Translate this page into:
Efficacy of platelet-rich plasma in alleviating split skin graft morbidities
Address for correspondence: Prof. Seema Khanna, Department of General Surgery, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221005, Uttar Pradesh, India. E-mail: seemakhanna119@rediffmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Introduction:
Skin grafting is a routinely employed technique to cover the skin defect. Though the skin grafts are technically effortless, they are tiresome because of the prolonged duration of hospital stay, labor–intensive, demanding repeated dressings, and also create a second wound. Platelet-rich plasma (PRP) is one that has a higher concentration of platelets than the blood. Alpha granules of the platelets are rich in growth factors.
Aims and Objectives:
To assess the effect of PRP on split-thickness skin graft uptake and donor site healing.
Materials and Methods:
In a single-center-based prospective study done from August 2018 to June 2020, 60 patients with acute and chronic wounds were divided into two equal groups. Autologous PRP was applied on the recipient wound bed and donor site in PRP group, and conventional methods like staples/sutures were used to anchor the skin grafts and standard of care of the donor site in a control group.
Results:
Instantaneous graft adhesion was observed in all patients of PRP group. The first graft inspection was delayed. Seroma, hematoma, total number of dressings, and duration of stay in hospital were significantly reduced in the PRP group. Donor site pain in the postoperative period was notably reduced in PRP group. PRP also remarkably hastened the donor site healing.
Conclusion:
The application of PRP promotes graft take, minimizes complications, enhances donor site wound healing, mitigates donor site pain, and has immense economic benefits due to the reduced number of dressing changes and shorter hospital stay.
Keywords
Adhesion
donor site
pain
PRP
split skin graft
uptake
INTRODUCTION
Skin grafting is a routinely employed technique to cover skin defects, ignoring the cause of the defect. Though skin grafts are technically effortless, they often require a prolonged duration of hospital stay and are labor intensive, demanding repeated dressings. It also creates a second wound that can cause excruciating pain and other morbidities.
Platelets play a key role in hemostasis. Normal platelet counts in the blood range from 1,50,000 to 350,000/µL. Platelet-rich plasma (PRP) contains a 3–5-fold increase in growth factor concentrations. PRP is believed to promote healing.[1]
Aims and Objectives
To assess the effect of PRP on split-thickness skin graft (STSG) uptake and donor site morbidities.
MATERIALS AND METHODS
In a single-center-based prospective interventional study done from August 2018 to June 2020, 60 patients with acute and chronic wounds were included and were assigned to either PRP group or control group alternately. Patients who are immunocompromised or have coagulation disorders were excluded from the study. Ethical clearance was obtained from the institute's ethics committee. Informed written consent was obtained from all patients. The wound area was measured preoperatively by measuring the two largest perpendicular diameters using a ruler (in centimeters) and multiplying these two diameters.
Autologous PRP was prepared in the operation theatre at the start of surgery. After induction of general anesthesia, blood (10 mL of whole blood/100 sq cm of area) was collected under strict aseptic conditions in citrate vials, and PRP was prepared by the double spin technique. Blood was centrifuged at 2400 rpm for 10 min. Supernatant plasma containing platelets was transferred into another sterile tube without anticoagulant. A tube containing plasma was centrifuged at a higher speed, i.e., at 3600 rpm, for 15 min to obtain platelet concentrate. Platelet pellets are seen to form at the bottom of the tube. The lower one-third is PRP, and the upper two-thirds is platelet-poor plasma (PPP). PPP was discarded, and platelet pellets were suspended in approximately 2–4 mL of plasma by gently shaking the tube.
Topical application of PRP on the wound was made, and a graft was placed. Topical application on the donor site was made, i.e., PRP was sprayed over the donor site, followed by regular dressing. Instant anchorage of the graft (2–3 min) was confirmed by gently trying to move the graft. If the instant anchorage is not appreciated, then we proceed with Mechanical fixation, either with staples or sutures. In control group, fixation techniques like sutures or staplers were used.
The first graft inspection was done after post-operative day (POD)#5 in PRP group and on POD#3 in control group. Seroma, hematoma, or any graft infection or rejection are noted in both groups. The total number of dressings and duration of hospital stay of every patient was recorded. Pain at donor site was assessed with a visual analog scale (VAS) on POD 1, 3, and 5 and was categorized into mild if VAS is ≤3, moderate if VAS is 4–6, and severe if VAS is ≥7. First donor site inspection on POD# 14 in case group and on POD#21 or when dressing slides down, whichever is earlier in control group, and look for the percentage of the wound area that has healed and is classified into <50% or >50%. Patients were followed up for 3 months to assess both recipient and donor sites.
