Translate this page into:
Efficacy of non-cultured non-trypsinized dermabraded epidermal cell graft followed by narrowband ultraviolet B phototherapy in stable vitiligo
*Corresponding author: Subhashini Konala, Department of Dermatology, Venereology, and Leprosy, GSL Medical College, Rajahmahendravaram, Andhra Pradesh, India. subha.konala@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chugh D, Kolalapudi SA, Praveen S, Konala S, Swetha NS, Reddy MK. Efficacy of non-cultured non-trypsinized dermabraded epidermal cell graft followed by narrowband ultraviolet B phototherapy in stable vitiligo. J Cutan Aesthet Surg. 2025;18:48-55. doi: 10.25259/JCAS_116_2024
Abstract
Objectives:
The objective of this study was to evaluate the efficacy and adverse effects of non-cultured, nontrypsinized dermabraded epidermal cell graft followed by narrowband ultraviolet B (NB-UVB) therapy for stable vitiligo.
Material and Methods:
A hospital-based and prospective interventional study was carried out on 45 patients (18–65 years) of both genders after approval from the Ethics Committee. The donor site was dermabraded after applying mupirocin ointment, and the material obtained was spread over the dermabraded recipient site. NBUVB phototherapy was initiated 3 weeks after the procedure and given for 3 months. Photographs were taken before the procedure and at the end of 3rd month of phototherapy and assessed for extent, pattern, and color matching of repigmented area according to physician global assessment (PGA) score and patient satisfaction score (PSS). Dermoscopic improvement was also noted.
Results:
Forty-five patients were enrolled in the study, out of which 43 patients completed the study. According to the intention to treat analysis, results were calculated in all 45 patients. Good to excellent response (50–100% improvement) was seen in 46.7% of patients according to the PGA score and in 57.8% of patients according to PSS. Most patients achieved the same color match with their normal skin at the end of the follow-up (73.3%). The most common repigmentation pattern was diffuse (46.7%), both clinically and dermoscopically. Among the clinical types, vitiligo vulgaris showed the maximum good to excellent repigmentation (61.3% and 77.4% of patients with PGA scores and PSS, respectively). Adverse effects were erythema, infection, and post-inflammatory hyper-pigmentation at the donor and recipient sites, whereas scarring was seen at the recipient site.
Conclusion:
It is a safe, simplified, cost-effective, and less time-consuming technique than earlier techniques and provides good to excellent repigmentation in a considerable proportion of participants.
Keywords
Dermabrasion
Non-cultured
Non-trypsinized
Vitiligo surgery
INTRODUCTION
Vitiligo causes cosmetic disability and results in great psychosocial stress.1 The prevalence of vitiligo in Asia is 0.1%.2 Overall, the prevalence in India is 2.5%.2
Many medical treatment methods are available for vitiligo, such as psoralen plus ultraviolet A (PUVA), narrowband ultraviolet B (NB-UVB) phototherapy, topical steroids, excimer laser, and topical immunomodulators, which may be used either alone or in combination.3 Many times, medical therapy alone is not satisfactory. The vitiliginous areas may remain stable without showing any repigmentation.4 When there was no further response with medical treatment and the lesions were stable for 1 year, surgical management is a better option.5
These surgical techniques are based on a common principle: To transplant autologous melanocytes from a normal pigmented donor site to a depigmented site.
Surgical techniques are broadly divided into tissue and cellular grafting6 and each technique has its limitations. Cellular grafting can treat large recipient areas with relatively smaller donor areas and consists of non-cultured and cultured cellular suspension. Cultured techniques are expensive and time-consuming. Non-cultured autologous melanocyte transfer is inexpensive but has certain limitations, such as expertise in taking skin grafts, incubation, and the need for additive agents (trypsin, ethylenediaminetetraacetic acid [EDTA], and media). A newer simplified technique with a non-cultured, non-trypsinized dermabraded epidermal cell graft followed by phototherapy has overcome the disadvantages of the above technique.7 In this technique, manual/motorized dermabrader was used to obtain epidermal cells from the donor area, and the paste-like material obtained (containing melanocytes, keratinocytes, and dermis) was collected with a spatula over a slide and was subsequently spread over the recipient area. This is a simplified, easier, and less time-consuming technique. There is no need for incubation and no need for additives (trypsin, EDTA).
NB-UVB alone is also an effective modality to treat vitiligo. However, the effect of the combination of non-cultured, nontrypsinized dermabraded epidermal cell graft and NB-UVB phototherapy has not been studied well. Hence, this study will add value to the existing literature.
MATERIAL AND METHODS
The study was done at a tertiary care teaching hospital from August 2022 to January 2024 after obtaining permission from the Institutional Ethics Committee (IEC/IRB Ref No: 827-EC/827-06/22).
It was a hospital-based prospective interventional study involving patients with stable vitiligo lesions who met the inclusion criteria. Participants included patients aged 18–65 years with stable vitiligo lesions for at least 1 year who consented to epidermal cell grafting and NB-UVB therapy. Exclusion criteria comprised infection over lesional sites, bleeding disorders, use of anticoagulants, unstable vitiligo, pregnancy and breastfeeding, and a history of skin cancer, keloids, hypertrophic scars, psoriasis, lichen planus, photosensitivity disorders, and Koebner’s phenomenon. Informed and written consent was taken from the patient. Detailed history, general physical, dermatological examination, and necessary laboratory investigations were documented.
