Translate this page into:
Efficacy of Fractional Carbon Dioxide Laser (FCO2) with Intralesional 5-Fluorouracil (5-FU) in the Treatment of Keloids
Address for correspondence: Dr. Nabeel K. Alhamzawi, Department of Dermatology, Diwaniyah Teaching Hospital, Diwaniyah, Iraq. E-mail: alhamzawi_n@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Context:
Managing keloids remains a challenge in clinical practice. Many therapeutic options are available, but none is universally accepted or without recurrence. Therefore, an effort is required to choose the treatment with maximal outcomes.
Aims:
To evaluate the effectiveness of combining fractional carbon dioxide (FCO2) laser and intralesional 5-fluorouracil (5-FU) for the treatment of keloids.
Materials and Methods:
In this prospective open-label study, 24 patients received FCO2 laser treatment, started at baseline, for a total of six sittings. The patients also received 1 mL/cm2/keloid of 5-FU (50 mg/mL) intralesionally, following irradiation, at identical time points. The primary outcome evaluated was the clinical response concerning height, pliability, vascularity, and pigmentation, using the Vancouver Score Scale (VSS). Adverse reactions and recurrences were recorded as secondary outcomes.
Results:
A significant reduction was observed in the VSS in terms of pliability and height after three treatment sessions. The mean VSS reduction was 65%, from 8.45 ± SD 0.93 at baseline to 3 ± SD 1.8 one month after the last treatment (P < 0.05). Most patients (79.1%; n = 19) showed a satisfactory response to treatment, with 57.8% (n = 11) achieving an excellent result. Adverse reactions included post-inflammatory hyperpigmentation in four patients and ulceration in two. Recurrences were reported in 21% of the patients who responded well.
Conclusions:
Combination therapy with FCO2 laser and intralesional 5-FU showed a promising effect in the treatment of resistant keloids, with an acceptable safety profile and low recurrence rate.
Keywords
5-Fluorouracil
fractional CO2 laser
intralesional
keloid
INTRODUCTION
Keloid is a firm growth that results from abnormal wound healing in response to trauma or inflammation. Genetic and environmental factors may contribute to the development of keloids.[1] They are seen most commonly on the pre-sternal areas, shoulders, upper back, earlobes, but they can occur anywhere. Keloids are firm, fibrous nodules, red to dark brown, and sometimes accompanied by pain or severe itching.[2] The best treatment is prevention in patients with predisposed risks. The therapeutic strategies include pressure therapy, topical silicone, radiation, intralesional corticosteroids, interferon, fluorouracil, and laser.[34]
Nonablative types of lasers include 980-diode, Nd: Yag, and pulse dye laser have been investigated in the treatment of keloids with conflicting results.
5-FU is a fluorinated pyrimidine analog with antimetabolite activity, and both in vitro and in vivo experiments have shown that 5-FU can inhibit fibroblastic proliferation. Moreover, it has an inhibitory effect on TGF-β induce expression of the type 1 collagen gene and is believed to reduce postoperative scarring by decreasing fibroblast proliferation.[567]
Ablation of keloids with a fractional CO2 laser (10,600nm) can result in selective thermolysis of the dermal layer of the skin by creating microthermal zones MTZ. It increases the temperatures of skin layers to 70°C, resulting in denaturation and irreversible coagulation of dermis proteins, without affecting the epidermal layer.[89]
The surrounding healthy tissue helps in the remodeling, starting with a molecular cascade. Heat shock proteins, metalloproteinases, and inflammatory cytokines are activated during the healing process 48 h following laser to compensate the vaporized columns with epidermal cells and restoring skin continuity.[1011] Collagen remodeling results in the formation of new collagen with a decrease of collagen type I and an increase in type III.[12] The newly formed collagen type III has the ability to change the architecture of the dermis by increasing pliability, decreasing thickness, and improving molecular function.[1213] Thus, it leads to the improvement of the surface of unstable chronic scars.[131415] The present study aimed to evaluate the efficacy and safety of combining fractional CO2 laser and intra-lesional 5FU for the treatment of keloids.
