Translate this page into:
Exploring surgical outcomes of elliptical excision against relaxed skin tension lines on the face
*Corresponding author: Yogesh M. Bhingradia, Department of Dermatology, Shivani Skin Care and Cosmetic Clinic, Surat, Gujarat, India. yogeshbhingradia@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhingradia YM, Sadhwani M, Rawat A, Kulkarni O, Patel R, Gandra S, et al. Exploring surgical outcomes of elliptical excision against relaxed skin tension lines on the face. J Cutan Aesthet Surg. doi: 10.25259/JCAS_70_2024
Abstract
Objectives
The excisional surgeries on the face are usually carried out along relaxed skin tension lines (RSTLs). However, when the long axis of the lesion cannot be oriented along the RSTL, it becomes imperative to plan excision, which although it may not follow the RSTL, still would help to reduce wound tension and scarring. This study aims to compare the surgical outcomes of elliptical excision along RSTL versus those against RSTL over the face.
Materials and Method
A retrospective, randomized, and comparative study was carried out on 100 patients who had undergone elliptical excision either against RSTL (Group A) or along RSTL (Group B) for various indications on the face. A modified Vancouver scar scale (VSS) was used to assess the scar after 6 months. Comparison of categorical data was performed by the Chi-square test and Fisher’s exact test, while Mann compared the quantitative data–Whitney Z test. P < 0.05 was considered significant.
Results
Fifty patients were included in Group A and Group B each. Maximum (32%) excisions in Group A were carried out on the forehead, whereas 52% of cases who were operated along RSTL had lesions on the cheek. The common indications for elliptical excision on the face were compound nevus (35%) and post-traumatic scar (39%). About 11% of the total cases developed minor complications postoperatively. The mean modified VSS between the two groups was found to be statistically insignificant (P = 0.364).
Conclusion
We can hereby postulate that elliptical excisions that do not follow RSTL on the face can give equally convincing surgical outcomes as compared to the ones aligned along the RSTL, provided that we give sufficient strength to the wounds by placement of subcutaneous sutures. The concept of biodynamic excisional skin tension lines can thus be emphasized.
Keywords
Elliptical excision
Face surgery
Relaxed skin tension lines (RSTL)
INTRODUCTION
The orientation of surgical incisions plays a crucial role in minimizing scarring after excisional surgeries, especially on the face. Karl Langer, who originally investigated cleavage lines, studied cadavers that were punctured with a round-tipped awl (like an ice-pick).1 Cox, who recreated Langer’s experiment in 1941, also marked out skin cleavage lines.2
Relaxed skin tension lines (RSTL), which are the natural lines of least tension in the skin, are often recognized as a guiding principle for planning a surgical incision. Surgeries planned according to RSTL have been believed to promote wound healing and reduce chances of scarring.
However, wound closures using biodynamic excisional skin tension (BEST) lines offer a new guide to minimize wound complications after excisional surgery. BEST lines aid in reducing wound tension, which has been shown time and again to minimize scarring.3
This article aims to compare the outcomes of elliptical excision surgeries carried out along and against RSTL on the face. By evaluating the modified Vancouver scar scale (VSS), we aimed to investigate the differences in scar formation between the two techniques.
MATERIAL AND METHODS
A retrospective, randomized, and comparative study was carried out on 100 patients who had undergone elliptical excision over the face from February 2019 to February 2024.
Patients were randomly assigned to one of the two groups: Group A: Elliptical excision against RSTL Group B: Elliptical excision along RSTL.
Data collected from the medical records included Patient demographics (age, gender, etc.), characteristic of the lesion (diagnosis, size, and location), surgical details (suture type), wound healing outcomes, complications, and scar assessment after 6 months (modified VSS assessed by two independent observers).
The inclusion criteria included:
Patients who underwent elliptical excisions for skin lesions on the face
Patients with clear documentation of incision orientation (along or against RSTL)
Patients with follow-up data on wound healing and scarring.
The following cases were excluded from the study.
