO2 laser as mVSS at the time of final assessment is given in Figure 5. At the time of final assessment, a positive response to fractional CO2 laser treatment was observed in all 28 patients.
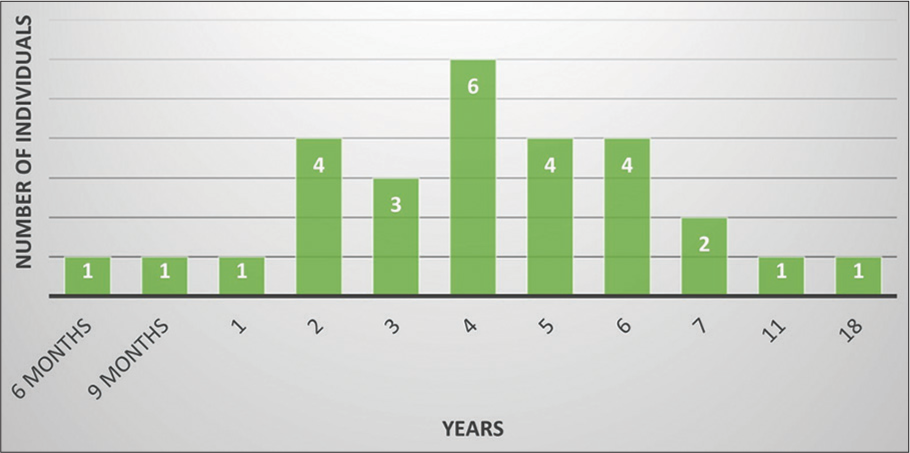
- Clustered column chart showing the duration of scars of patients who underwent fractional carbon dioxide laser.
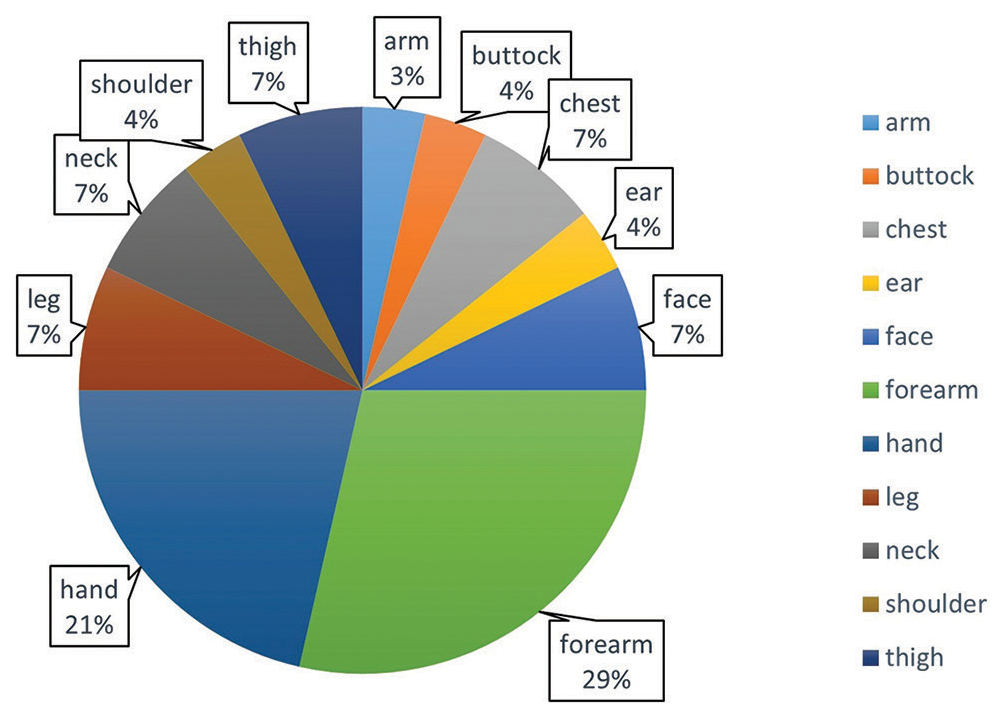
- Pie chart showing the distribution of sites of scar area.