SUBJECTS AND METHODS
An open-label prospective interventional trial was carried out among 24 patients to evaluate the efficacy and safety of FCO2 laser and intralesional 5-FU for the treatment for keloids. Approval was obtained from the local medical committee and written consent signed by all participants.
The inclusion criteria were
Clinically diagnosed keloids
Duration of keloids >1 year
Patient age ranged from 18 to 65 years
A healthy person who has no serious illness
Those willing for treatment and regular follow-up
No topical or intralesional therapy for the last 6 months.
The exclusion criteria include
Patients <18 years and elderly
Patients not willing to regular follow-up
Medical illness of bone marrow, liver, and renal diseases
Pregnant and lactating women
Those who received topical or intralesional therapy within the last 6 months.
In total, 24 patients, each with one to three keloid scars, were enrolled for this study. The patient received 1 mL/cm2 /lesion of 5-FU (50 mg/mL) intralesionally, with a maximum dose of 150 mg/session. The treatment was given with a 1-month interval, for a maximum of six sittings.
Topical lidocaine ointment (Emla) was applied 30 min before the treatment, to achieve local anesthesia. Each keloid was irradiated with FCO2 laser, fluence 20 mJ, distance 0.6 mm, moving time 1s, perpendicularly. 5-FU (1 mL/cm2) was infiltrated into each lesion until complete blanching observed, using a 27-gauge syringe.
Analysis of laboratory profiles was done to monitor the changes in the liver, renal, and bone marrow functions before and every month after the procedure.
Evaluation of the response to the treatment was subjectively made using VSS, which incorporates the subsequent parameters (height, pliability, vascularity, and pigmentation). The height was measured using a caliber. Pliability was evaluated by palpation and labeled as soft, semi-solid, and solid. Vascularity was labeled as normal, pink, red, and purple, and pigmentation was labeled as hypopigmented, skin color, and hyperpigmented by inspection. The evaluation was done at four points: the baseline, 2 months, 4 months, and 6 months. The objective assessment of pain and pruritus was done at an equivalent time.
The response was measured by calculation of the percentage of changes in VSS before and after treatment, and labeled as follows: 0 = No change, 1–25% = poor, 26–50% = good, 51–75% = very good, 76–100% = excellent. The satisfactory result was assigned for patients who achieved >50% changes in VSS, and unsatisfactory result for those exhibited <50%. Adverse reactions were recorded during and after treatment, and follow-up continued for one year to assess the recurrence rate.
Vancouver score scale
A tool evaluated the changes in the appearance of the scars, using the parameters such as height, vascularity, pliability, and pigmentation to determine the score. The maximum score is 13, calculated as follows; pliability 0–5, height 0–3, vascularity 0–3, and pigmentation 0–2. Clinical improvement in the scar was assessed by decreasing the mean values of the score.[1617]
Data were analyzed using SPSS software version 26, by IBM, Chicago, USA. Data were defined as mean, standard deviation, number, and percentage. A paired t-test was used to study the rate of changes in the VSS before and after treatment. Spearman’s correlation was used to determine the association between the changes in the VSS and patient age and duration of the keloid. P < 0.05 was considered significant.
RESULTS
Twenty-four patients were enrolled in this study, aged from 16 to 58 years (mean 24.25 ± SD 9.49 years). The sex ratio was 1.4:1, with 14 males and 10 females.
The keloid etiology was surgery in 11 cases, ear piercing in 5, burn-in 4, trauma in 2, and aggressive salabrasion for tattoo removal in 2. The duration of keloids ranged from 14 to 48 months (mean 31.25 ± SD 11.6 months). A positive family was reported in three patients (12.5%). The majority of participants (79.1%) had Fitzpatrick skin type IV [Table 1].
