Translate this page into:
Epidermoid Cyst: An Esthetic Challenge, If Neglected—A Comprehensive Analysis of 217 Cases
Address for correspondence: Dr. Pakesh Baishya, Department of Pathology, Level-3, Medical Teaching Block, All India Institute of Medical Sciences (AIIMS), Rishikesh, Uttarakhand, India. E-mail: pragbaishya@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
An epidermoid cyst is a benign keratin-filled cyst, commonly located in the face, scalp, neck, and trunk. Although it is a common benign cystic neoplasm, large series of analyses in English literature are still scarce. To comprehend the clinical and pathological variation of epidermoid cysts in the sub-Himalayan region of India, as well as their clinical implications for late diagnosis, a retrospective study on epidermoid cysts was conducted.
Materials and Methods:
This was a retrospective observational study conducted on 217 cases of epidermoid cyst subjected for fine-needle aspiration cytology over a period of 3.6 years (from 2018 to 2021). The clinical details and other epidemiological data were archived from the pathology requisition forms.
Results:
It showed slight male preponderance with head and neck site as the most common area. Most patients were adults. Few uncommon sites were also seen namely breast, parotid, epididymis, and tonsils. Few large lesions were identified measuring up to 10 cm. The skin changes were seen in 5.5% cases, 0.9% cases show extreme ulceration, and 4.1% cases show foreign body giant cell reactions. Due to the province’s steep terrain and limited access to medical services, the majority of patients arrived at out patient department (OPD) late.
Conclusion:
The findings suggest that fine-needle aspiration can be used as a quick diagnostic test even in remote areas by the general practitioner who can send the slides for evaluation to a pathologist. Many times, clinically looking epidermoid cyst can reveal certain challenging entities such as a biphasic fibroepithelial tumor with cystic squamous metaplasia and proliferating pilar tumor in our series. The study of this lesion is also needed for early diagnosis as long-standing lesion may rupture and cause requirement of extensive treatment followed cosmetic impairment.
Keywords
Epidermoid
fine needle aspiration
squamous epithelium
INTRODUCTION
An epidermoid cyst is a slow-growing keratin-filled cyst, lined by epidermis-like epithelium in the dermal or subcutaneous location. It is a benign tumor, commonly located in the face, scalp, neck, and trunk.[1] It is developed due to trauma to the pilosebaceous unit of hair follicles in the hair-bearing area.[2] However, there are few case reports on unusual sites including bone, intra breast, spleen, etc. The pathogenesis is still elusive. Although it is a common benign cystic neoplasm, large series of analyses in English literature are still scarce. Many ruptured cysts need extensive prolonged antibiotic therapy before surgical excision which is time-consuming and costly.[23] In this article, we have discussed the clinical and pathological findings of this entity for 3.6 years in the sub-Himalayan region of India.
MATERIALS AND METHODS
All the cases of the epidermoid cyst, diagnosed on fine-needle aspiration cytology from 2018 to 2021 were retrieved from the archive of the Department of Pathology and Laboratory Medicine. Those cases which had histopathology slides were also retrieved for histo-cytological correlation. The patient details were collected from the pathology requisition forms and medical record departments. A retrospective cross-sectional study was performed on the data after obtaining institutional ethical approval.
RESULTS
In this study, 217 cases of epidermoid cysts were included. The age of the patients ranged from 2 to 78 years with a mean age of 36 years. The highest incidence was observed in the age group of 21–30 years (23.9%, 52/217) followed by age groups of 41–50 (23.5%, 51/217) and 31–40 (19.35%, 42/217) years, respectively [Figure 1]. Males were more affected than females with an overall male:female ratio of 1.6:1.