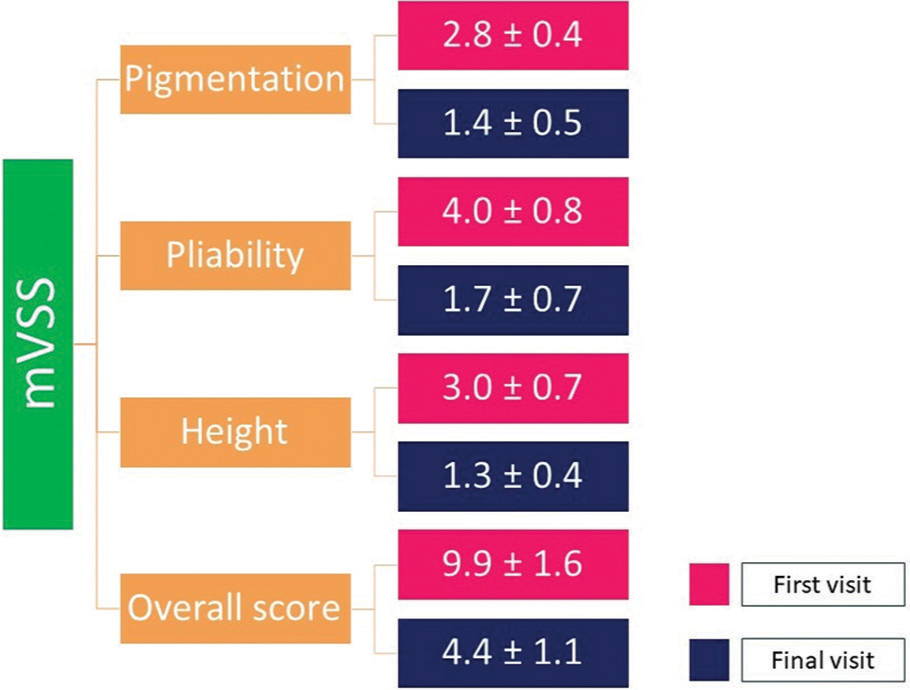
Statistically significant improvements occurred in pigment, thickness, and pliability after the first treatment. These improvements were maintained up to the last laser treatment. The values of mean pigmentation ± SD of pigmentation, pliability, and height at first visit using paired t-test are 2.8 ± 0.4, 4.0 ± 0.8, and 3.0 ± 0.7, respectively. The values of mean pigmentation ± SD of pigmentation, pliability, and height at the final visit using paired t-test are 1.4 ± 0.5, 1.7 ± 0.7, and 1.3 ± 0.4 [Figure 6].
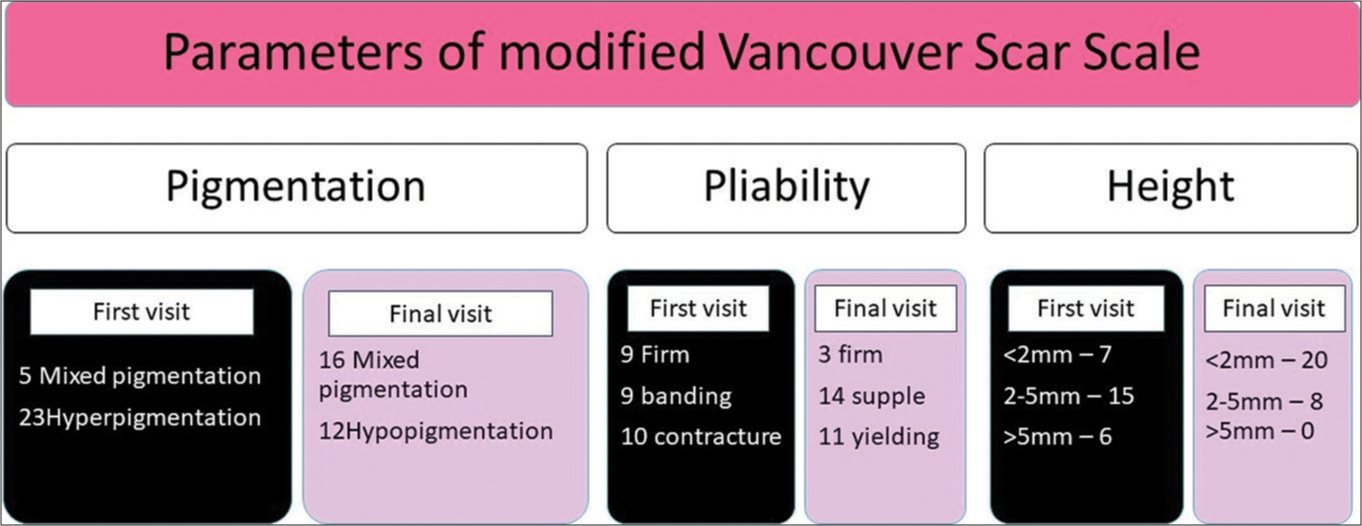
- Image showing various parameters of modified Vancouver scar scale on the first and final visit.