| Demographic | n (%) |
|---|---|
| Number | 24 |
| Age | |
| Range | 16–58 |
| Mean | 24.25 |
| Gender (M/F) | 14/10 |
| Ratio | 1.4/1 |
| Number of keloids | 44 |
| 8 patients | 1 for each |
| 12 patients | 2 for each |
| 4 patients | 3 for each |
| Duration of disease | |
| Range | 14–48 months |
| Mean | 31.25 ± SD 11.6 |
| Fitzpatrick skin | |
| Type III | 1 (4.16) |
| Type IV | 19 (79.1) |
| Type V | 4(16.6) |
| Etiology | |
| Surgery | 11 |
| Ear piercing | 5 |
| Burn | 4 |
| Trauma | 2 |
| Salabrasion | 2 |
| Family history | 3 (12.5) |
A total of 44 keloid lesions were investigated in the 24 patients: 25 lesions in males and 19 in females. The majority of patients (83.3%) had either one or two lesions [Table 2].
| keloids/ patient | Male | female | % |
|---|---|---|---|
| One | 5 | 3 | 33.3 |
| Two | 7 | 5 | 50 |
| Three | 2 | 2 | 16.6 |
Most keloids (61.3%) were located on the chest or shoulders, with others distributed on the back, ears, and upper arms [Table 3]. Itching was reported in 13 participants (54%), particularly those with presternal or earlobe keloids.
| Site | No. of keloids | % |
|---|---|---|
| Chest | 16 | 36.3 |
| Shoulders | 11 | 25 |
| Back | 7 | 15.9 |
| Ear | 7 | 15.9 |
| Upper arms | 3 | 6.8 |