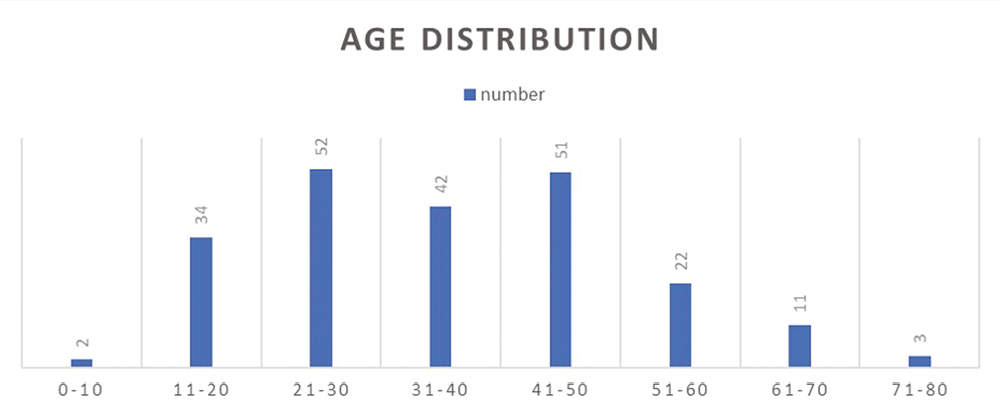
- Demographic data (age range)
The majority of cases were non-tender and demonstrated punctum with unremarkable overlying skin. However, 12 cases showed erythematous skin change and two cases were ulcerated. The average diameter of the lesions was 2.3 cm in our series. The largest in our series measures 10 cm and the smallest measures 0.5 cm in diameter. The largest was located in the right gluteal region of an 18-year-old female. On fine needle aspiration, maximum cases yielded pultaceous material followed by greasy, blood mixed, and pus-like materials.
The head and neck region (62.2%, 135/217) was the most commonly affected region followed by the back (10.1%, 22/217), lower limb (9.6%, 21/217), and upper limb (5.07%, 12/217), respectively [Figure 2]. In the area of the head and neck, the scalp was affected more (22.96%, 31/135) than the face and neck (14.8%, 20/135).
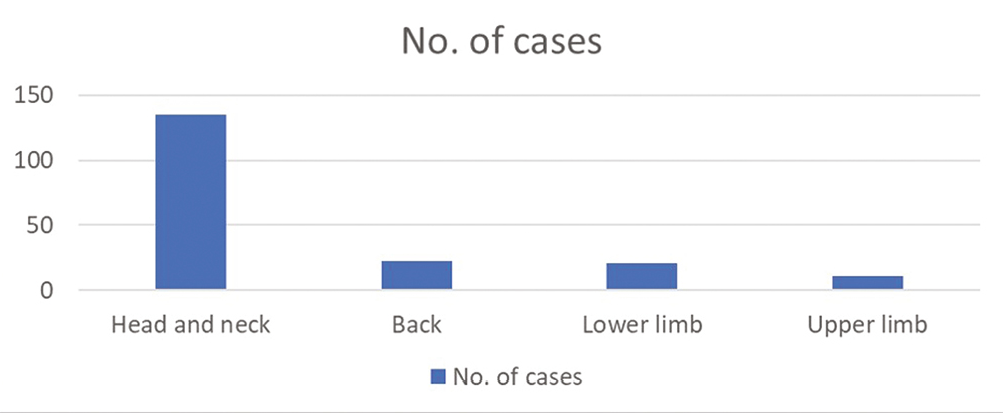
- Different anatomic sites of epidermoid cyst
However, in the lower limb, 28.57% (6/21) cases were seen over foot and thigh respectively followed by gluteal 19.04% (4/21).
Out of 217 cytology cases, histopathology was noted in 52 cases (23.9%). Foreign body giant cell reactions were seen in nine cases (4.1%) on histology along with one case showing dense lymphocytic infiltration in the cyst wall. Five cases (2.3%) were infected epidermoid cyst in histology compared to 29 cases (13.3%) that reported in cytology. Two cases in the head and neck region exhibited calcification in cytology.
The unusual sites observed in this study were breast, tonsillar fossa, oral cavity, parotid gland, fingers, soles, and epididymis [Table 1].
| Unusual site | No. of cases |
|---|---|
| Breast | 10 |
| Parotid gland | 4 |
| Tonsillar fossa | 2 |
| Oral cavity | 2 |
| Epididymis | 1 |
| Soles | 6 |
| Fingers | 2 |
Ten cases were seen at the extra areolar breast region, out of which two were in the intramammary plane and the rest were subcutaneous. All the cases were above 25 years of age. The largest measured 2 cm. Four cases were in the parotid region, of which two were intra-parotid and the rest were subcutaneous [Figure 3]. Both the intra parotid cases underwent resection surgery and subjected for histopathological examination which confirms epidermoid cyst. One case was from the epididymis, which was non-tender, 3 cm in diameter, and revealed blood mixed aspirate.