Graft procedure
Equipments
Motorized dermabrader, spatula, sterile Petri dish, and topical 2% mupirocin ointment.
Recipient site
The Vitiligo site was prepared under sterile conditions. Hair over the site was shaved, cleaned with spirit, and anesthetized with 2% lidocaine after the test dose. Then dermabrasion was done over a vitiliginous patch using an electric dermabrader at the speed of 3500 rpm until pin-point bleeding was seen. This ensured that the dermabrasion was done at the level of the dermo-epidermal junction.
Donor site
The lateral area of the thigh was selected as a donor site in all the patients. The hair at the donor site was shaved off. The donor site was painted with povidone-iodine and then cleaned with spirit, and 2% lidocaine was infiltrated. This was followed by the application of mupirocin ointment to get a high yield of epidermal particles. Dermabrasion was done with the help of motorized dermabrader at 3000–5000 rpm and was continued until the area appeared whitish (i.e., upper dermis); then, the paste such as material containing melanocytes, keratinocytes, and dermis entangled in mupirocin ointment was collected and was subsequently spread over the recipient area with the help of the spatula.
Dressing was done with antibiotic-soaked gauze at both donor and recipient sites. After 10 days, dressings at both sites were removed. The patient was advised to apply topical mupirocin ointment daily, and oral antibiotics (amoxicillin and clavulanic acid 625 mg twice daily) were given for 1 week.
NB-UVB phototherapy
NB-UVB phototherapy (Derma India Company, Philip TL/01) was used. Patients were given NB-UVB phototherapy twice a week for 3 months post-surgery. The initial starting dose of NB-UVB was 200 mJ/cm2 with a 10% increment in every session. The patient’s eyes were protected by UV-protected goggles and genital areas were covered during phototherapy.
Digital and dermoscopic photographs were taken at the recruitment time, at the initiation of phototherapy, and at the end of 3 months of phototherapy with the patient’s consent. The degree of repigmentation was observed after 3 months of phototherapy and was graded according to physician global assessment (PGA) score and patient satisfaction score (PSS). Dermoscopic improvement was also noted.
Statistical analysis
Statistical analysis was done by the Statistical Package for the Social Sciences Software 20.0 Version and MS EXCEL 2010. All qualitative data were described in percentages. Descriptive data were presented as mean ± standard deviation and percentages. Data were tabulated and graphically represented. A chi-square test was done for categorical data evaluation. The result was considered significant when the P-value was <0.05.
RESULTS
A total of 45 patients attending our outpatient department were enrolled in the study. Forty-three patients completed the study. Two patients could not complete the study due to personal reasons. Considering the intention to treat analysis, results were assessed in all 45 patients.
The demographic details are given in Table 1. Out of 45 patients, the majority (22, 48.9%) were found in the 31–40 years age group. The mean age of the study population was 31.82 years, with the majority being female (26 patients, 57.8%). The face was the most commonly affected site (12 patients, 26.7%), while vitiligo vulgaris was the predominant type, affecting 31 patients (68.9%). The mean duration of the disease was 6.6 years, and the mean duration of stability was 3.6 years. A small portion reported a family history of vitiligo (6.7%), diabetes (11.1%), and hypothyroidism (6.7%).
| Category | Subcategory | Number of patients | Percentage | Mean value |
|---|---|---|---|---|
| Mean age | 31.82 years | |||
| Gender | Female | 26 | 57.8 | - |
| Male | 19 | 42.2 | - | |
| Site of vitiligo | Face | 12 | 26.7 | - |
| Lip | 2 | 4.4 | - | |
| Upper limb | 8 | 17.8 | - | |
| Lower limb | 11 | 24.4 | - | |
| Trunk | 7 | 15.6 | - | |
| Acral | 5 | 11.1 | - | |
| Type of vitiligo | Vitiligo vulgaris | 31 | 68.9 | - |
| Focal | 7 | 15.6 | - | |
| Mucosal (lip) | 2 | 4.4 | - | |
| Acral | 5 | 11.1 | - | |
| Mean duration of disease | 6.6 years | |||
| Mean duration of stability | 3.6 years | |||
| Family history | 6.7 | - | ||
| Comorbidities | Diabetes | 5 | 11.1 | - |
| Hypothyroidism | 3 | 6.7 |
Good to excellent response was seen in 21 patients (46.7%) according to the PGA score and in 26 patients (57.8%) according to PSS [Table 2 and Figures 1-3]. Among the clinical types, vitiligo vulgaris showed the maximum good to excellent repigmentation (61.3% and 77.4% of patients with PGA scores and PSS, respectively). Among the clinical sites, the upper limb showed the maximum good to excellent repigmentation (62.5% and 87.5% of patients with PGA scores and PSS, respectively).