Statistical analysis was done using Statistical package for social sciences, (Developed by IBM Corp., New York) software for Windows (Version V27). The chi-square test was used for categorical variables. Students t-test was used for comparing means of two groups. P value <0.05 was considered significant.
RESULTS
Age, gender, comorbidities, nutritional status, wound characteristics like etiology, site, area of the wound were compared in both the groups [Table 1].
| Characteristic | Control | PRP | ||
|---|---|---|---|---|
| n (%) | n (%) | |||
| Age group (in years) | ||||
| <40 | 15 (50) | 17 (56.7) | ||
| >40 | 15 (50) | 13 (43.3) | ||
| Total | 30 (100) | 30 (100) | ||
| (P: 0.987) | ||||
| Gender | ||||
| Male | 18 (60) | 21 (70) | ||
| Female | 12 (40) | 9 (30) | ||
| Total | 30 (100) | 30 (100) | ||
| (P: 0.417) | ||||
| Comorbidity | ||||
| Absent | 20 (66.7) | 25 (83.3) | ||
| Present | 10 (33.3) | 05 (16.7) | ||
| Total | 30 (100) | 30 (100) | ||
| (P: 0.136) | ||||
| Site | ||||
| Trunk | 6 (20) | 4 (13.3) | ||
| Extremities | 24 (80) | 26 (86.7) | ||
| Total | 30 (100) | 30 (100) | ||
| (P: 0.488) | ||||
| Etiology | ||||
| Trauma and burns | 16 (53.3) | 11 (45) | ||
| Malignancy | 05 (16.7) | 06 (18.3) | ||
| Benign | 09 (30.0) | 13 (36.7) | ||
| Total | 30 (100) | 30 (100) | ||
| (P: 0.418) | ||||
| Area of the wound (cm2) | ||||
| Mean area | 63.73 | 73.53 | ||
| SD | 51.1 | 41.2 | ||
| (P: 0.41) | ||||
| Mean | SD | Mean | SD | |
| Hemoglobin (g%) | ||||
| 12.16 | 1.16 | 12.24 | 1.48 | |
| (P: 0.81) | ||||
| S. Transferrin (mg/dL) | ||||
| 249.07 | 11.44 | 251.97 | 21.81 | |
| (P: 0.52) | ||||
Instantaneous graft adherence was seen in all patients in PRP group and was not appreciated in any of control group patients.
The incidence of seroma was 36.7% in control group, whereas in PRP group, it was found to be 10 % (P = 0.015). The incidence of hematoma was 26.7% in control group, whereas in the PRP group, it amounted to 3.3% (P = 0.026). Our study demonstrated a 23.3% incidence of wound infection in the control group, whereas it was 3.3.% in PRP group [Table 2].
| Complications at recipient site | Control | PRP |
|---|---|---|
| n (%) | n (%) | |
| Seroma | ||
| Present | 11 (36.7) | 03 (10) |
| Absent | 19 (63.3) | 27 (90) |
| Total | 30 (100) | 30 (100) |
| (P: 0.015) | ||
| Hematoma | ||
| Present | 08 (26.7) | 01 (3.3) |
| Absent | 22 (73.3) | 29 (96.7) |
| Total | 30 (100) | 30 (100) |
| (P: 0.026) | ||
| Wound infection | ||
| Present | 07 (23.3) | 01 (3.3) |
| Absent | 23 (76.7) | 29 (96.7) |
| Total | 30 (100) | 30 (100) |
| (P: 0.052) | ||
| First graft inspection (P < 0.001) | ||
| Before POD#5 | 26 (86.7) | 02 (6.7) |
| After POD#5 | 04 (13.3) | 28 (93.3) |
| Total | 30 (100) | 30 (100) |
| (P:<0.001) | ||
| Duration of hospital stay | ||
| Less than 10 days | 11 (36.7) | 27 (90) |
| More than 10 days | 19 (63.3) | 03 (10) |
| Total | 30 (100) | 30 (100) |
| (P:<0.001) | ||
| Recipient site dressings | ||
| Less than 2 | 04 (13.3) | 26 (86.7) |
| More than 2 | 26 (86.7) | 04 (13.3) |
| Total | 30 (100) | 30 (100) |
| (P:<0.001) | ||
| Extent of healing of donor site | ||
| <50% | 14 (46.7) | 04 (13.3) |
| >50% | 16 (53.3) | 26 (86.7) |
| Total | 30 (100) | 30 (100) |
| (P: 0.004) | ||
| Scar hypertrophy of donor site | ||
| No | 27 (90) | 28 (93.3) |
| Yes | 03 (10) | 02 (6.7) |
| Total | 30 (100) | 30 (100) |
| (P: 0.64) | ||
First graft inspection was done before POD 5 in 86.7% patients in control group and in 6.7% patients in the PRP group. In the rest of the patients, i.e., in 13.3% patients in control group and in 93.3% patients of the PRP group, it was done after POD#5. The early graft inspection in control group was mainly either due to soakage of dressing or seroma formation. Duration of hospital stay was 10 days in 63.3% patients of control group, whereas it is so in 10% of the patients in the PRP group. A total number of recipient site dressing during hospital stay were less than two in just 13.3% of patients of control group and in 86.7% patients of PRP group. A number of dressings were more than two in the rest of the patients [Table 2, Figures 1 and 2].