The mean ± SD of the overall mVSS score at the first visit and final visit is 9.9 ± 1.6 and 4.4 ± 1.1 [Figures 7 and 8], respectively. Some of the clinical images showing the pre- and post-burn scars followed by fractional CO2 laser are depicted in Figures 9-12. The correlations between baseline and final visit of pigmentation, pliability, height, and overall mVSS score are 0.404, 0.623, 0.636, and 0.640, respectively. Clinical complaints, such as difficulty in extending the arms or neck due to burn scars, and pruritus significantly improved in the majority of instances beginning with the patient’s second visit. The only complication we noticed in our research was an insignificant occurrence of post-inflammatory hyperpigmentation.
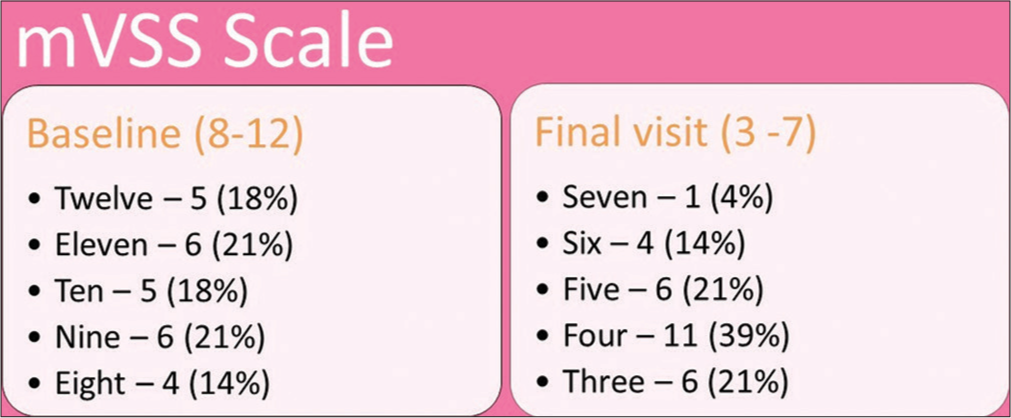
- Modified Vancouver scar scale at baseline and at the final visit.
- Image showing modified Vancouver scar scale parameters on the first and final visit.