| Score | PGA at 3 months | PSS at 3 months | ||
|---|---|---|---|---|
| No. of patients | Percentage | No. of patients | Percentage | |
| 0 No improvement | 5 | 11.1 | 5 | 11.1 |
| 1 Minimal (1–25%) | 8 | 17.8 | 7 | 15.6 |
| 2 Moderate (26–50%) | 11 | 24.4 | 7 | 15.6 |
| 3 Good (51–75%) | 12 | 26.7 | 14 | 31.1 |
| 4 Excellent (76–100%) | 9 | 20.0 | 12 | 26.7 |
PGA: Physician global assessment, PSS: Patient satisfaction score
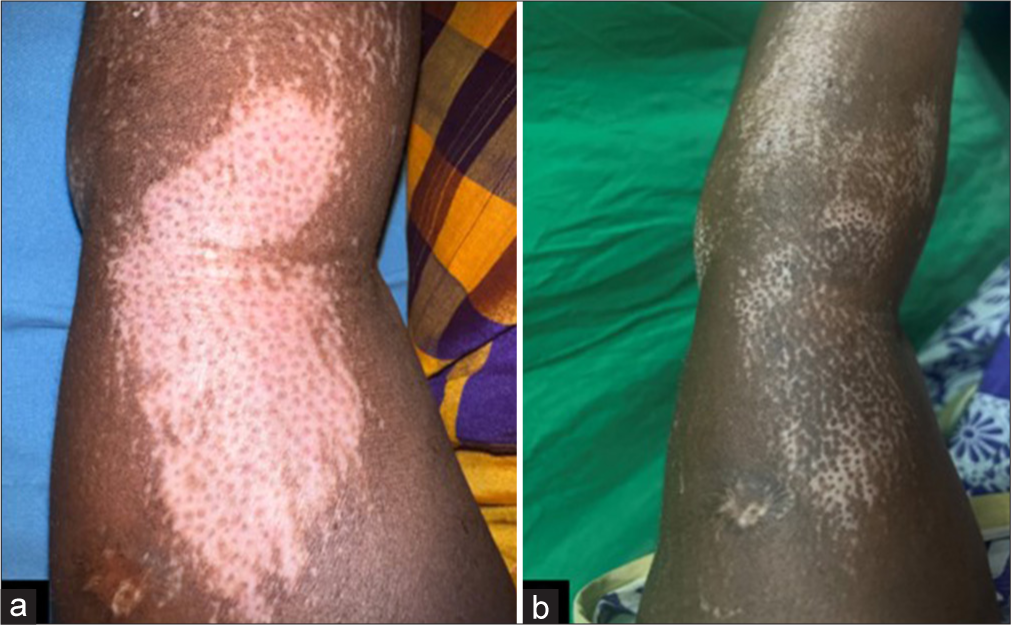
- (a) Pre-procedure and (b) post procedure image after 3 months of follow-up with grade 4 (>75% repigmentation) improvement, diffuse pattern of repigmentation, and same color match.
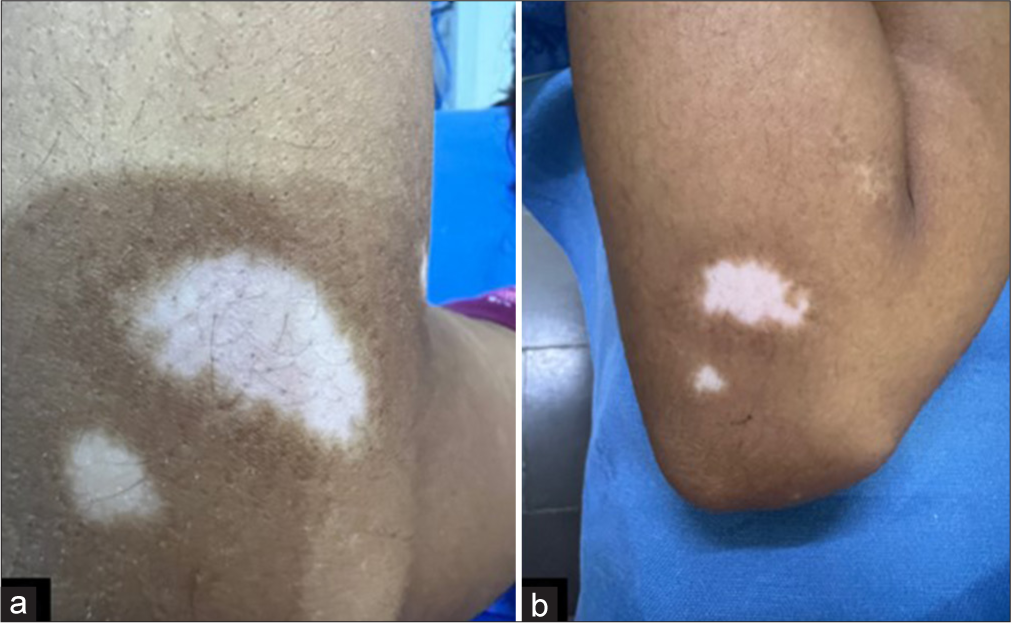
- (a) Pre-procedure and (b) post-procedure image after 3 months of follow-up with grade 2 (25–50% repigmentation) improvement, marginal pattern of repigmentation, and same color match.
- (a) Pre-procedure and (b) post-procedure image after 3 months of follow-up with grade 2 (25–50% repigmentation) improvement, dotted pattern of repigmentation, and same color match.
The results for the color match were promising, with 33 patients (73.3%) achieving pigmentation closely resembling their normal skin tone [Figures 1-3]. However, 5 patients (11.1%) experienced darker pigmentation and another 5 patients (11.1%) showed no pigmentation [Figure 4]. The same color match was achieved in almost all types and sites except acral.