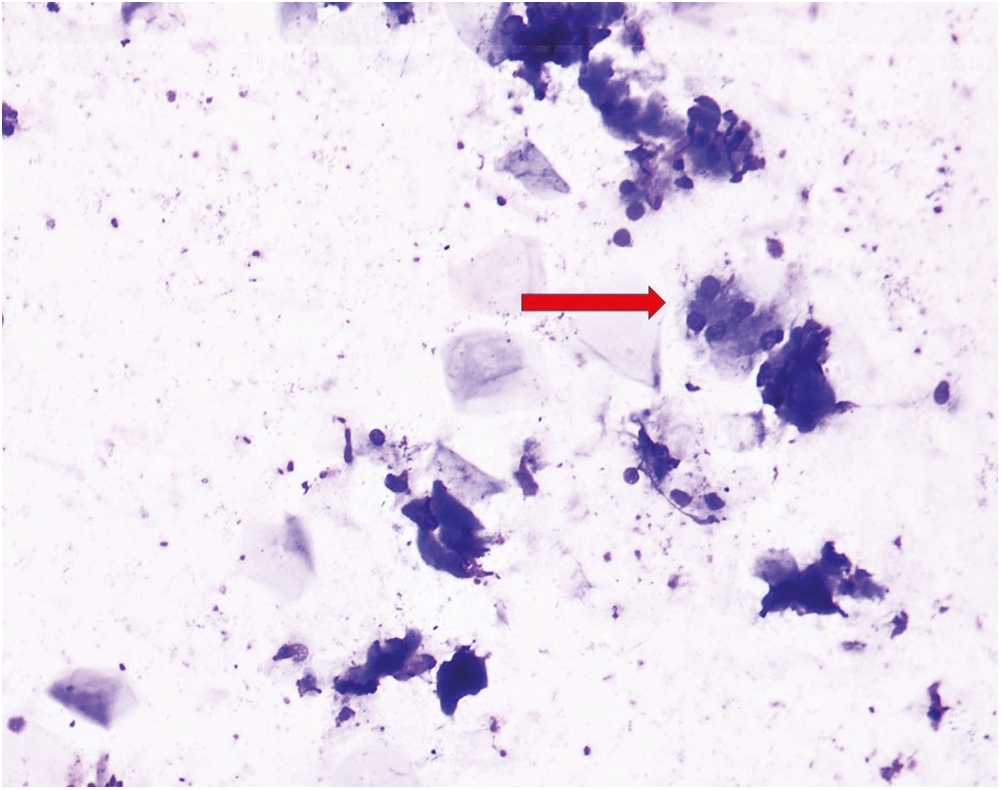
- Smear shows intra parotid epidermoid cyst with salivary ductal and acinar cells (red arrow) (MGG stain, 40×)
The histopathological discrepancy is noted in seven cases.
The trichilemmal cyst was noted in five cases (2.3%) on histology [Figure 4]. Four of them were located on the scalp and one at the chest.