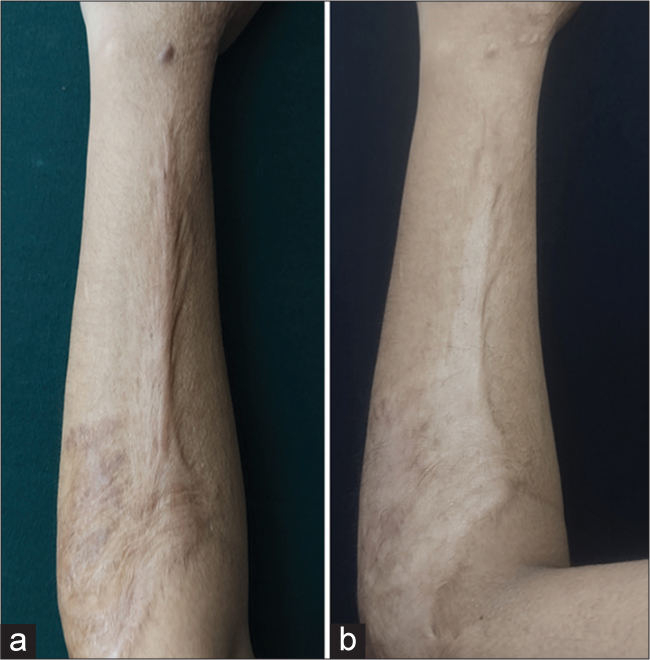
- (a) Pre-clinical image of the post-burn scar and (b) post-clinical image of the post-burn scar over the forearm showing visible improvement in height after 4 visits.

- Pre- and post-burn scar over forearm showing decrease in pigmentation post 3 visits.

- Pre- and post-clinical image of post-burn scar over hand showing improvement in pigmentation and height after 5 visit.
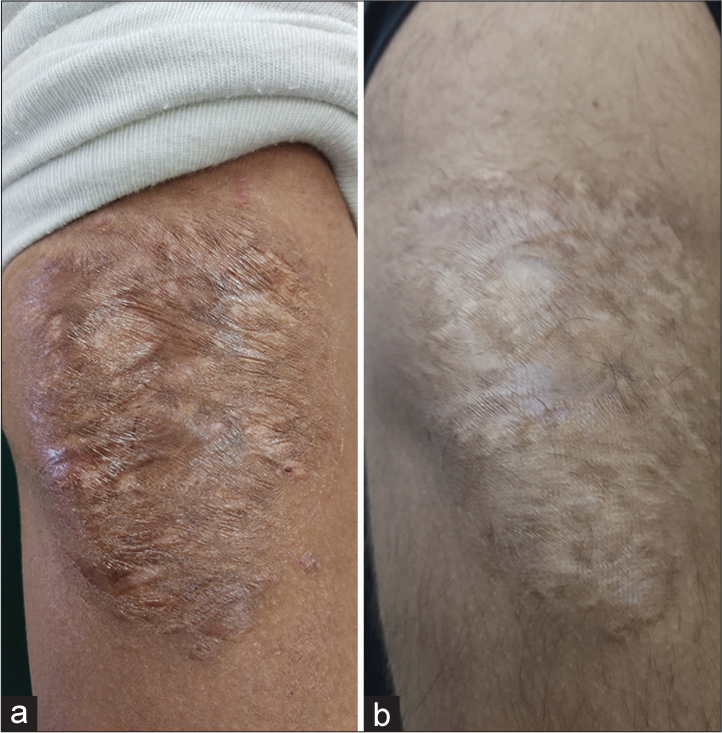
- (a) Pre-clinical image burn scar and (b) post-clinical image burn scar over arm showing a decrease in pliability, pigmentation, and height after 4 visits.