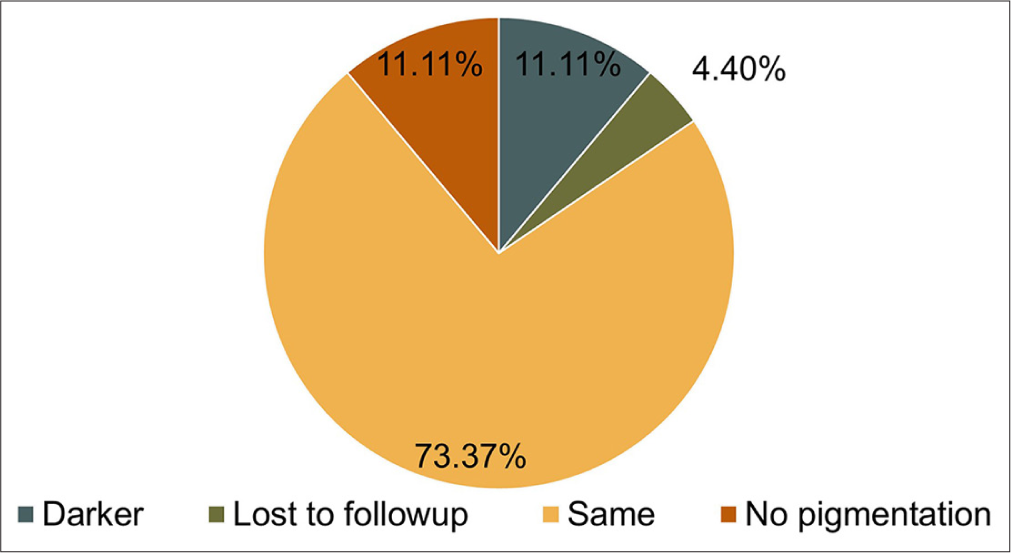
- Color match with normal skin post-surgery.
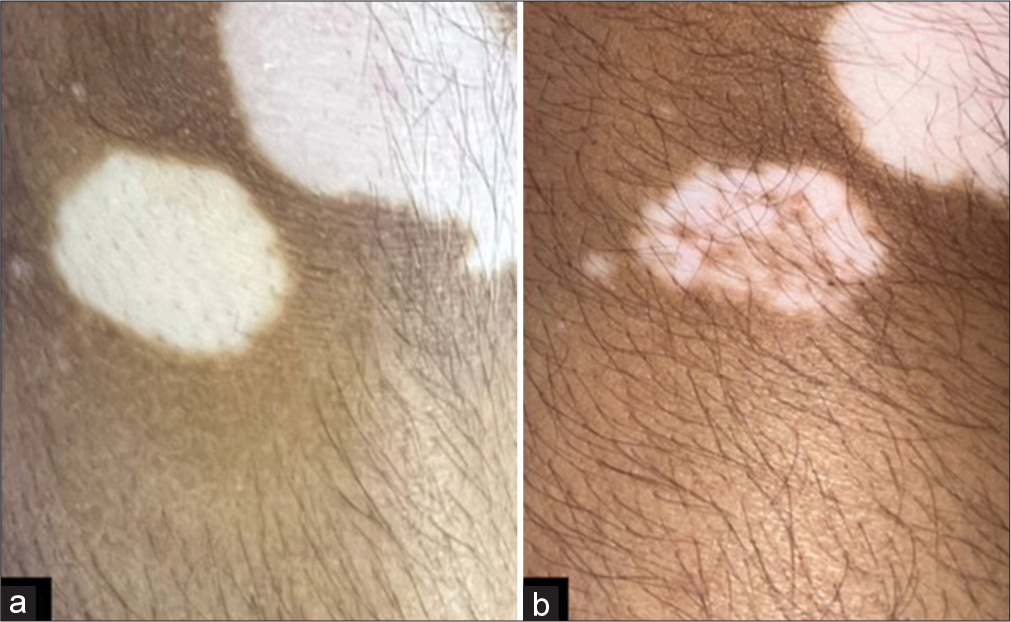
The most common pattern of repigmentation observed by naked eye examination was diffuse (21, 46.7%) [Figure 1b], followed by marginal repigmentation (12, 26.7%) [Figure 2b] and dotted (5, 11.1%) [Figure 3b]. On dermoscopy, diffuse pigmentation was seen in most (23, 51.1%), followed by marginal repigmentation (12, 26.7%) and perifollicular (5, 11.1%) [Figures 5 and 6]. For the dotted pattern, the mean number of dots seen clinically by the naked eye was 20.2, and by dermoscopy was 28.2 [Figure 7].