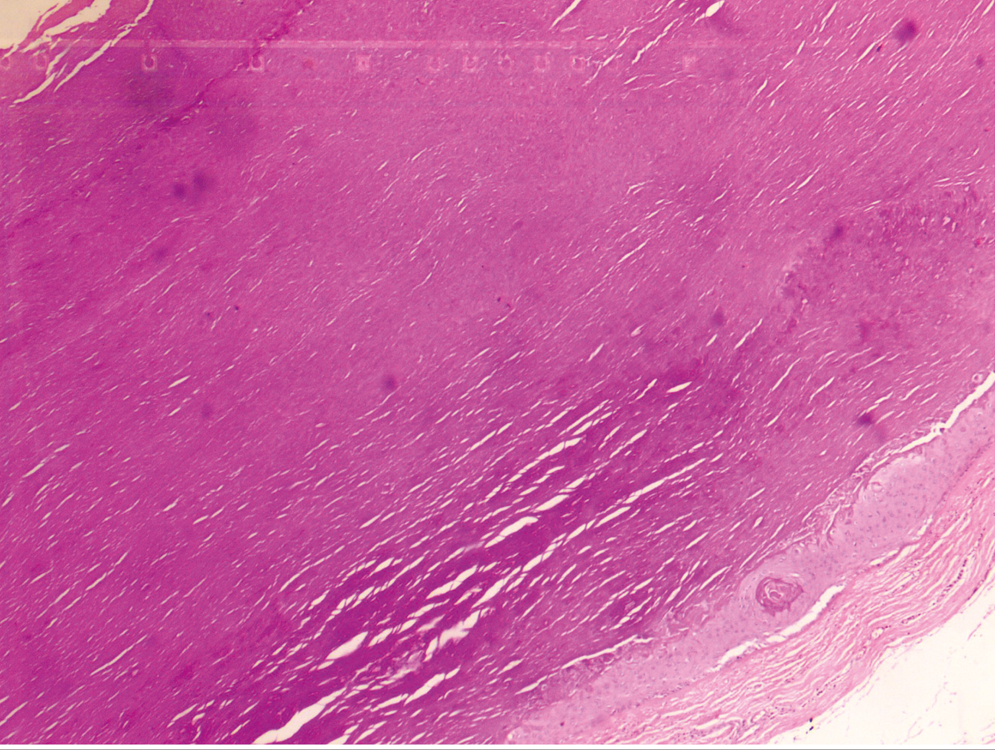
- Histopathology of trichilemmal cyst showing absence of granular layer (Hematoxylin and eosin, 10×)
One case of proliferating pilar tumor was noted in histology. It was located at the nape of the neck and scalp. It measured 10 cm and was multicystic [Figure 5]. On fine needle aspiration, the aspirate was blood mixed and pultaceous with many anucleated squames. Histology showed a pushing border with lobulated contour and bands of squamous epithelium with trichilemmal type keratinization [Figure 6].
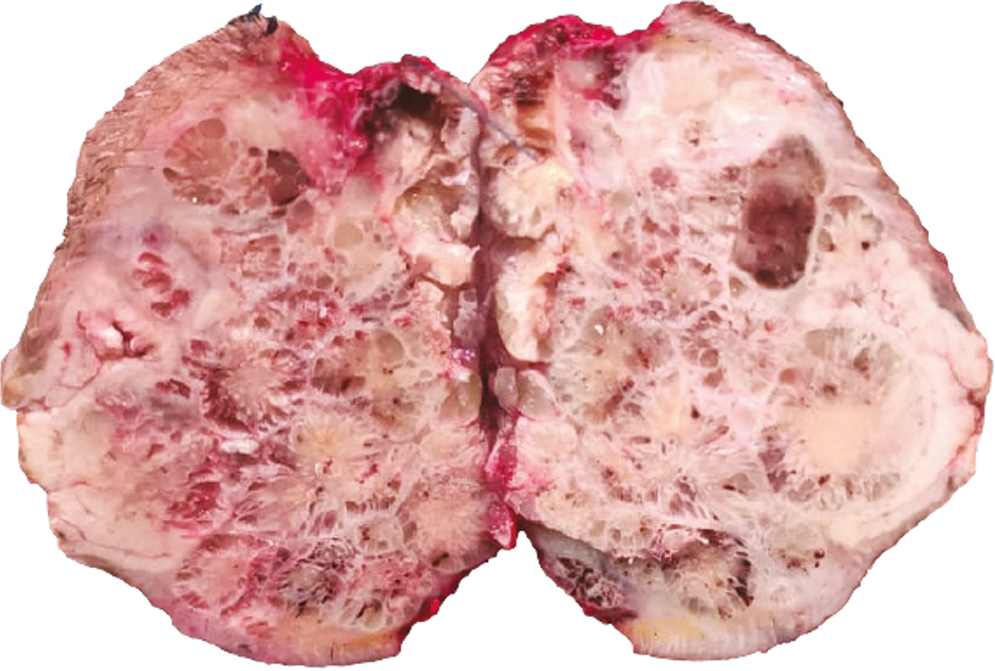
- Skin covered well-demarcated cystic mass, pilar tumor at the nape of the neck region (gross image)
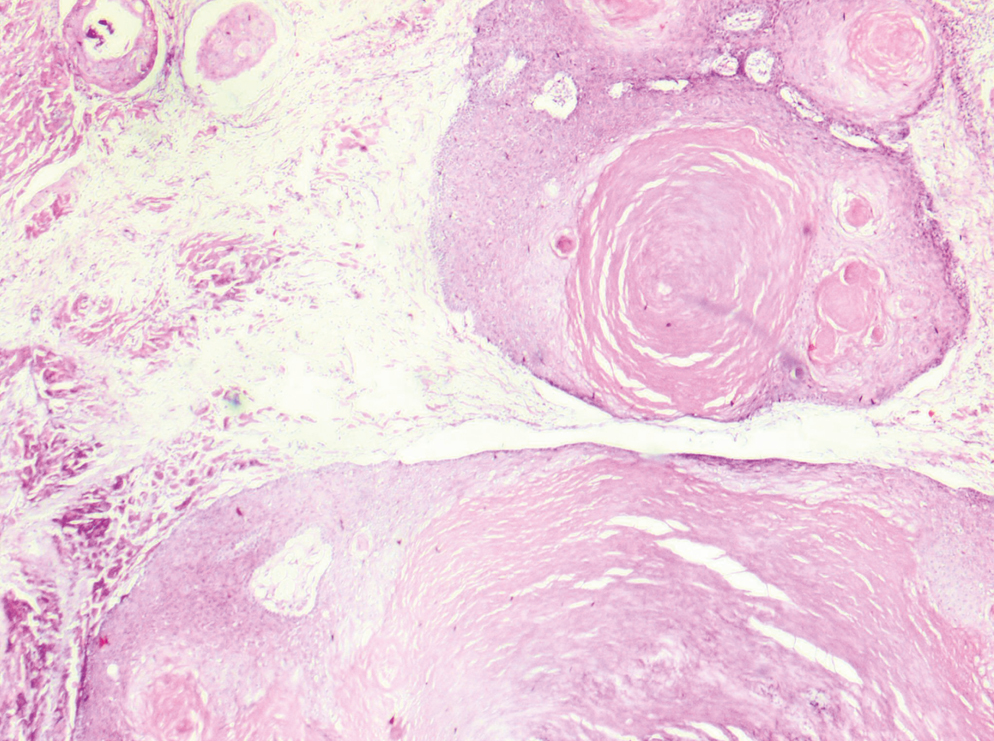
- Histopathology of pilar tumor showing bands of squamous epithelium with trichilemmal type keratinization (Hematoxylin and eosin, 10×)
Another interesting and rare case that was reported as an epidermal inclusion cyst in the breast on histology turned out to be borderline phyllodes tumor. The patient was a 31-year-old women who presented with a rapidly growing mass in the left breast with purulent discharge. The fine needle aspiration cytology shows anucleated squames along with benign ductal epithelial cells and it was reported as an epidermoid cyst [Figure 7]. However, the ultrasonography study of the left breast revealed a large heterogeneous solid cystic lesion with a moderate suspicion of malignancy qualifying for a breast imaging-reporting and data system 4b category. Core biopsy revealed a biphasic fibroepithelial tumor with a proliferation of epithelial and stromal components. The left mastectomy specimen confirmed a biphasic fibroepithelial tumor corroborating the findings of the trucut biopsy. Additionally, areas of stromal overgrowth and tumor infiltration into the adjacent breast parenchyma were identified. Interestingly, the cystic areas were lined by stratified squamous epithelium and filled with anucleate squames [Figure 8A and Band B].