DISCUSSION
HTSs are pathologically abnormal scars that form as a result of burns and traumatic events. After surgery or trauma, there is a 30–50% chance of developing HTSs. Even years after the initial injury, hypertrophic burn scars can cause heat intolerance, neuropathic pain, and pruritus. Functional impairment results from contractures, tightness, and thickness, which are accompanied by physical restrictions and a limited range of motion. The scars left behind by thermal burns are among the most disfiguring scars observed in clinical practice and can have a major negative psychological and esthetic impact.9
The pathological factors that lead to the formation of HTSs remain unknown. The aberrant fibroproliferation in the dermis causes HTSs. Hypertrophy and contraction are typically caused by increased fibrosis and aberrant type I and type III collagen deposition in the dermal layer. Three major categories can be used to group risk factors for HTSs: Burn depth, microbiological load, and location are injury-related factors. Patient-related factors include heredity, race, skin color, and age. Treatment-related aspects include the kind of wound closure, healing duration, and associated wound tension. The presence of a protracted inflammatory state, which can be triggered by a multitude of causes, is one common mechanism for many HTSs.10,11
HTSs have very different mechanical characteristics from healthy skin. The treatment of burn injuries has significantly increased survivability. Application of silicone sheets, pressure dressings, radiation, cryotherapies, surgery, and local or systemic pharmacological agents, such as 5-fluorouracil, bleomycin, analgesics, and corticosteroids, have all been used as treatment techniques to decrease scar development and contracture. It has been established that they are effective; however, the outcomes were much less than expected.12
The barrier function of the skin limits topical substance absorption through the epidermis. Micro-needling, dermabrasion, radiofrequency, and lasers have all been used to improve penetration in a process known as transdermal medication delivery. Transdermal drug delivery (TDD) is the process by which a substance enters the bloodstream or another compartment after passing through the epidermal barrier. To improve TDD, external physical or chemical sources can be employed. LADD, a technique that is becoming more and more popular, uses ablative or non-ablative lasers to destroy or weaken areas of the stratum corneum and epidermis to access the dermis beneath.13 The actual process of using lasers to help deliver drugs involves using lasers on the desired skin area, followed by the application of topical medication. For usage with laser-assisted medication delivery, fractional lasers are frequently researched. These lasers use a fractionated delivery system for their laser beams, creating a large number of vertical channels known as microthermal treatment zones. Laser preparation of the skin can improve drug penetration with both local cutaneous and systemic effects. The dispersion of tiny thermal damage foci is known as micro treatment zones, which can be further divided into non-ablative and ablative fractional photothermolysis.14
Using an ablative fractional laser, such as a CO2 or erbium-doped yttrium aluminum garnet (Er: YAG) laser, to build microscopic channels, LADD allows medications to penetrate the epidermis. Both the Er: YAG and CO2 lasers are ablative, however depending on the biological interaction, they have variable ablation-to-coagulation ratios. Although this also depends on the laser fluence and beam spot size, Er: YAG laser light has a substantially higher absorption coefficient in water than CO2 laser light, resulting in a higher ablation-to-coagulation ratio and shorter depth of penetration. While both lasers are equally effective in allowing therapeutic materials to pass through the stratum corneum, the CO2 laser is preferred over the Er: YAG laser for more penetrative beam dermal delivery of drugs due to its deeper beam profile and coagulative zone.15
This method allows for the penetration of high molecular weight substances into the stratum corneum. The stratum corneum is the first layer of skin to experience tissue destruction when using the ablative fractional laser technique. The laser parameters used determine the depth of the tissue that is destroyed. A microscopic treatment zone surrounds the channel formed through the skin, allowing topical molecules to penetrate the treated skin layer and hasten healing with reduced scarring.16,17
Lasers release a beam of photons from a substance in the instance of a CO2 laser, CO2 that can emit energy at a wavelength of 10,600 nm. If utilized properly, the CO2 laser offers a wide variety of dermatological indications with excellent precision for incision, excision, vaporization, and coagulation treatments. The improvement of atrophic and HTSs caused by non-ablative fractional lasers may be caused by focal dermal heating in the microthermal zone, which sets off a chain of events that normalizes the cycle of collagen synthesis and lysis.18,19
According to the theory, the laser separates the disordered collagen fibrils that cause the contracture, and as a result, the body tends to repair the wound more efficiently. Type I and III procollagen, matrix metalloproteinase-1, transforming growth factor-b2/-b3, beta-fibroblast growth factor, and miR-18a and miR-19a expressions are all changed by a fractional CO2 laser beam on a scar. In the early remodeling stage of human skin, fractional CO2 laser also promotes the expression of the Wnt5a, CYR61, and HSP90 genes.20