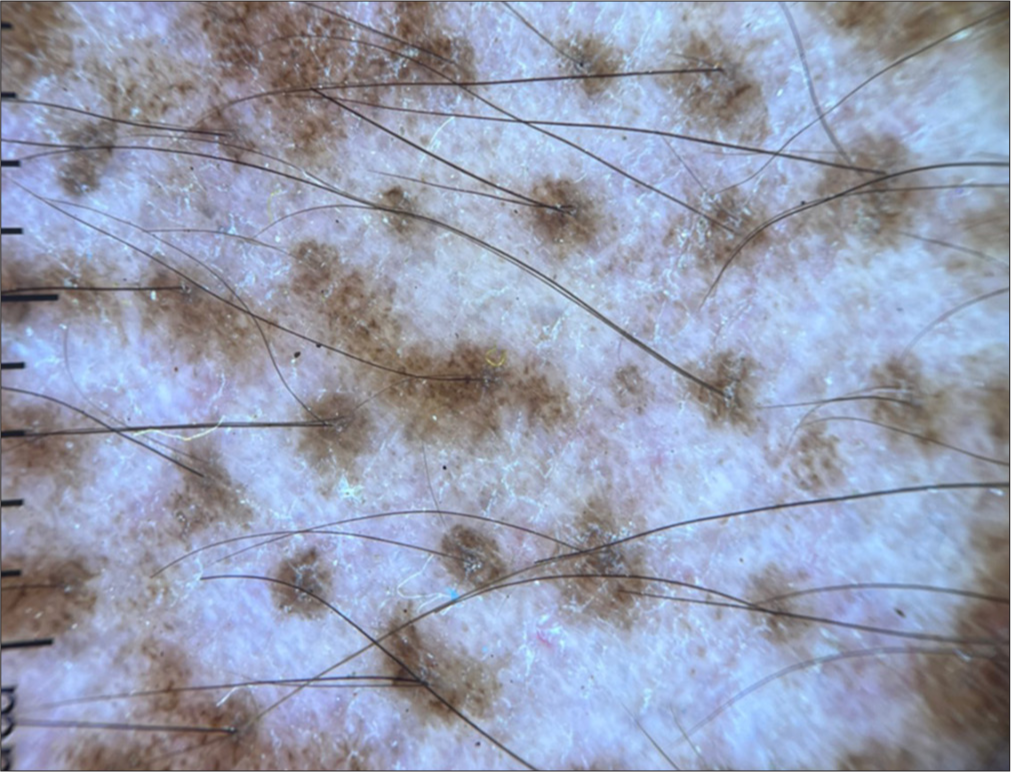
- Perifollicular repigmentation seen on dermoscopy (DermLite DL4, non-polarized, ×10 magnification).
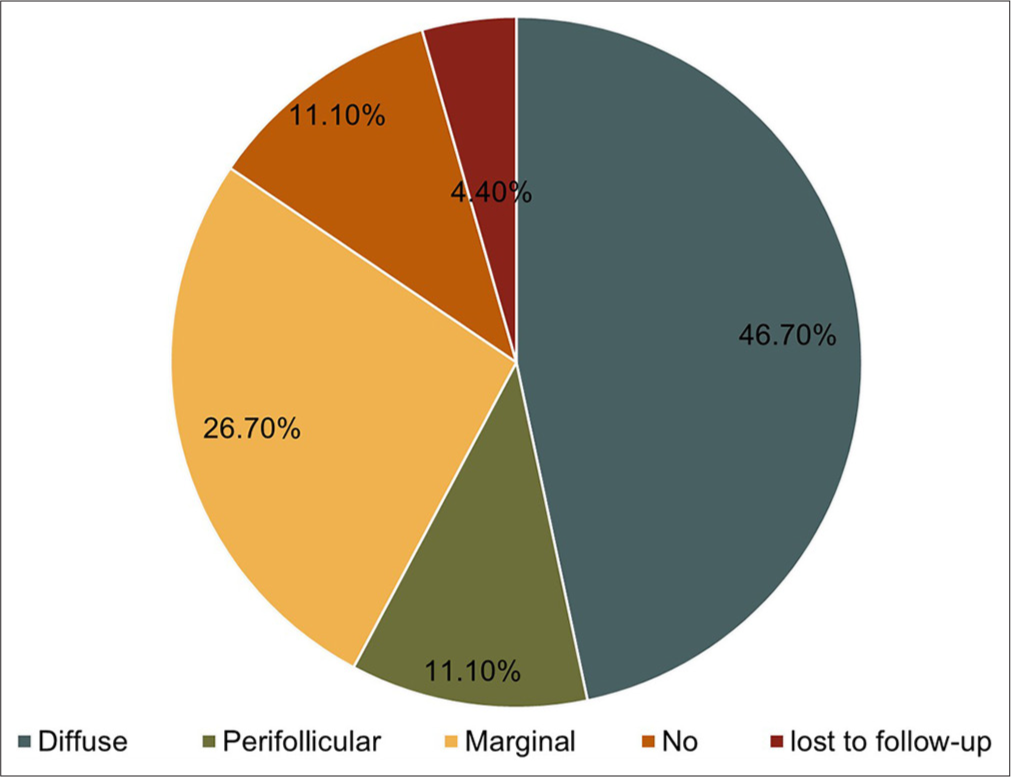
- Pattern of repigmentation when seen dermoscopically post-surgery.
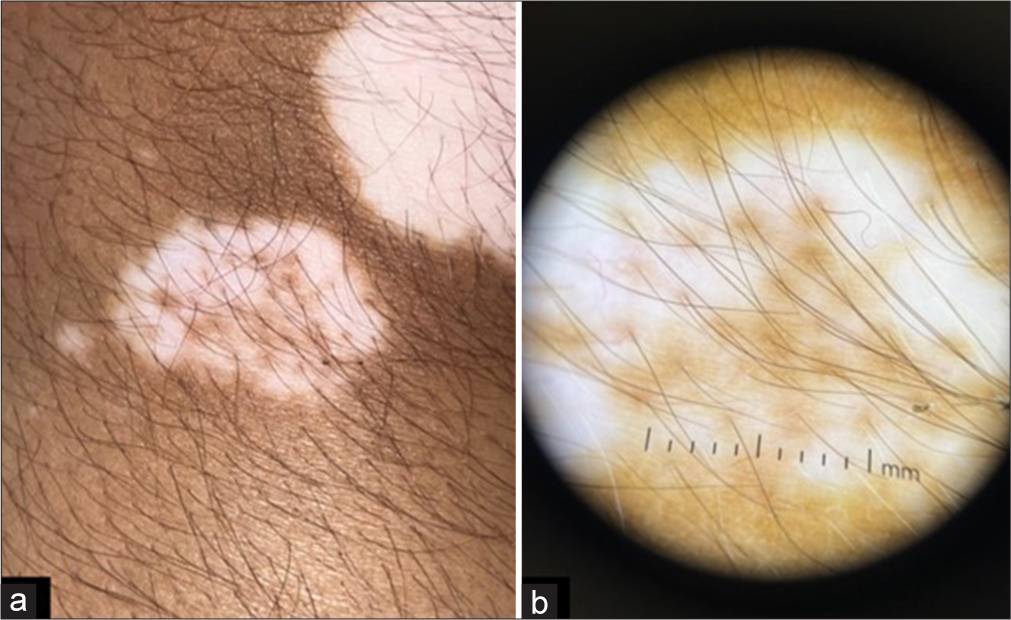
- (a and b) Increased number of dots seen on dermoscopy when compared to naked eye examination (a) 16 dots on naked eye examination and (b) 22 dots seen on dermoscopic examination (DermLite DL4, non-polarized, ×10 magnification).