Lesions such as cysts and lipomas which were removed by incision
Patients with complex medical histories or comorbidities that could significantly impact wound healing
Pregnant and lactating females
Malignant skin lesions such as squamous cell carcinoma and melanoma
Patients with insufficient follow-up data.
The pre-operative size of the lesion was calculated. Elliptical excisions were performed by using standard surgical techniques, keeping in mind the principle of length: width ratio of at least 3:1. The wound was closed in two layers (interrupted, subcutaneous closure followed by vertical mattress skin closure) using 6-0 Polyamide black nonabsorbable suture material for both the layers. All patients were prescribed oral antibiotics postoperatively and were followed up after 1 week for suture removal. Thereafter, monthly follow-ups were conducted for up to 6 months. Comparison of categorical data between the two groups was performed by the Chi-square test and Fisher’s exact test, while Mann compared the quantitative data–Whitney Z test and Kruskal–Wallis test. P < 0.05 was considered significant using the Statistical Package for the Social Sciences 23.0 version.
RESULTS
The mean age of presentation in Group A and Group B was 30.64 (standard deviation [SD]: 12.876) years and 32.54 (SD: 12.407) years, respectively. The overall mean age of patients was 31.59 ± 12.61 years. The sex ratio was as follows: Group A had 26 females (52%) and 24 males (48%), while Group B had 29 females (58%) and 21 males (42%).
In Group A, 16 cases (32%) had lesions over the forehead, while in Group B, 26 cases (52%) had lesions over the cheek. About 93% of the lesions were <3 cm in diameter, whereas 7% of them were more than 3 cm in diameter. The overall common indications for elliptical excision on the face were compound nevus (35%) and post-traumatic scar (39%) [Figure 1]. Other less common indications included basal cell carcinoma, chalazion, chicken pox scar, congenital melanocytic nevus, keloid, hypertrophic scar, mature tattoo, pyogenic granuloma, and seborrheic keratoses. A significantly higher number of cases of compound nevi were excised along the RSTL (46% of Group B cases). With respect to post-traumatic scar cases, RSTL was mostly not followed during excision (48% of Group A cases) [Table 1].