According to Zhang et al. meta-analysis study, fractional CO2 laser treatment for burn scars is an efficient technique to enhance both function and appearance. After treatment, there were notable improvements in the Vancouver scar scale (VSS) and patient and observer scar assessment scale (POSAS) scores, particularly in the areas of pigmentation, vascularity, pliability, and scar height. With this therapy, pruritus and pain also became better. The use of a fractional CO2 laser has been linked to a considerable reduction in type I collagen and an increase in type III collagen, as well as an enhanced architectural dermal layer with finer and more fibrillar collagen.21
According to a study by Keen et al., 53.75% of patients who underwent fractional CO2 laser treatment for post-burn and post-traumatic scars had great results, 16.25% of patients had good results, and 30% of patients had poor results.22
The VSS score and the POSAS score were both considerably improved by fractional CO2 laser therapy, according to Peng et al. meta-analysis study to evaluate the efficacy and safety of fractional CO2 laser in burn scars. Scar thickness assessed through ultrasonography was significantly reduced by fractional CO2 laser. The pigmentation, vascularity, pliability, scar height, vascularity, and relief all showed significant improvements.23
According to Miletta et al. multicentric prospective study, there were statistically significant improvements in elastic stretch, elastic recovery, extensibility, and thickness in adult hypertrophic burn scars treated with fractional ablative CO2 laser for HTSs. Scar appearance and pain/pruritus as reported by both patients and physicians have considerably improved.24
The objectively evaluated thickness, pliability erythema, and pigmentation of the treated scars dramatically improved in the Blome et al. prospective study to assess fractional CO2 laser treatment of adult scars. Although elasticity increased, it was not statistically significant. Independent observer evaluations of the VSS decreased from 8 to 6, although patient self-reported pain and pruritus remained constant in both groups.25
In a study by Lee et al. on dermal remodeling of burn scars, all patients showed clinical improvement in their scars with a significant decrease in VSS. Histologic findings showed the changes in the upper dermis with newly formed dermal papilla. This characteristic upper dermis change was presented as an improvement in surface smoothness and skin tension clinically. Post-inflammatory hyperpigmentation and itching sensation were the most common adverse effects.26
The uniqueness of our study compared to the previous studies is creating numerous microchannels using fractional CO2 laser and application of a single time 0.05% clobetasol cream under occlusion for 24 h. Clobetasol administered once under occlusion is less expensive, effective, and has fewer side effects. Our study demonstrated a notable improvement in the scar’s height, pliability, and color as measured by the mVSS score. At the final visit, the mean ± SD of the overall mVSS score dropped from 9.9 ± 1.6 at the initial visit to 4.4 ± 1.1 which is very significant compared to the previous studies done in the management of post-burn scars using fractional CO2 lasers. The aggregate mVSS score’s correlation between the first and last visits is 0.640.
Smaller population size, patients with different etiologies such as burns induced by hot water, electric injuries, and chemical burns, scar location and kind, diverse population, semi-fixed duration, and energy settings for all patients are some of the limitations of our study. Despite these drawbacks, our study shows that fractional CO2 laser significantly improves the contour of the deep scar brought on by post-burn cause.
CONCLUSION
The contour of post-burn scars can be improved with a fractional CO2 laser, which is a safe, well-tolerated, and efficient modality. It offers a safer alternative to invasive therapies and a powerful substitute for several prevalent conventional conservative management techniques for HTSs. Future research on the use of fractional CO2 lasers should include a bigger sample size and long-term follow-up in a population that is homogeneous with a variety of subgroups.
Author’s Contributions
All authors contributed to the research Study. Shekhar Neema: Concepts, Definition of intellectual content, Data acquisition, Manuscript preparation. Senkadhir Vendhan: Concepts, Definition of intellectual content, Literature search, Manuscript editing and review. Biju Vasudevan: Definition of intellectual content, Literature search, Manuscript preparation. Lekshmipriya K.: Concepts, Definition of intellectual content, Manuscript review. Senkadhirdasan Dakshinamurthy: Results analysis, Manuscript review and editing.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki 1975 and was approved by the Institution’s Ethics Committee. The Study is conducted in the department of Dermatology at Armed Forces Medical College, Pune, Number- 2021/5, and dated 10/02/2021.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Hypertrophic scarring and keloids: Pathomechanisms and current and emerging treatment strategies. Mol Med. 2011;17:113-25.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertrophic scarring: The greatest unmet challenge after burn injury. Lancet. 2016;388:1427-36.
