Translate this page into:
Evaluation of Wrinkle and Dermal Thickness in the Forearm before and after Picosecond Laser Therapy
Address for correspondence: Dr. Putri Hendria Wardhani, Department of Dermatology and Venereology, Faculty of Medicine, Universitas Airlangga, Dr. Soetomo General Academic Hospital, Jl. Mayjen Prof. Dr. Moestopo No. 6–8, Surabaya 60131, Indonesia. E-mail: putrihendriawardhani@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Skin wrinkles are generated as a result of the aging process. Dermal thickness underneath a wrinkle decreases absolutely. Approximately 20% of dermal thickness disappears as people become elderly. In recent times, people have attempted to reduce wrinkles using various procedures. Currently, available picosecond lasers in dermatology can create mechanical stress and the energy can be fractionated via diffractive lens arrays (DLA). An emerging indication for the picosecond laser includes photorejuvenation. Non-ablative laser skin rejuvenation therapy demonstrates the dermis can be safely reconstructed by only irradiating the skin surface with a laser. The clinical effects of picosecond pulse laser have been frequently reported, but few studies have included histological investigation.
Aims and Objectives:
This study aimed to evaluate wrinkle and dermal thickness in the forearm before and after picosecond laser therapy.
Materials and Methods:
Twenty healthy male and female subjects between 36 and 55 years old with wrinkles in the forearm who met the sample requirements and were willing to participate were recruited in this study. Clinical examination and biopsy for histopathological examination were carried out before and 4 weeks after therapy, then treatment was carried out using a picosecond laser.
Results:
At 1-month follow-up, a significant improvement was noted in wrinkle and dermal thickness (P < 0.05).
Conclusions:
This picosecond 755 nm alexandrite laser with DLA was found to be very effective in treating wrinkles, which was confirmed by a dermatologic assessment from forearm photographic assessment scaled and dermal thickness improvement.
Keywords
Dermal thickness
laser
photoaging
picosecond
wrinkle
INTRODUCTION
As time passes, wrinkles typically appear. Skin wrinkles are generated as a result of the aging process and are a measure of aging. These skin depressions that become deeper and deeper draw more and more coarser lines on almost all the visible parts of an aging individual’s skin. They are indeed the most obvious and maybe disliked signs of skin aging. Wrinkling is thought to be a complex biophysical process resulting from repeated strains on progressively, structurally, and biochemically altered aging skin with impaired mechanical properties.[1] The more dramatic effects of skin aging are seen in the dermis, which is thought to be mainly responsible for the skin's mechanical properties. The dermis provides mechanical strength, resiliency, and elasticity to the skin. During aging, the dermis is submitted not only to quantitative but also qualitative and structural changes. The skin wrinkles are generated mainly in the dermis, associated with decreased collagen contents related to its synthesis and degradation.[2] A significant correlation between the wrinkle depth and dermal thickness at the wrinkle point was found. Dermal thickness underneath a wrinkle decreases absolutely, not relatively. Approximately 20% of dermal thickness disappears as people become elderly.[34]
Although wrinkles are a natural aging process, people want to avoid them. In recent times, people have attempted to reduce wrinkles using various procedures.[2] Currently, available picosecond lasers in dermatology have pulse durations in picoseconds that can create mechanical stress. Picosecond laser energy can be fractionated via diffractive lens arrays (DLA).[56] The application of picosecond lasers continues to expand, and an emerging indication for the picosecond laser includes photorejuvenation. In 2014, the Food and Drug Administration gave clearance for picosecond laser with DLA in the treatment of wrinkles.[7] Nonablative laser skin rejuvenation therapy based on the selective photothermolysis theory, demonstrates the dermis can be safely reconstructed by only irradiating the skin surface with a laser. The clinical effects of irradiation with a picosecond pulse laser have been frequently reported, but few studies have included detailed histological investigation. This study aimed to evaluate wrinkle and dermal thickness in the forearm before and after picosecond laser therapy.
MATERIALS AND METHODS
This study is a comparative analytical study that compares the dermal thickness and clinical wrinkles on the forearm before and after picosecond laser therapy. Twenty healthy male and female subjects between 36 and 55 years old with wrinkles in the forearm who met the sample requirements and were willing to participate in the study by signing the information for consent, informed consent, and a medical action consent form participated in this study. Patients who received previous microdermabrasion, chemical peeling, botox, filler, laser, or other light therapy in the past 6 months were excluded. The exclusion criteria were pregnancy, menopausal female, history of keloid or skin malignancy, photosensitivity, immunosuppressive state, and active infection.