The VSS was markedly reduced after three treatment sessions, particularly in height and pliability [Figures 1,2,3]. The mean VSS was reduced by 65%, from 8.45 ± SD 0.93 at the baseline to 3 ± SD 1.8 one month after the end of treatment (P < 0.05). The most obvious changes were in pliability for all patients. Other changes included a reduction in lesion height in 83%, vascularity in 20.8%, and pigmentation in (16.6%) of the patients. The majority of patients (79.1%; n = 19) showed a satisfactory response to treatment, with 57.8% (n = 11) achieving an excellent results [Table 4].
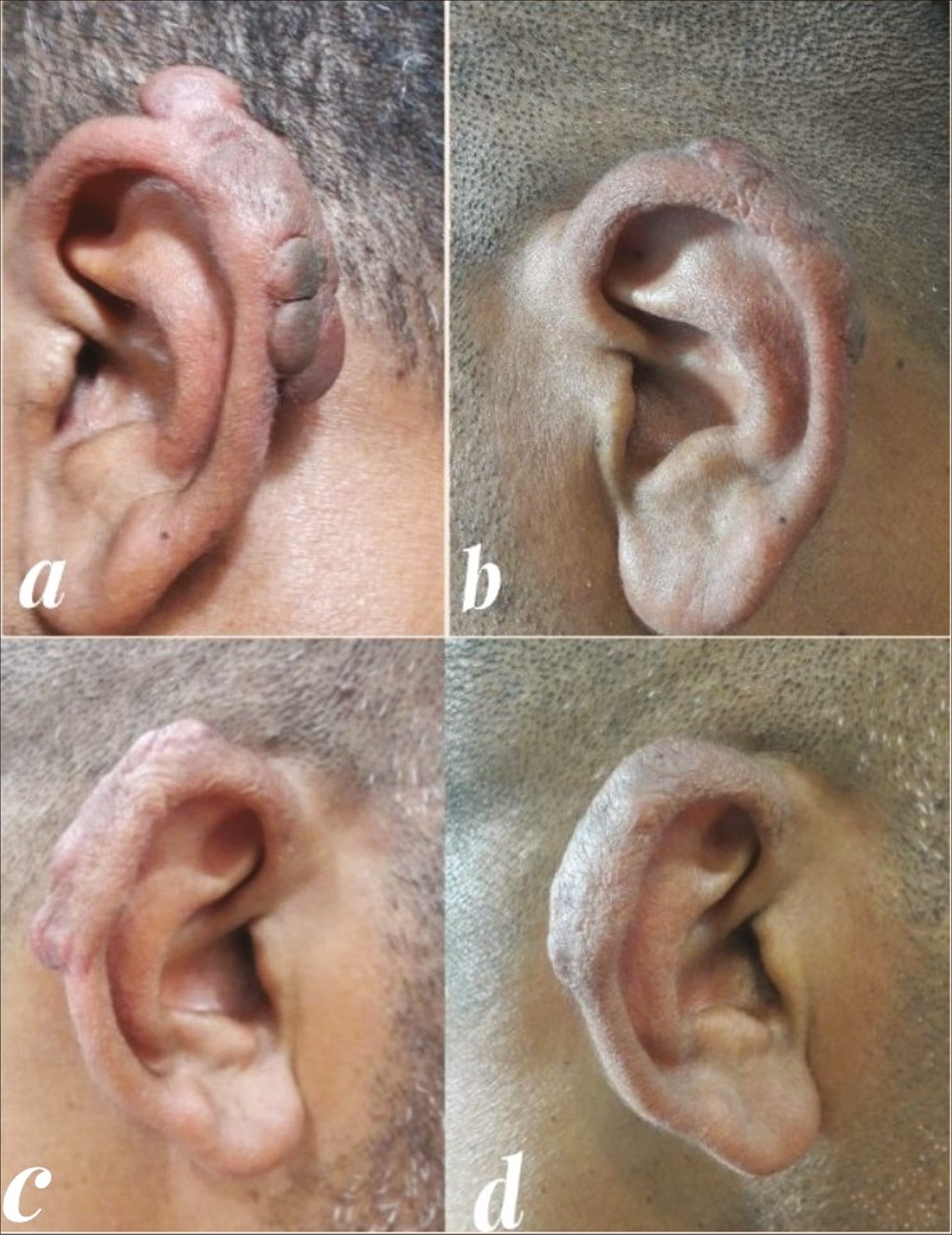
- Bilateral earlobe keloids showed a satisfactory response to treatment after six sittings of combining FCO2 laser and intralesional 5-FU
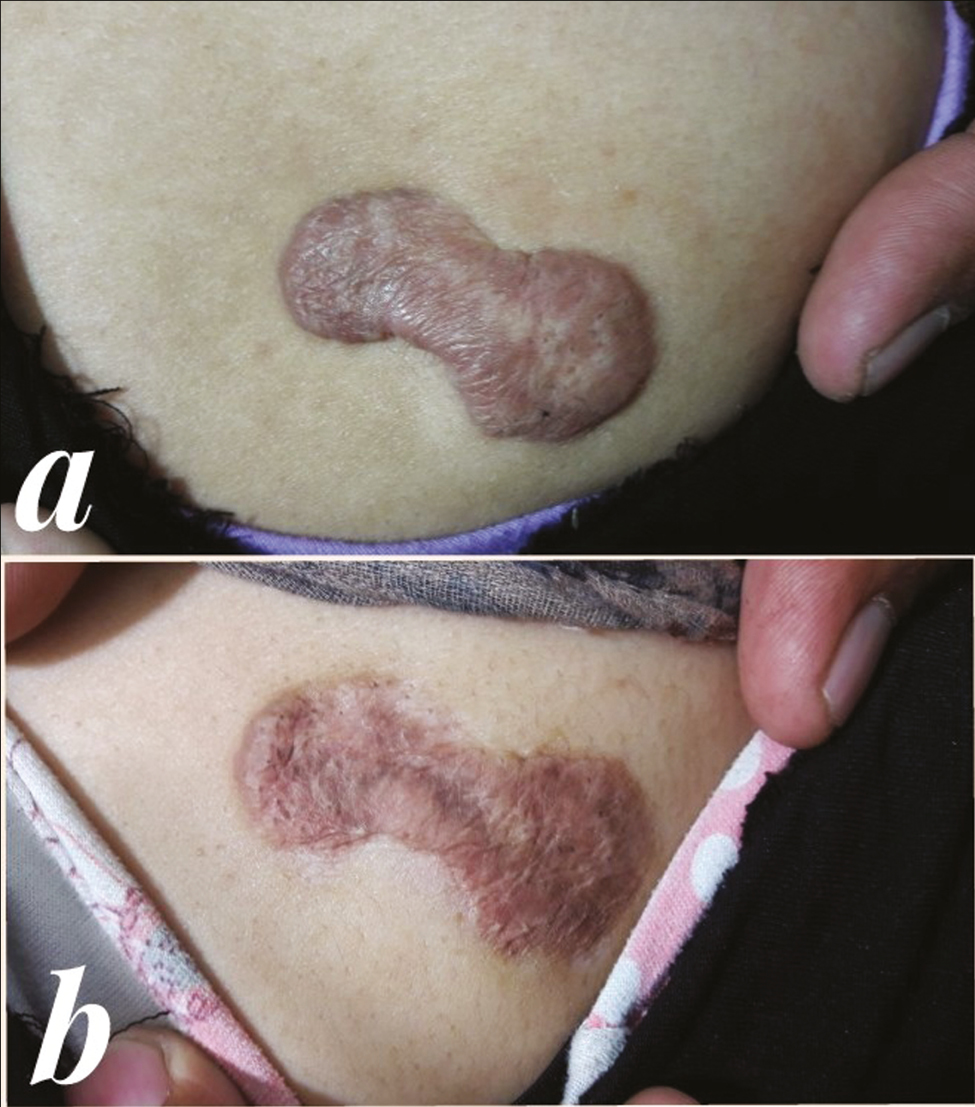
- (A) A fionke-shaped keloid in the upper back of 26-year-old female. (B) Complete flattening of keloid after treatment with post-inflammatory hyperpigmentation

- (A) Keloid developed after piercing the ear. (B) Excellent response to the treatment following six sessions
| Age | Gender | Duration | VSS before | VSS after | % of changes | Grade |
|---|---|---|---|---|---|---|
| 37 | M | 16 | 10 | 2 | 80% | Excellent |