- [CrossRef] [PubMed] [Google Scholar]
- Keloids: A review of etiology, prevention, and treatment. J Clin Aesthet Dermatol. 2020;13:33-43.
- [Google Scholar]
- Current laser resurfacing technologies: A review that delves beneath the surface. Semin Plast Surg. 2012;26:109-16.
- [CrossRef] [PubMed] [Google Scholar]
- The role of the CO2 laser and fractional CO2 laser in dermatology. Laser Ther. 2014;23:49-60.
- [CrossRef] [PubMed] [Google Scholar]
- The use of CO2 fractional photothermolysis for the treatment of burn scars. J Burn Care Res. 2016;37:106-14.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of fractional CO2 laser resurfacing in non-hypertrophic traumatic and burn scars. J Cutan Aesthet Surg. 2015;8:159-64.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of fractional carbon dioxide laser in the treatment of mature burn scars: A clinical, histopathological, and histochemical study. J Clin Aesthet Dermatol. 2017;10:36-43.
- [Google Scholar]
- The roles of inflammation in keloid and hypertrophic scars. Front Immunol. 2020;11:603187.
- [CrossRef] [PubMed] [Google Scholar]
- The molecular mechanism of hypertrophic scar. J Cell Commun Signal. 2013;7:239-52.
- [CrossRef] [PubMed] [Google Scholar]
- Genetic risk factors for hypertrophic scar development. J Burn Care Res. 2013;34:477-82.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertrophic scar formation following burns and trauma: New approaches to treatment. PLoS Med. 2007;4:e234.
- [CrossRef] [PubMed] [Google Scholar]
- Skin barriers in dermal drug delivery: Which barriers have to be overcome and how can we measure them? Pharmaceutics. 2020;12:684.
- [CrossRef] [PubMed] [Google Scholar]
- Update of ablative fractionated lasers to enhance cutaneous topical drug delivery. Adv Ther. 2017;34:1840-9.
- [CrossRef] [PubMed] [Google Scholar]
- Lessons learned from the first decade of laser-assisted drug delivery. Dermatol Ther (Heidelb). 2021;11:93-104.
- [CrossRef] [PubMed] [Google Scholar]
- Ablative fractional resurfacing in topical drug delivery: An update and outlook. Dermatol Surg. 2013;39:839-48.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional carbon dioxide laser resurfacing. Semin Plast Surg. 2012;26:125-30.
- [CrossRef] [PubMed] [Google Scholar]
- Improvement of burn scars treated with fractional ablative CO2 lasers-a systematic review and meta-analysis using the Vancouver scar scale. J Burn Care Res. 2021;42:200-6.
- [CrossRef] [PubMed] [Google Scholar]
- Characterization of microthermal zones induced by fractional radiofrequency using reflectance confocal microscopy: A preliminary study. Lasers Surg Med. 2013;45:503-8.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of multiple modes of UltraPulse fractional CO2 laser treatment on extensive scarring: A retrospective study. Lasers Med Sci. 2022;37:1575-82.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of fractional CO2 laser therapy combined with hyaluronic acid dressing for treating facial atrophic acne scars: A systematic review and meta-analysis of randomized controlled trials. Lasers Med Sci. 2023;38:214.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of post-burn and post-traumatic atrophic scars with fractional CO2 laser: Experience at a tertiary care centre. Lasers Med Sci. 2018;33:1039-46.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy and safety of fractional CO2 laser therapy in the treatment of burn scars: A meta-analysis. Burns. 2021;47:1469-77.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional ablative laser therapy is an effective treatment for hypertrophic burn scars: A prospective study of objective and subjective outcomes. Ann Surg. 2021;274:e574-80.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective evaluation of fractional CO2 laser treatment of mature burn scars. J Burn Care Res. 2016;37:379-87.
- [CrossRef] [PubMed] [Google Scholar]
- Dermal remodeling of burn scar by fractional CO2 laser. Aesthetic Plast Surg. 2016;40:761-8.
- [CrossRef] [PubMed] [Google Scholar]