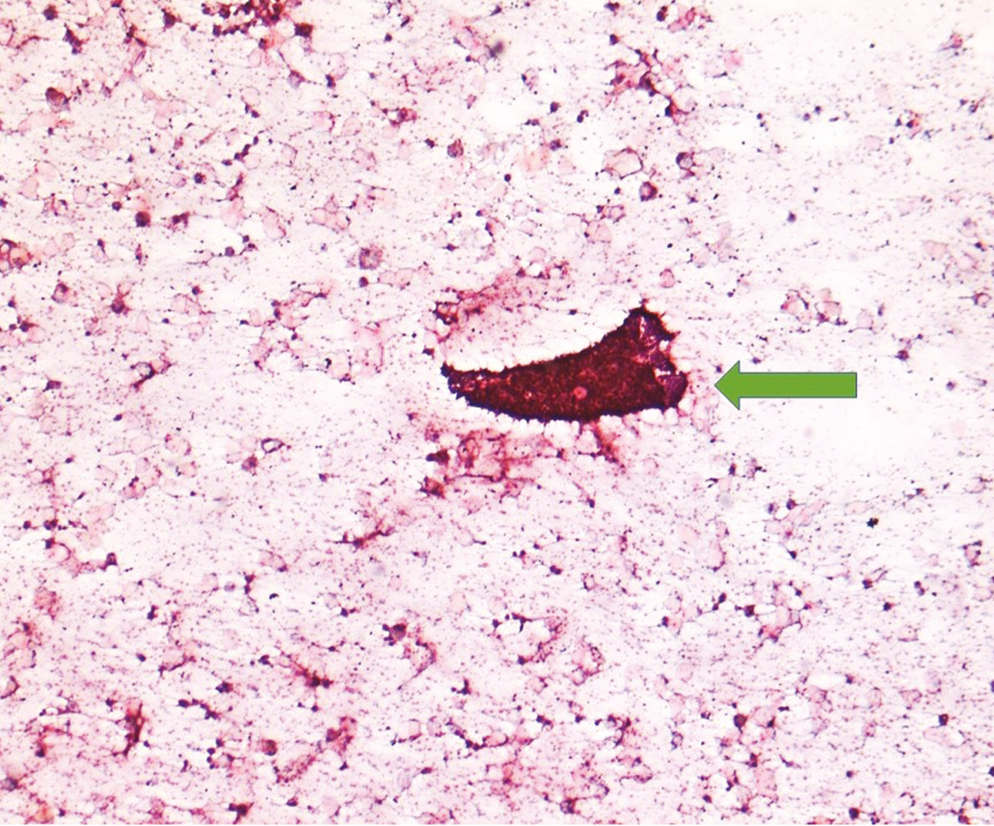
- Smear shows intra mammary epidermoid cyst with anucleated squames with tight cohesive clusters of benign ductal epithelial cells (green arrow) (May grunwald giemsa, 10×)
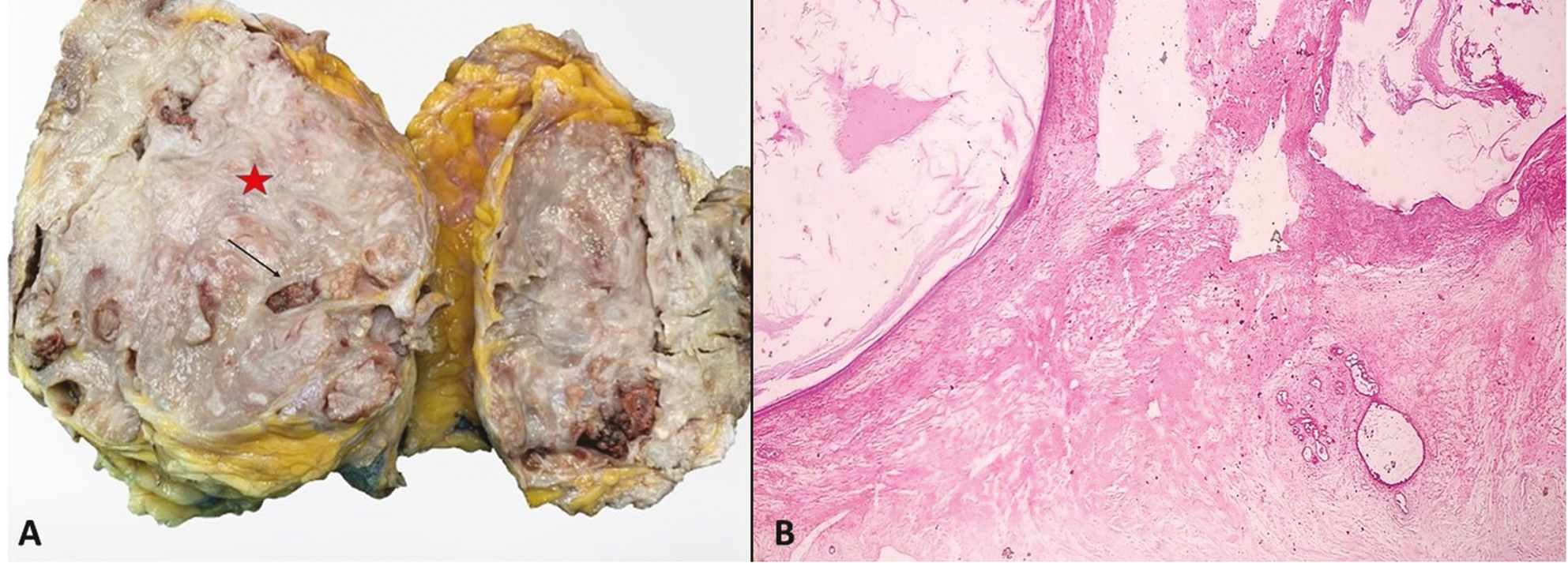
- (A) Mastectomy specimen showing solid (red star) and cystic (black arrow) tumor. (B) Histopathology of mastectomy showing solid cystic tumor with features of epidermoid cyst and borderline phyllodes
DISCUSSION
An epidermoid cyst is a relatively common intra-dermal benign tumor. It occurs mainly because of damage to the pilosebaceous unit; however, due to its presence in unusual sites such as the spleen and other organs, its pathogenesis is still unclear.[12] Although it is common in all age groups, in the present study it is mostly seen in the age group of 20–30 years. These cysts are equally observed in both sexes.[4] This study shows a male preponderance which is similar to the findings of Nigam et al.[3] which was done at an island-based population of the Indian subcontinent. As suggested by Nigam et al.,[3] these could be due to the socioeconomic behavior in the region. The ruptured cysts usually need more cosmetic and medical care. In this study ruptured cysts (2.3%, 7/217) are relatively low in comparison study done by Park and Ko[2] in South Korea (28.2%, 103/359). The epidermoid cyst can be of few millimeters to several centimeters in diameter. Although we have noticed the largest one up to 10 cm in a young girl at the buttock, there are reports of cysts measuring more than 15 cm in diameter in various sites including the ovary.[567]
The majority of the cysts are located at the face, scalp, trunk, and extremities.[1234] These locations make them easily accessible for fine-needle aspiration. In our study, the head and neck region (62.2%, 135/217) was the most common site followed by the back (10.1%, 22/217), lower limb (9.6%, 21/217). In the head and neck region, face and cheek contribute to the highest followed by the scalp. This correlates with the other studies.[123] The unusual sites observed in this study were breast (10/217), parotid gland (04/217), tonsillar fossa (02/217), oral cavity (02/217), and epididymis (01/217) apart from soles (06/217) and fingers (02/217). The soles and fingers are considered unusual sites as they do not contain hair follicles and result mostly due to trauma and human papilloma virus-related infections.[8] The presence of an epidermoid cyst in the epididymis is extremely rare.
The fine-needle aspiration cytology renders a quick diagnosis for these subsets of the lesion as they are easily accessible. However, one needs to keep in mind that other lesions such as pilar cyst, branchial cyst, pilomatrixoma, thyroglossal cysts, and well-differentiated squamous cell carcinoma can be missed due to sampling error in cytology practice [Table 2]. The cytological diagnosis of these entities is of different clinical implications.[91011]