| 26 | M | 23 | 9 | 3 | 66.6% | Very good |
| 16 | M | 27 | 9 | 4 | 55.5% | Very good |
| 32 | F | 30 | 8 | 3 | 62.5% | Very good |
| 22 | M | 18 | 8 | 3 | 62.5% | Very good |
| 26 | F | 25 | 9 | 2 | 77.7% | Excellent |
| 19 | F | 14 | 7 | 1 | 85.7% | Excellent |
| 18 | M | 23 | 9 | 2 | 77.7% | Excellent |
| 19 | F | 22 | 7 | 1 | 85.7% | Excellent |
| 21 | F | 27 | 9 | 2 | 77.7% | Excellent |
| 23 | M | 38 | 8 | 1 | 87.5% | Excellent |
| 16 | M | 34 | 9 | 5 | 44.4 | Good |
| 20 | M | 36 | 8 | 1 | 87.5 | Excellent |
| 24 | F | 30 | 7 | 3 | 57.14 | Very good |
| 22 | F | 26 | 7 | 2 | 71. 4 | Very good |
| 19 | M | 22 | 8 | 5 | 37.5 | Good |
| 25 | M | 36 | 8 | 2 | 75 | Very good |
| 58 | F | 60 | 8 | 3 | 62.5 | Very good |
| 20 | M | 25 | 9 | 2 | 77.7 | Excellent |
| 18 | M | 32 | 9 | 6 | 33.3 | Good |
| 41 | F | 54 | 10 | 2 | 80 | Excellent |
| 19 | M | 45 | 8 | 6 | 25 | Poor |
| 18 | M | 39 | 9 | 2 | 77.7 | Excellent |
| 23 | F | 48 | 10 | 8 | 20 | Poor |
A significant correlation was seen between the changes in VSS and duration of keloids: 13 out of 19 patients (68.4%) with a satisfactory response had a keloid duration of under 3 years (P < 0.05). No significant correlation was found with the age of the patients (P = 0.063) [Figure 4].