- Recipient site graft take after PRP application
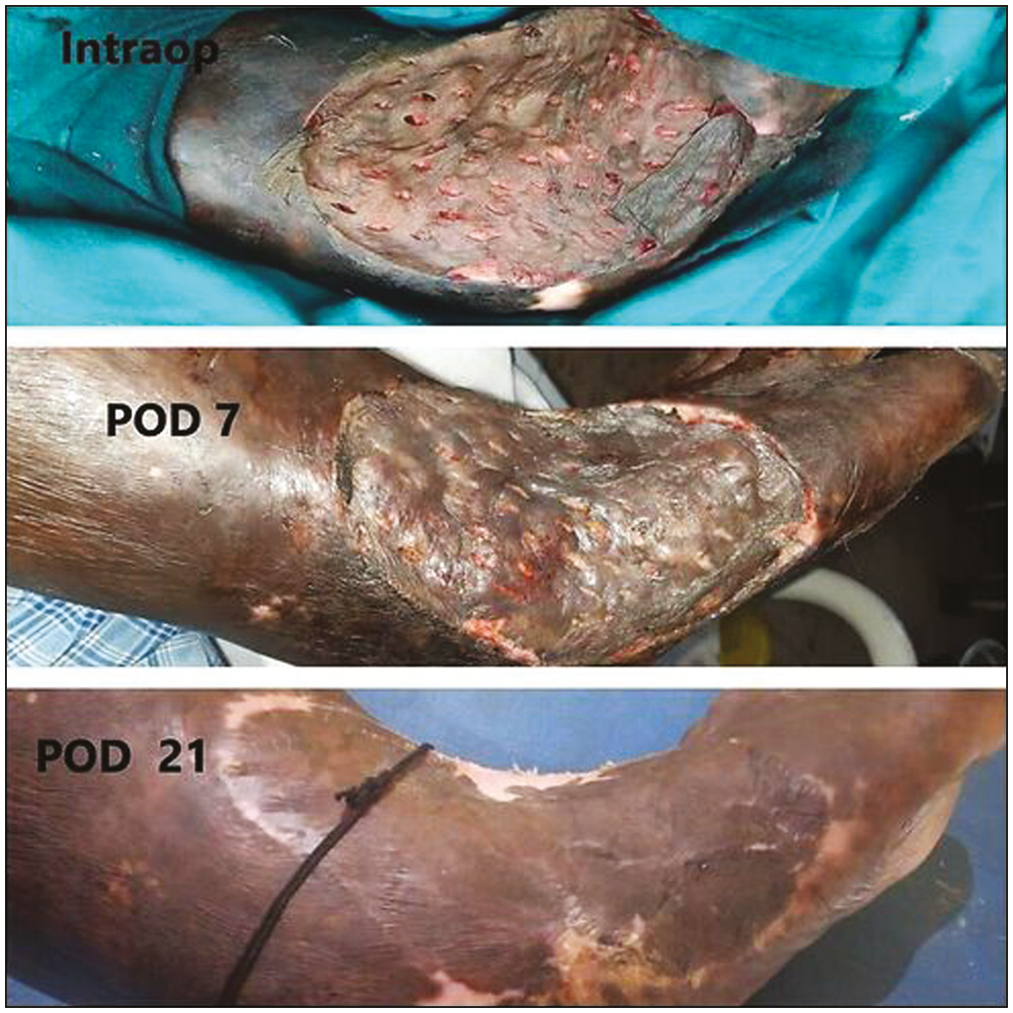
- Recipient site graft take after PRP application at POD 21
The severity of pain at donor site was assessed by VAS score and was categorized into mild, moderate, and severe. Patients in both groups were started on injectable Diclofenac IM 12 hourly and were transferred to oral analgesics by POD5 or upgraded to injectable opioid analgesics accordingly. In our study, four patients in control group were upgraded to opioid analgesics between POD1 and 4. On POD1 in control group, 93.3% experienced severe pain, while 6.7% had moderate pain. In PRP group, 70% patients complained of severe pain, while 30% patients experienced moderate pain. On POD3 in control group 60% patients experienced severe pain, whereas the remaining 40% had moderate pain. In PRP group, 3.3% had severe pain rest of the 96.7% had moderate pain. On POD5 in control group, 93.3% patients experienced moderate pain, and the rest of 6.7% patients complained of mild pain. Whereas in PRP group majority of the patients, i.e., 80% of them experienced mild pain, and only 20% complained of moderate pain on POD5 [Table 3].
| Pain at donor site | Control | PRP |
|---|---|---|
| n (%) | n (%) | |
| POD#1 | ||
| Severe (VAS ≥ 7) | 28 (93.3) | 21 (70) |
| Moderate (VAS 4–6) | 02 (06.7) | 09 (30) |
| Total | 30 (100) | 30 (100) |
| (P = 0.02) | ||
| POD#3 | ||
| Severe (VAS ≥ 7) | 18 (60) | 01 (03.3) |
| Moderate (VAS 4–6) | 12 (40) | 29 (96.7) |
| Total | 30 (100) | 30 (100) |
| (P < 0.001) | ||
| POD#5 | ||
| Moderate (VAS 4–6) | 28 (93.3) | 06 (20) |
| Mild (VAS ≤ 3) | 02 (06.7) | 24 (80) |
| Total | 30 (100) | 30 (100) |
| (P < 0.001) | ||