| Entity | Cytology diagnostic clinching points |
|---|---|
| Pilar cyst | Usually at scalp with sparse epithelial component and lack a mixture of anucleate and nucleate squames. Many cholesterol crystals could be seen in the background. |
| Branchial cyst | Aspirate is usually thick, yellow pus-like fluid with mature squamous cells and neutrophils in a background of amorphous debris. Lymphoid tissue is not very evident in cytology. |
| Thyroglossal cyst | Site and location are important. Presence of Mucin secreting cells and/or ciliated columnar epithelial cells could be a clue. |
| Pilomatricoma | Sheets of degenerate, anucleate and keratinized squamous cells with clusters of basaloid cells, calcific debris, and inflammatory cells. If the basaloid cells are scanty or overlooked diagnostic error could may result. |
| Well, differentiated squamous cell carcinoma | Clinical history with cytology showing pleomorphic, hyperchromatic nuclei, coarsely granular chromatin, intense orangophilic cytoplasm, and an occasional mitotic figure. If very well differentiated, biopsy and follow up is recommended. |
In this study, histopathology was noted in 52 cases (23.9%). A total of seven cases were given revised diagnoses. The majority were trichilemmal cysts, which were located at the scalp and chest. Another case was a giant proliferating pilar tumor measuring 10 cm in diameter located at the nape of the neck and scalp. On fine needle cytology, it was reported as a giant epidermoid cyst-based presence of pultaceous material and anucleated squames. However, histology showed a multilobulated mass with squamous epithelium and trichilemmal type of keratinization. Due presence of pushing border without invasion renders a proliferating pilar tumor. These findings were similar to the case reported by Bronfenbrener et al.[12]
As we know, an epidermoid cyst in the breast is a rare entity and clinically and radiologically it imparts a scenario of a malignant tumor.[13] A 31-year-old woman presented with a rapidly growing mass in her left breast. The cytology releveled anucleated squames in a hemorrhagic background. A cytologic diagnosis of the epidermoid cyst was given; however, due to radiological breast imaging-reporting and data system 4b score warrants this case a core needle biopsy. The biopsy confirms a biphasic fibroepithelial tumor with the proliferation of epithelial and stromal components. Following the mastectomy, core needle biopsy findings were confirmed and interestingly the tumor showed a cystic area lined with squamous epithelium and filled with keratin. This case was very challenging and shows an important diagnostic pitfall in breast fine-needle aspiration cytology. Although rare, one has to remember that phyllodes tumor can have cystic squamous metaplasia and may result in erroneous diagnosis in breast cytology.[14]