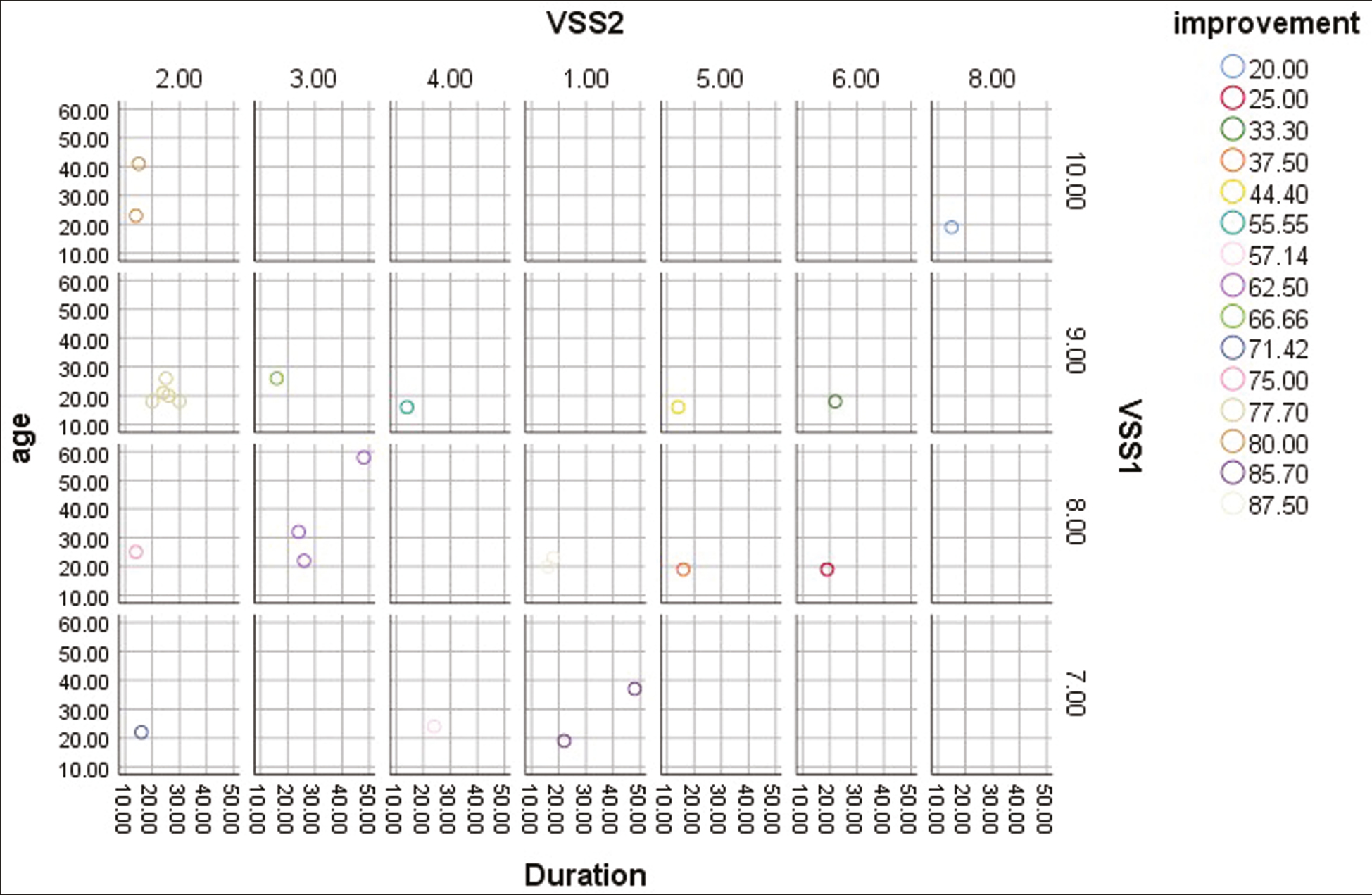
- Changes in VSS in relation to the patient age and duration of keloid
Adverse reactions such as pain, redness, and edema were transient, lasting no more than a week.