Donor site dressing was examined on POD14 in PRP group and in control group, it was examined on POD21 or when dressing slides down spontaneously, whichever is earlier. In control group extent of donor site healing on the first dressing was >50% in 53.3% patients, whereas it is seen in 86.7% in PRP group. The incidence of scar hypertrophy of donor site was 10% in control group, whereas it was 6.7% in PRP group [Table 2 and Figure 3]. The mean platelet count in PRP group is 2.46 lakh. Platelet count was also measured in the autologous PRP of all the patients. The mean platelet count of autologous PRP was 5.65 lakh which was found to be 2.3 times the blood platelet levels.

- Donor site PRP group versus conventional group
DISCUSSION
PRP contains a 3–5-fold increase in the concentration of growth factors.[2] α degranulation of platelets causes a burst of growth factors such as insulin-like growth factor 1, transforming growth factor, platelet-derived growth factor, fibroblast growth factor, epidermal growth factor, and vascular endothelial growth factor.[3]
The application of autologous PRP to the STSG sites is believed and proven to provide immediate skin graft adhesion, as well as inosculation of the STSG. Autologous PRP promotes stable hemostasis as it mimics the terminal steps of coagulation cascade. PRP promotes instant adhesion of graft to bed, thereby preventing any collection under the graft or any untoward shearing. In our study we compared two groups of patients, one group underwent STSG by conventional methods, whereas in the other group the wound bed was primed with PRP before resurfacing with STSG. In control group, the donor site was managed by traditional dressing methods as per standard of care, whereas in PRP group, the donor site was also treated with topical application of PRP before the application of the nonadhesive dressing.