At the donor site, erythema was noted in 2 patients (4.4%), infection in 3 patients (6.7%), and post-inflammatory hyperpigmentation (PIH) in 4 patients (8.9%), with no instances of scarring or milia reported. At the recipient site, erythema occurred in 4 patients (8.9%), infection [Figure 8] and PIH each were present in 2 patients (4.4%), scarring was also seen in 2 patients (4.4%), and no milia were observed. The complications arising from phototherapy include erythema in 8 patients (17.8%), desquamation in 2 patients (4.4%), and herpes labialis in 2 patients (4.4%).
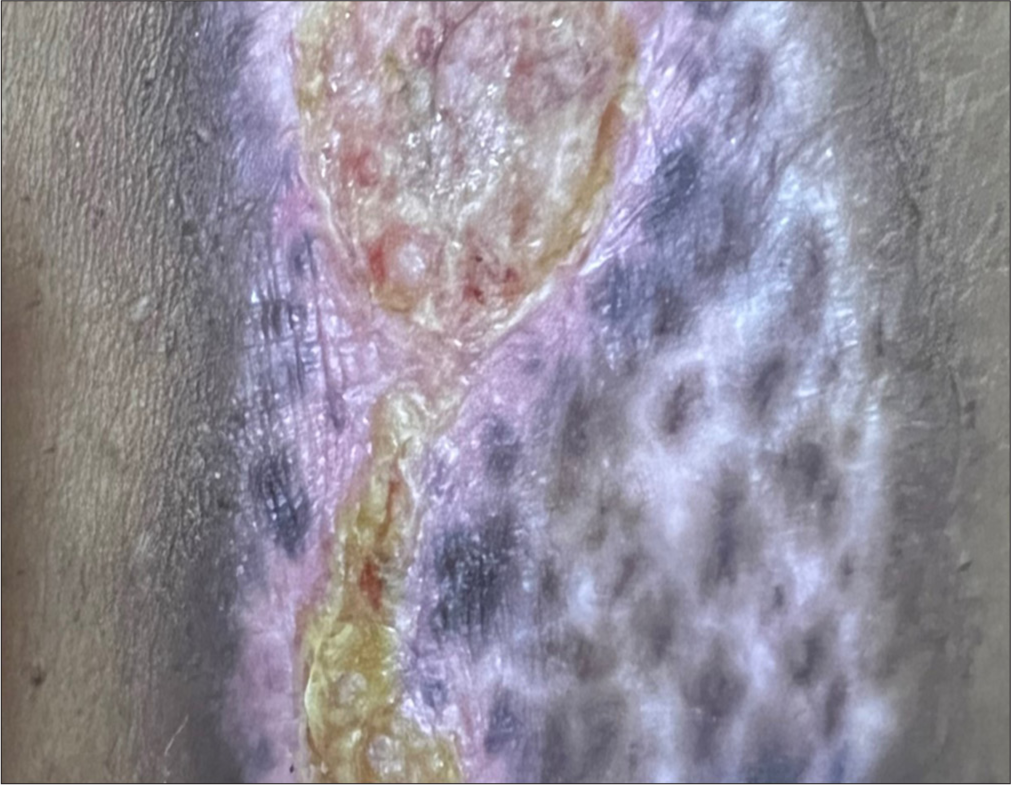
- Infection with crusting at recipient site.
DISCUSSION
This study introduces a novel approach by combining non-cultured, non-trypsinized dermabraded epidermal cell grafting with NB-UVB phototherapy in the treatment of stable vitiligo. This is a simplified, easier, and less time-consuming technique and there is no need for incubation and no need for additives (trypsin, EDTA). This method leverages the advantages of surgical melanocyte transplantation to repopulate the depigmented areas with pigment-producing cells and the photobiological effects of NB-UVB light to stimulate melanogenesis. The efficacy and safety of this combined treatment were evaluated in a hospital-based prospective interventional study, highlighting a significant improvement in repigmentation and patient satisfaction.