Post-inflammatory hyperpigmentation and skin erosion were observed in some patients [Table 5]. No laboratory changes were recorded throughout the treatment course. The itching was resolved in patients experiencing it before treatment. Recurrences after a follow-up of 1 year were reported in four (21%) of those who responded well.
| Adverse effect | Frequency |
|---|---|
| Pain | 5/24 |
| Telangiactsia | 0 |
| Atrophy | 0 |
| Pigmentation | 4/24 |
| Ulceration | 2 |
DISCUSSION
Keloid treatment remains a challenge in clinical practice. Keloids may lead to cosmetic and psychological embarrassment for patients. Many treatment options are available, but none are universally effective or without adverse reactions. By understanding how keloids are formed, appropriate medications can be chosen to address the causes and determine which is most effective. The pathogenesis of keloids includes the formation of excessive collagen and other extracellular matrix components. 5-FU may inhibit the synthesis of type 1 collagen, the main structural protein of scar tissue. Published data about 5-FU indicate a scheduled dose ranging from 50 to 150 mg, weekly for eight to 16 weeks. These doses are considered safe because they are small compared to intravenous chemotherapy.[1819] Intralesional 5-FU has been tried in combination with other medications to treat keloids, with excellent results.[20]
CO2 lasers target water molecules to cause local tissue changes, including collagen remodeling, increased fibroblast growth factor, and decreased TGF-β expression. Moreover, frequent treatments with FCO2 laser have been shown to reduce keloids, primarily in terms of pliability.[15]
Evidence suggests that the use of FCO2 laser with an adjuvant medication, as fractional laser-assisted therapy, can enhance drug delivery and potentiate the clinical efficacy of the applied drug.[2122] Given this, some research studies have described the use of topical 5-FU in combination with FCO2 for keloids. Irradiation of the keloid lesion with the laser before the application of 5-FU can lead to a uniform distribution of the drug within the vaporized tissue columns created.[232425] A further benefit of this combination therapy is the administration of a low dose of medication to reduce undesirable adverse effects. Waibel et al. investigated laser-assisted topical 5-FU versus laser-assisted topical corticosteroid, finding no significant difference in efficacy, and determining that 5-FU had fewer adverse effects such as dermal atrophy and telangiectasia compared to the standard treatment of triamcinolone acetonide.[22] Because the drug can diffuse more easily when used intralesionally than topically, the current study used the intralesional mode to apply 5-FU before irradiation of the keloid with FCO2. FCO2 laser creates coagulation and carbonization in the vaporized columns, which makes diffusion of the topical drug to the target tissue more difficult.
Compared to the recurrence rate of 21% in this study, other studies that used either FCO2 laser or 5-FU as monotherapy for keloids found 95% and 35% recurrence, respectively, at a minimum of 3 months.[2627]
Care after treatment was required to promote rapid healing and epithelialization of damaged tissue. A daily moisturizing ointment was applied for 1 week. The patients were advised to use sunscreen on exposed treated areas. Side effects of this treatment such as pain, pruritus, redness, and local edema were transient and subsided within a few days. Other side effects such as infection, ulceration, and hyperpigmentation were not clinically significant.
Multimodal therapy was used to treat relapsing keloids including the addition of intralesional triamcinolone acetonide to the 5-FU following irradiation of the lesion with the FCO2 laser. In addition, silicone gel was prescribed to use throughout the treatment course. It is thought that compression therapy work by reducing blood supply to the keloid tissue, resulting in hypoxia of fibroblast and increase activity of collagenase enzyme that lead to more degradation of collagen fibers.
This novel modality of laser-assisted drug delivery with intralesional 5-FU has several advantages: (1) it shortens the treatment course and reduces the number of sessions, (2) it creates a more synergistic effect on the fibrous tissue of keloids, (3) it reduces the need for large doses of the drug, and (4) it reduces the side effects, such as hyperpigmentation and ulceration.
The majority of patients exhibited a satisfactory response to combining FCO2 laser with intralesional 5-FU for the treatment of keloids, with a low rate of recurrence. The greatest reduction was seen in pliability and height, with the least changes in vascularity and color. The modality was tolerated by the patients, and adverse reactions were transient and subsided without treatment.
CONCLUSION
Encouraging results were seen after six treatment sessions combining FCO2 laser and intralesional 5-FU for the treatment of keloids. The treatment exhibited high safety and tolerability profiles.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Keloid research: Current status and future directions. Scars Burn Heal. 2019;5:2059513119868659.