No malignant lesion was missed in the fine-needle aspiration cytology in the present study.
CONCLUSION
The fine-needle aspiration cytology provides an excellent tool to diagnose the epidermoid cysts and in remote areas general practitioner can prepare the slides and send to pathologist for quick evaluation. One has to pay attention to its clinical features along with the subtle differences in cytologic findings of similar entities for accurate cytologic diagnosis. An early diagnosis helps with cosmetic and therapeutic advantages. Similar entities such as pilomatrixoma have different treatment requirements. A delayed diagnosis with a ruptured cyst has to follow a time-consuming and tedious treatment procedure. One has to be cautiously imparting a diagnosis of epidermoid cyst in rare sites as it may result in disastrous management of such patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Epidermal inclusion cyst: Cytomorphological features and differential diagnosis. Diagn Cytopathol. 2008;36:861-3.
- [Google Scholar]
- A histopathologic study of epidermoid cysts in Korea: Comparison between ruptured and unruptured epidermal cyst. Int J Clin Exp Pathol. 2013;6:242-8.
- [Google Scholar]
- Epidermal cysts: A clinicopathological analysis with emphasis on unusual findings. Int J Trichol. 2017;9:108-12.
- [Google Scholar]
- McKee’s Pathology of the Skin with Clinical Correlations (4th ed.). China: Elsevier Saunders; 2012. p. :1571-4.
- The largest epidermal cyst with vitiligo lesions following female genital mutilation: A case report and literature review. Acta Dermatovenerol Alp Pannonica Adriat. 2018;27:211-3.
- [Google Scholar]
- A large epidermoid cyst developing in the palm: A case report. Int J Surg Case Rep. 2013;4:773-7.
- [Google Scholar]
- A rare case of a giant epidermoid cyst of the ovary. J Clin Diagn Res. 2012;6:1584-6.
- [Google Scholar]
- Cytodiagnosis of simple and proliferating trichilemmal cysts. Acta Cytol. 2001;45:582-8.
- [Google Scholar]
- Head and neck; salivary glands. In: Orell SR, Sterrett GF, Whitaker D, eds. Fine Needle Aspiration Cytology (4th ed.). New Delhi: Churchill Livingstone; 2005. p. :41-82.
- [Google Scholar]
- Fine needle aspiration diagnosis of pilomatrixoma: A monomorphic population of basaloid cells with squamous differentiation not to be mistaken for carcinoma. Acta Cytol. 1991;35:570-4.
- [Google Scholar]
- Benign phyllodes tumor with cystic squamous metaplasia: A cytohistological correlation of a rare case. Iran J Pathol. 2017;12:291-4.
- [Google Scholar]