A comparison of techniques used for grafting among various studies is mentioned in Table 3.8-14 According to PGA, both our study and Kachhawa et al.’s7 study demonstrated good-excellent outcomes (>50% response) in 46.7% and 67% of the patients, respectively, with non-cultured non-trypsinized epidermal cell grafting, whereas other studies such as Gill et al.,8 Verma et al.,9 Pandya et al.,10 Mulekar,11 Van Geel et al.,4 and Kahn and Cohen12 which used the trypsinized methods exhibited slightly superior results with good-excellent response in 60–100% of the cases compared to the non-trypsinized technique [Table 4]. This suggests that trypsinization may enhance the effectiveness of the epidermal cell grafting procedure. However, our method was easier, simplified, and time-saving without any need for incubation and additives (trypsin, EDTA) along with appreciable results.
| Study | Technique used | Donor site preparation | Recipient site preparation | Use of additives |
|---|---|---|---|---|
| Our study | Non-cultured non-trypsinized melanocyte transfer | Dermabrasion | Dermabrasion | Not used |
| Gill et al.8 (2019, Punjab, India) | Non-cultured melanocyte transplant | Split skin thickness | Dermabrasion | Trypsin, EDTA, Hi media 3001 |
| Gupta et al.3 (2019, Delhi, India) | Non-cultured melanocyte keratinocyte transplant | Split skin thickness | Er-YAG laser, dermabrasion | Trypsin, Hi media, trypsin inhibitor, phosphate-buffered saline. |
| Kachhawa et al.7(2017, Jodhpur, India) | Non-cultured non-trypsinized Epidermal cell grafting | Dermabrasion | Dermabrasion | Not used |
| Verma et al.9 (2014, India) | AMRCS (non-cultured) and cultured comparison | Split skin thickness | Dermabrasion | Trypsin, EDTA, DMEM media |
| Pandya et al.10 (2005, Ahmedabad, India) | Non-cultured and cultured melanocyte transfer | Split skin thickness | Dermabrasion | Trypsin, MK media, trypsin inhibitor, |
| Mulekar11 (2003, Pune, India) | Non-cultured epidermal cell transplant | Shave biopsy | Dermabrasion | Trypsin, DMEM media, trypsin inhibitor |
| Van Geel et al.4(2001, Ghent, Belgium) | Non-cultured melanocyte keratinocyte transplant | Shave graft | CO2 Laser | Trypsin, EDTA, M199 media, phosphate buffer saline+hyaluronic acid |
| Kahn and Cohen12 (1998, Los Angeles, California, USA) | AMRCS | Split skin thickness | dermabrasion and CO2 Laser | |
| Olsson and Juhlin13 (1998, Stockholm, Sweden) | Non-cultured melanocyte keratinocyte transplant | Shave biopsy | Dermabrasion | Phosphate buffer saline |
| Gauthier and Surleve-Bazeille14 (1992, France) | Non-cultured epidermal cellular grafting | Shave biopsy from scalp | Blister by liquid nitrogen | Trypsin, EDTA, trypsin inhibitor, |
EDTA: Ethylenediaminetetraacetic acid, CO2: Carbon dioxide, Er:YAG: Erbium-doped yttrium aluminum garnet, AMRCS: Autologous melanocyte-rich cell suspension, DMEM: Dulbecco’s modified eagle medium, MK: Melanocyte keratinocyte
| Study | Results |
|---|---|
| Our study | Good to excellent response (>50% repigmentation)- 46.7% patients |
| Gill et al.8 (2019, Punjab, India) | Good repigmentation (>70%): 62% patients |
| Kachhawa et al. 7(2017, Jodhpur, India) | Excellent (>75%): in 41% of patches |
| Verma et al.9 (2014, India) | Excellent (>70%): 62.17% patients for non-cultured and 52% for cultured melanocyte transplant |
| Pandya et al.10 (2005, Ahmedabad, India) | Excellent response (>90%)- 52.17% cases |
| Mulekar11 (2003, Pune, India) | Excellent (95–100%) repigmentation in 65 (53%), good (65–94%) repigmentation in 10 (8%) |
| Van Geel et al.4(2001, Ghent, Belgium) | >85% pigmentation - % cases |
| Kahn and Cohen12 (1998, Los Angeles, California, USA) | Excellent repigmentation: 88% patients |
In comparing our study with Kachhawa et al.,7 our study involved a smaller sample size (45 patches vs. 437 patches). While Kachhawa et al.7 reported a higher excellent response rate (>75% repigmentation) in 41% of patients compared to our study (20% of patients) and a higher proportion of good to excellent responses (>50% repigmentation) in 67% compared to 46.6% in our study. Differences in expertise, precision, and surgeon’s approach could be the reason for the difference in results between our study and Kachhawa et al.’s7 study. Both studies identified similar good response sites, while acral areas consistently showed poor response in both. Our study evaluated the degree of repigmentation dermoscopically which was not done in Kachhawa et al.’s7 study. Adverse effects differed between the studies, with our study reporting erythema, infection, PIH, and scarring, whereas Kachhawa et al.7 did not observe hyperpigmentation and scarring. In addition, color matching was higher in Kachhawa et al.’s7 study (94.8%) compared to ours (73.3%). Post-surgical phototherapy modality used in Kachhawa et al’s7 study was psoralen plus ultraviolet A using sunlight (PUVASOL), whereas our study utilized NB-UVB phototherapy.
Our study performed a dermoscopy to assess the pattern of repigmentation. For the dotted pattern, the mean number of dots seen clinically by the naked eye was 20.2 and by dermoscopy was 28.2, which suggests that dermoscopy enhances the detection sensitivity for identifying dotted patterns. This highlights the importance of using dermoscopy as a complementary tool to detect subtle skin changes not visible to the naked eye. The dermoscopic assessment was not done in any previous studies.