Application of PRP on recipient bed prior to placement of skin graft promotes hemostasis and makes the surface sticky by forming fibrin bridges for instant adherence of graft. Platelets in the PRP on coming in contact with collagen get activated and degranulate resulting in the conversion of fibrinogen to fibrin which makes the wound bed sticky. Instantaneous graft adhesion was seen in all the patients in the PRP group, and this finding is consistent with the findings of other studies.[34] Platelets, when degranulate, release various growth factors that promote angiogenesis and hasten the phase of capillary inosculation of graft take. By promoting instant graft adherence and vascularization PRP reduces the incidence of seroma formation, graft edema, and hematoma significantly, which is also seen in other previous studies.[3–5]
As PRP promotes instant graft adhesion and promotes early vascularization, there are decreased instances of soaked dressings and graft failure due to increased moisture, thus reducing the total number of dressings and duration of hospital stay remarkably.
Donor site pain is what makes the postoperative course of skin graft patients more frustrating and is often claimed to be severe than the recipient site pain. This severe pain is routinely attributed to the exposed nerve endings. Various topical and systemic agents were tried to address this issue. Some studies prove that PRP can promote axonal regeneration and reinnervation.[6] In a previous study, they showed that PRP application reduced pain both in terms of subjective Likert scale and narcotic usage.[7] However, there are several limitations to this study. It is a retrospective study, small sample size and comorbid cohort. Another recent retrospective study demonstrated that PRP application could alleviate pain on POD 7, 10, and 14, but not much difference was observed on POD 3 and 21.[8] In our study, we reported appreciable reduction in VAS scores in the immediate and early postoperative period with PRP usage.
Alpha granules of platelets are repositories of various growth factors enumerated previously making PRP rich source of growth factors. There is enormous data supporting the role of PRP in promoting chronic wound healing in various arenas like dentistry, orthopedics, gynecology, and plastic surgery. However, data regarding its role in acute wounds are sparse. A randomized control study comparing PRP gel to conventional dressing in acute wounds showed PRP accelerated wound healing.[9] Our study showed that donor site healing was promoted by PRP application. But in our study, the assessment of healing was subjective. However, in a randomized controlled study, PRP did not significantly improve the epithelization of donor areas.[10]
Incidence of scar hypertrophy of donor area was 10% in control group, whereas it was 6.7% in the PRP group with a P value of 0.64 which is not statistically significant.
CONCLUSION
Application of PRP to the wound bed prior to graft placement promotes instant adhesion of graft to the recipient wound bed and also decreases the incidence of seroma, hematoma, and wound infection. PRP application to donor sites reduces postoperative pain in terms of VAS scores and analgesic usage in the early postoperative period. To our best knowledge, this is the first prospective study to evaluate the effect of PRP on early and immediate postoperative pain of the donor area. Application of PRP to donor site promotes wound healing; however, its effect on reducing scar hypertrophy was not significant. The application of PRP enhances wound healing and has immense economic benefits due to the reduced number of dressing changes and shorter hospital stays.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:638-46.
- [Google Scholar]
- Platelet-rich plasma: From basic science to clinical applications. Am J Sports Med. 2009;37:2259-72.
- [Google Scholar]
- Comparison between control mechanical fixation and use of autologous platelet rich plasma (PRP) in wound beds prior to resurfacing with split thickness skin graft. World J Plast Surg. 2015;4:50-9.
- [Google Scholar]
- Efficacy of autologous platelet rich plasma over control mechanical fixation methods in split thickness skin grafting. Int Surg J. 2019;6:108-13.
- [Google Scholar]
- The effectiveness of autologous platelet rich plasma application in the wound bed prior to resurfacing with split thickness skin graft vs. control mechanical fixation using sutures and staples. World J Plast Surg. 2019;8:185-94.
- [Google Scholar]
- Platelet-rich plasma and the elimination of neuropathic pain. Mol Neurobiol. 2013;48:315-32.
- [Google Scholar]
- Reduction of pain via platelet-rich plasma in split-thickness skin graft donor sites: A series of matched pairs. Diabet Foot Ankle. 2015;6:24972.
- [Google Scholar]
- The use of autologous platelet-rich plasma gel increases wound healing and reduces scar development in split-thickness skin graft donor sites. J Plast Surg Hand Surg. 2019;53:356-60.
- [Google Scholar]
- The use of autologous PRP gel as an aid in the management of acute trauma wounds. Injury. 2009;40:801-5.
- [Google Scholar]
- Effect of topical autologous platelet-rich fibrin versus no intervention on epithelialization of donor sites and meshed split-thickness skin autografts: A randomized clinical trial. Plast Reconstr Surg. 2008;122:1431-40.
- [Google Scholar]