Before the sample was given treatment, a clinical examination of wrinkles and biopsy for histopathological examination was carried out as a pre-test (E0) evaluation, then treatment was carried out using a picosecond laser and after 4 weeks, a clinical examination and biopsy were performed as a postevaluation test (E1). Clinical assessment of wrinkles was photographed and assessed with a dermatologic assessment form forearm photographic assessment scaled to assess the severity of wrinkles on a scale of 0–9. Scale 0: none, 1–3: mild, 4–6: moderate, and 7–9: severe. Each patient received a picosecond 755 nm laser with DLA (Picosure®, Cynosure, Westford, MA, USA), treatment with settings of 0.71 J/cm2 fluence, 6 mm spot size, 10 Hz pulse rate, and a total of 3–4 passes to the forearm. Topical anesthesia was achieved with lidocaine 2.5% and prilocaine 2.5% applied for 30 min before treatment. Patients received a cooling pad and a moisturizer immediately following each treatment. Dermal thickness examination was seen using histopathological examination with hematoxylin and eosin staining. Dermal thickness (µm) is dermal thickness data, which is the average value of dermal thickness measured in (three) different areas. The dermal thickness data were examined at 40× magnification.
RESULTS
Twenty patients were enrolled in this study, predominantly female (95% female, and 5% male) with a mean age of 42.5 ± 6.7 (range 36–55 years). At 1 month follow-up, a significant improvement was noted in wrinkles [Figure 1]. At baseline, the average scale was 4.75, at the 1-month follow-up the average score improved to 2.7 (P < 0.05). A lower score means fewer wrinkles [Table 1].
| Group | n | Wrinkle | P value | |
|---|---|---|---|---|
 ± SD ± SD |
Min–Max | |||
| Pretest | 20 | 4.75 ± 0.64 | 4.00–6.00 | 0.000 |
| Posttest | 20 | 2.70 ± 0.57 | 2.00–4.00 |

- Comparison of wrinkles before and after therapy. Left: before therapy. Right: after therapy
Table 2 shows the results of measuring the dermal thickness in each group. It appears that the dermis thickness in the pre-est group with an average of 699.00, whereas the posttest group with an average of 820.32. These results indicate that the dermal thickness in wrinkles treated with picosecond laser is higher than before [Figure 2].
| Group | n | Dermal thickness | P value | |
|---|---|---|---|---|
 ± SD ± SD |
Min–Max | |||
| Pretest | 20 | 699.00 ± 75.56 | 609.98–922.80 | 0.000 |
| Posttest | 20 | 820.32 ± 108.85 | 640.50–956.26 |
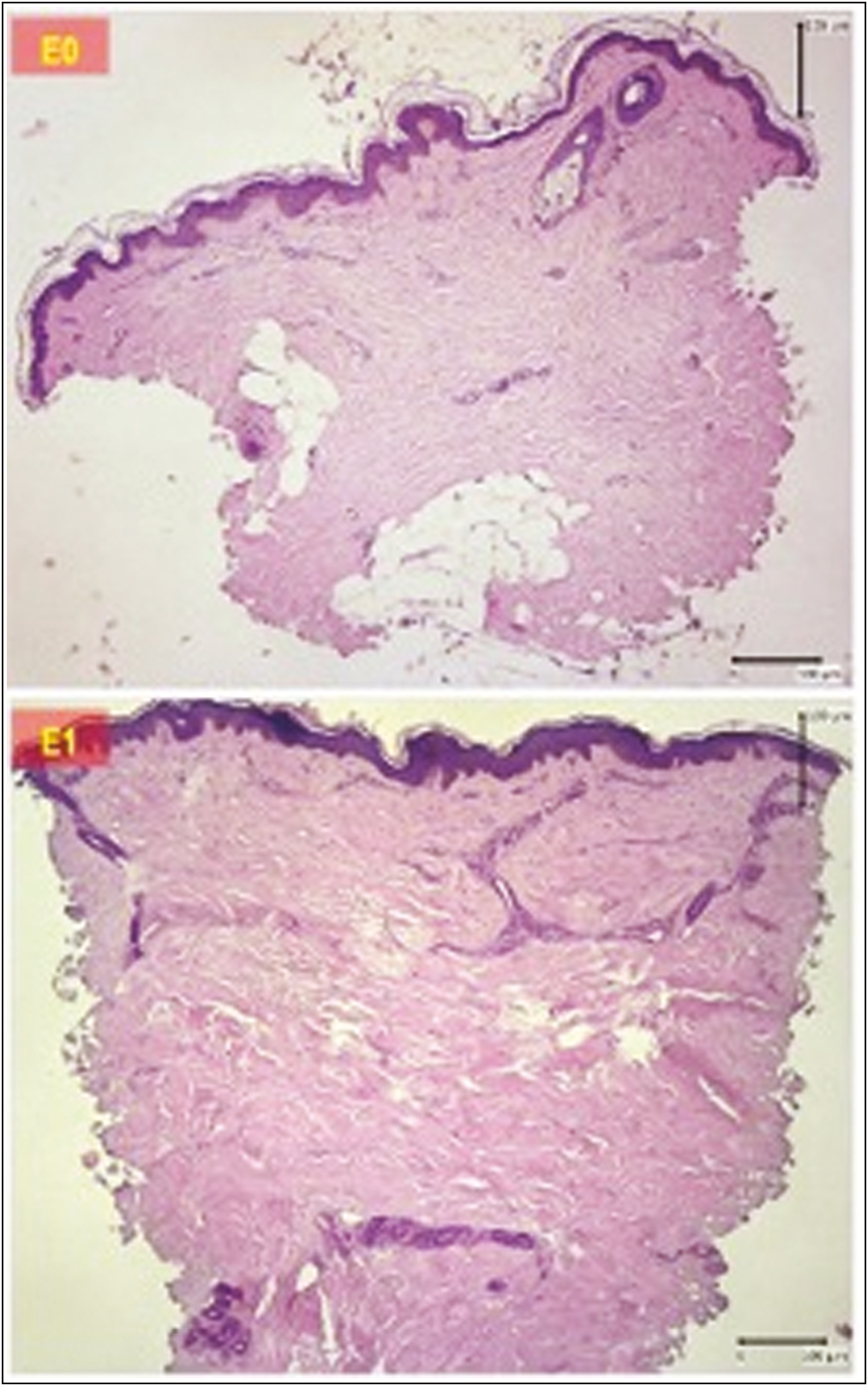
- Comparison of dermal thickness before and after therapy. Upper: before therapy. Lower: after therapy
DISCUSSION
This is a study to evaluate wrinkle and dermal thickness in the forearm before and after picosecond laser therapy. This picosecond 755 nm alexandrite laser with DLA was found to be very effective in treating wrinkles, which was confirmed by a dermatologic assessment from forearm photographic assessment scaled and dermal thickness improvement. This picosecond laser creates a greater degree of photomechanical damage and reduces the degree of nonspecific photothermal effects, thereby enhancing the specificity of energy delivered to target molecules. When used in conjunction with the DLA, it offers the added benefits of fractionation. A unique mechanism of tissue injury induces laser-induced optical breakdown (LIOB) in the epidermis and papillary dermis, which may confer superior healing characteristics. The DLA redistributes the laser beam into peaks of high fluence surrounded by a low fluence background.