In our study, few side effects were noted; common side effects included erythema, infection, PIH, and scarring, almost aligning with other studies.4,8-10 However, Gupta et al.,3 Pandya et al.,10 and Mulekar11 reported new lesions exclusively at the donor site, suggesting a different pattern of side effects. This could be probably due to a lack of reasonable generalized stability or due to local instability. None of the patches in our study showed new lesions either at the donor or recipient sites. Erythema and infection resolved after a course of antibiotics. To reduce PIH, Gupta et al.3 suggested that any form of post-operative phototherapy should be stopped when sufficient color matching is achieved.
In discussing the utilization of phototherapy post-surgery in vitiligo treatment, Kachhawa et al.,7 Verma et al.,9 and Van Geel et al.4 utilized PUVA therapy. In contrast, our study opted for NB-UVB phototherapy post-surgery due to several advantages associated with NB-UVB phototherapy. NB-UVB has been increasingly favored due to its higher safety profile compared to PUVA with reduced risk of systemic side effects, such as nausea and hepatotoxicity, commonly associated with psoralen use in PUVA therapy.15
In addition, NB-UVB phototherapy is well-suited for use in combination with surgical interventions16 due to its compatibility with wound healing processes and its ability to promote melanocyte proliferation and migration. This synergistic effect can potentially enhance the outcomes of surgical procedures by stimulating repigmentation and minimizing the risk of depigmentation recurrence.
Limitations
The small sample size and the absence of a control group receiving either treatment alone or the absence of a long-term follow-up to assess the durability of repigmentation were our limitations.
CONCLUSION
Non-cultured non-trypsinized epidermal cell grafting, followed by NBUVB phototherapy, showed good to excellent repigmentation in a considerable proportion of participants, corroborating the potential of this combined treatment modality to improve the clinical outcomes for individuals with stable vitiligo significantly. Moreover, the treatment was well-tolerated, with minimal and reversible side effects, indicating its feasibility and safety for broader clinical application.
The main advantage of this technique is that it is simple and inexpensive. By forgoing trypsin and other additives, this method simplified the grafting process, rendering it faster and easier to execute compared to trypsinized melanocyte transfer methods. Although the excellent response was slightly less than the non-cultured melanocyte transfer (NCMT), it can be an optional treatment in less resourceful places.
Authors’ contributions
All the authors have made substantial contributions in intellectual content, conceptualizing and designing of the work, the analysis and interpretation of the data (when applicable), as well as the writing of the manuscript.
Ethical approval
The research/study approved by the Institutional Review Board at GSL Medical College and General Hospital, number IEC/IRB Ref No: 827-EC/827-06/22, dated June 23, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Quality of life in patients with vitiligo. Health Qual Life Outcomes. 2003;23(1):58.
- [CrossRef] [PubMed] [Google Scholar]
- A nationwide, multicentric case-control study on vitiligo (MEDEC-V) to elicit the magnitude and correlates. Indian J Dermatol. 2020;65:473-82.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous noncultured melanocyte-keratinocyte transplantation in stable vitiligo: A randomized comparative study of recipient site preparation by two techniques. Indian J Dermatol Venereol Leprol. 2019;85:32-8.
- [CrossRef] [PubMed] [Google Scholar]
- Modified technique of autologous noncultured epidermal cell transplantation for repigmenting vitiligo: A pilot study. Dermatol Surg. 2001;27:873-6.
- [CrossRef] [PubMed] [Google Scholar]
- Stability in vitiligo? What's that? J Cutan Aesthet Surg. 2009;2:38-40.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of vitiligo. Int J Environ Res Public Health. 2022;19:4812.
- [CrossRef] [PubMed] [Google Scholar]
- Simplified non-cultured nontrypsinised epidermal cell graft technique followed by psoralen and ultraviolet a light therapy for stable vitiligo. J Cutan Aesthet Surg. 2017;10:81-5.
- [CrossRef] [PubMed] [Google Scholar]
- Non-cultured melanocyte transfer in the management of stable vitiligo. J Family Med Prim Care. 2019;8:2912-6.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative study of efficacy of cultured versus non cultured melanocyte transfer in the management of stable vitiligo. Med J Armed Forces India. 2014;70:26-31.
- [CrossRef] [PubMed] [Google Scholar]
- A study of autologous melanocyte transfer in treatment of stable vitiligo. Indian J Dermatol Venereol Leprol. 2005;71:393-7.
- [CrossRef] [PubMed] [Google Scholar]
- Melanocyte-keratinocyte cell transplantation for stable vitiligo. Int J Dermatol. 2003;42:132-6.
- [CrossRef] [PubMed] [Google Scholar]
- Repigmentation in vitiligo patients. Melanocyte transfer via ultra-thin grafts. Dermatol Surg. 1998;24:365-7.
- [CrossRef] [Google Scholar]
- Leucoderma treated by transplantation of a basal cell layer enriched suspension. Br J Dermatol. 1998;138:644-8.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous grafting with noncultured melanocytes: A simplified method for treatment of depigmented lesions. J Am Acad Dermatol. 1992;26:191-4.
- [CrossRef] [PubMed] [Google Scholar]
- Psoralen-ultraviolet A vs. narrow-band ultraviolet B phototherapy for the treatment of vitiligo. J Eur Acad Dermatol Venereol. 2006;20:175-7.
- [CrossRef] [PubMed] [Google Scholar]
- Validation of a physician global assessment tool for vitiligo extent: Results of an international vitiligo expert meeting. Pigment Cell Melanoma Res. 2019;32:728-33.
- [CrossRef] [PubMed] [Google Scholar]