- [Google Scholar]
- The most current algorithms for the treatment and prevention of hypertrophic scars and keloids. Plastic Reconstr Surg. 2010;125:557-68.
- [Google Scholar]
- Hypertrophic scars and keloids: Etiology and management. Am J Clin Dermatol. 2003;4:235-43.
- [Google Scholar]
- Up-to-date approach to manage keloids and hypertrophic scars: A useful guide. Burns. 2014;40:1255-66.
- [Google Scholar]
- 5-fluorouracil treatment of problematic scars. Plast Reconstr Surg. 2009;123:139-48; discussion 149-51.
- [Google Scholar]
- Antimitotic drug injections and radiotherapy: A review of the effectiveness of treatment for hypertrophic scars and keloids. Int J Low Extrem Wounds. 2008;7:151-9.
- [Google Scholar]
- Intralesional 5-fluorouracil as a treatment modality of keloids. Dermatol Surg. 2004;30:54-6; discussion 56-7.
- [Google Scholar]
- Laser modulation of hypertrophic scars: Technique and practice. Clin Plast Surg. 2017;44:757-66.
- [Google Scholar]
- In vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med. 2007;39:96-107.
- [Google Scholar]
- Inflammatory responses, matrix remodeling, and re-epithelialization after fractional CO2 laser treatment of scars. Lasers Surg Med. 2017;49:675-85.
- [Google Scholar]
- Evaluation of clinical results, histological architecture, and collagen expression following treatment of mature burn scars with a fractional carbon dioxide laser. JAMA Dermatol. 2013;149:50-7.
- [Google Scholar]
- Clinical and molecular effects on mature burn scars after treatment with a fractional CO(2) laser. Lasers Surg Med. 2012;44:517-24.
- [Google Scholar]
- Ablative CO2 fractional resurfacing in treatment of thermal burn scars: An open-label controlled clinical and histopathological study. J Cosmet Dermatol. 2015;14:324-31.
- [Google Scholar]
- Treatment of hypertrophic scars and keloids by fractional carbon dioxide laser: A clinical, histological, and immunohistochemical study. Lasers Med Sci. 2016;31:9-18.
- [Google Scholar]
- The Vancouver Scar Scale: An administration tool and its interrater reliability. J Burn Care Rehabil. 1995;16:535-8.
- [Google Scholar]
- Intralesional 5-fluorouracil in keloid treatment: A systematic review. Acta Derm Venereol. 2015;95:778-82.
- [Google Scholar]
- A review of the effectiveness of antimitotic drug injections for hypertrophic scars and keloids. Ann Plast Surg. 2009;63:688-92.
- [Google Scholar]
- Efficacy of intralesional 5-fluorouracil and triamcinolone in the treatment of keloids. Aesthetic Surg J. 2009;29:40-6.
- [Google Scholar]
- Treatment of keloids with laser-assisted topical steroid delivery: A retrospective study of 23 cases. Dermatol Ther. 2015;28:74-8.
- [Google Scholar]
- Treatment of hypertrophic scars using laser-assisted corticosteroid versus laser-assisted 5-fluorouracil delivery. Dermatol Surg. 2019;45:423-30.
- [Google Scholar]
- Penetration enhancement of two topical 5-aminolaevulinic acid formulations for photodynamic therapy by erbium:YAG laser ablation of the stratum corneum: Continuous versus fractional ablation. Exp Dermatol. 2010;19:806-12.
- [Google Scholar]
- The effect of laser treatment on skin to enhance and control transdermal delivery of 5-fluorouracil. J Pharm Sci. 2002;91:1613-26.
- [Google Scholar]
- Fractional laser-assisted topical delivery leads to enhanced, accelerated and deeper cutaneous 5-fluorouracil uptake. Expert Opin Drug Deliv. 2017;14:307-17.
- [Google Scholar]
- Efficacy and safety of intralesional 5-fluorouracil in the treatment of keloids. Dermatology. 2002;204:130-2.
- [Google Scholar]
- The effect of carbon dioxide laser surgery on the recurrence of keloids. Plast Reconstr Surg. 1991;87:44-9; discussion 50-3.
- [Google Scholar]