[8] In the epidermis or dermis, cavities termed LIOB are sporadically formed that may influence a layer deeper because of the larger peak power. These localized epidermal vacuoles were associated with the deposition of new dermal collagen. Keratinocytes produce several growth factors, chemokines, and cytokines in response to injury or a wound. These factors and agents could stimulate and regulate the response to this injury through receptors on epidermal and dermal cells. It has been speculated that the rapid vacuole formation with the generation of an LIOB could create a pressure fluctuation in the skin that propagates into the dermis. This barotrauma and the presence of a cytokine network between the epidermis and dermis may lead to changes in the dermis that result in dermal improvement.[910] This could also result in the initiation of dermal remodeling from changes in cell signaling and the release of cytokines from alterations in cellular membranes.[1112] A significant clinical and dermal thickness improvement was detectable as early as 1 month. Remodeling of the dermis may be induced following the mechanism of wound healing. Nakano[9] reported in the skin treated by picosecond laser-toning therapy, rejuvenation of the entire dermis with reconstructions was confirmed. The dermal thickness increased and collagen bundles were regenerated in the reticular layer.[9]
Picosecond 755 nm laser with DLA is an effective option for increasing the dermal thickness and leading to wrinkle improvement but further exploration of this technology is still needed. Both unfractionated and fractionated delivery modes should be explored to achieve optimal results and comparative trials with other modalities would also be interesting.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Funding from the researchers themselves.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The work was supported by Surabaya Skin Centre, Surabaya, Indonesia, and PT Mediva, Jakarta, Indonesia.
REFERENCES
- Menopause, ultraviolet exposure, and low water intake potentially interact with the genetic variants related to collagen metabolism involved in skin wrinkle risk in middle-aged women. Int J Environ Res Public Health. 2021;18:2044.
- [Google Scholar]
- The relationship between wrinkle depth and dermal thickness in the forehead and lateral canthal region. Arch Dermatol. 2011;147:822-8.
- [Google Scholar]
- Safety and efficacy of novel diffractive lens array using a picosecond 755 nm Alexandrite laser for treatment of wrinkles. Lasers Surg Med. 2017;49:40-4.
- [Google Scholar]
- A systematic review of picosecond laser in dermatology: Evidence and recommendations. Lasers Surg Med. 2021;53:9-49.
- [Google Scholar]
- Evolution of the picosecond laser: A review of literature. Dermatol Surg. 2019;45:183-94.
- [Google Scholar]
- Efficacy and safety of picosecond 755-nm Alexandrite laser with diffractive lens array for non-ablative rejuvenation in Chinese skin. Lasers Surg Med. 2019;51:8-13.
- [Google Scholar]
- Histological investigation of picosecond laser-toning and fractional laser therapy. Laser Ther. 2020;29:53-60.
- [Google Scholar]
- Safety of a picosecond laser with diffractive lens array (DLA) in the treatment of Fitzpatrick skin types IV to VI: A retrospective review. J Am Acad Dermatol. 2016;74:931-6.
- [Google Scholar]
- The histology of skin treated with a picosecond alexandrite laser and a fractional lens array. Lasers Surg Med. 2016;48:646-52.
- [Google Scholar]
- Comparison of the cutaneous thermal signatures over twenty-four hours with a picosecond Alexandrite laser using a flat or fractional optic. J Drugs Dermatol. 2016;15:1347-52.
- [Google Scholar]