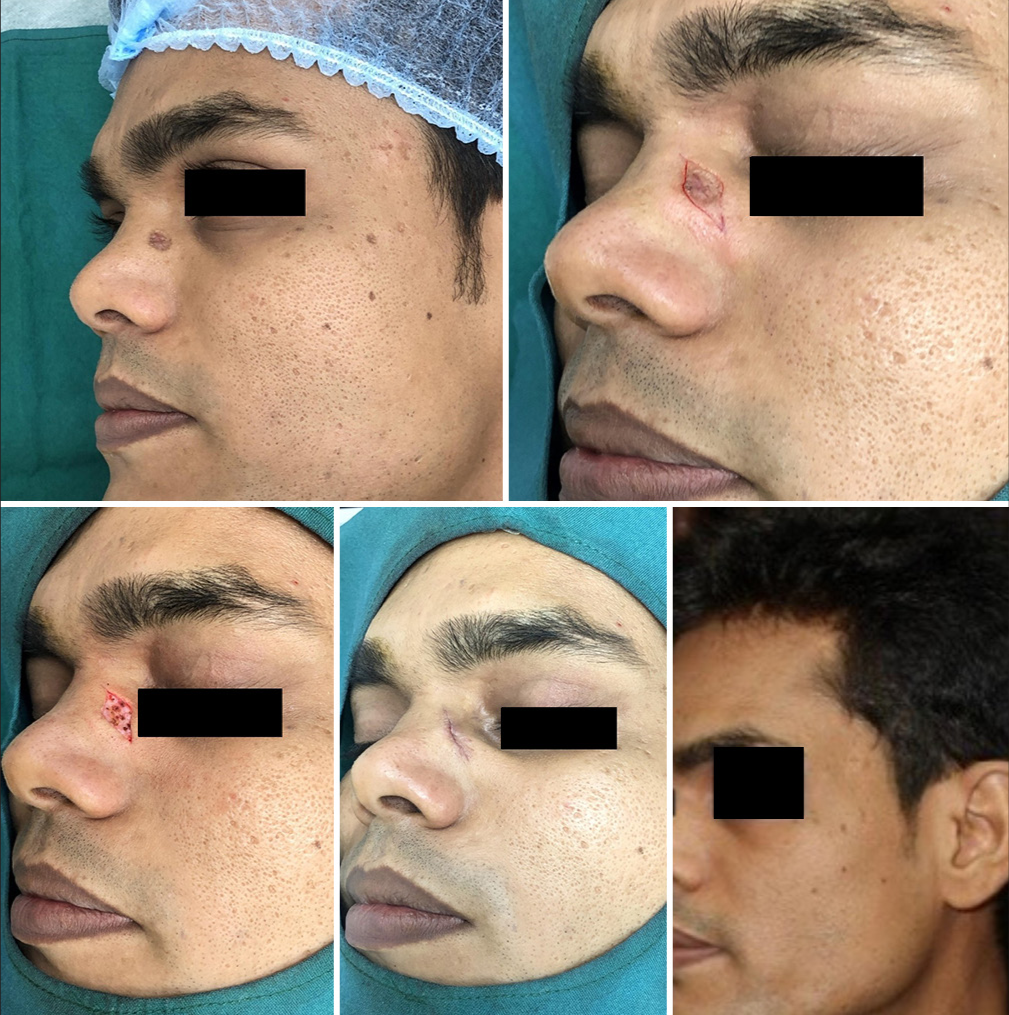
- A 32-year-old male patient with post-traumatic scar over left side of nasal bridge, who underwent elliptical excision along the relaxed skin tension line, leading to excellent recovery after 6 months.
| Group | P-value by Fischer’s exact test | ||||
|---|---|---|---|---|---|
| Group A | Group B | ||||
| Number of cases | Percentage | Number of cases | Percentage | ||
| Site of lesion | |||||
| Cheek | 12 | 24.0 | 26 | 52.0 | 0.020 |
| Chin | 6 | 12.0 | 8 | 16.0 | |
| Eyelid | 0 | 0.0 | 1 | 2.0 | |
| Forehead | 16 | 32.0 | 6 | 12.0 | |
| Infraorbital | 1 | 2.0 | 0 | 0.0 | |
| Lateral canthus | 1 | 2.0 | 0 | 0.0 | |
| Lip | 0 | 0.0 | 1 | 2.0 | |
| Nose | 14 | 28.0 | 8 | 16.0 | |
| Total | 50 | 100.0 | 50 | 100.0 | |
| Diagnosis | |||||
| Basal cell carcinoma | 2 | 4.0 | 3 | 6.0 | 0.028 |
| Chalazion | 0 | 0.0 | 1 | 2.0 | |
| Chicken pox scar | 0 | 0.0 | 4 | 8.0 | |
| Compound nevus | 12 | 24.0 | 23 | 46.0 | |
| Congenital melanocytic nevus | 4 | 8.0 | 2 | 4.0 | |
| Keloid | 1 | 2.0 | 0 | 0.0 | |
| Hypertrophic scar | 1 | 2.0 | 0 | 0.0 | |
| Mature tattoo | 1 | 2.0 | 2 | 4.0 | |
| Pyogenic granuloma | 4 | 8.0 | 0 | 0.0 | |
| Seborrheic keratoses | 1 | 2.0 | 0 | 0.0 | |
| Traumatic scar | 24 | 48.0 | 15 | 30.0 | |
| Total | 50 | 100.0 | 50 | 100.0 | |
Post-operative side effects were observed in 11% of the total cases (Group A: five cases, Group B: six cases). Secondary infection (four cases), worsening of scar (three cases), wound gaping (three cases), and recurrence of lesion (one case) were noted.
The mean modified VSS in Group A was 2.1 ± 1.3 and that in Group B was 1.9 ± 0.8. The difference between the two groups was found to be statistically insignificant (P = 0.364) when assessed with Mann–Whitney test [Figure 2].
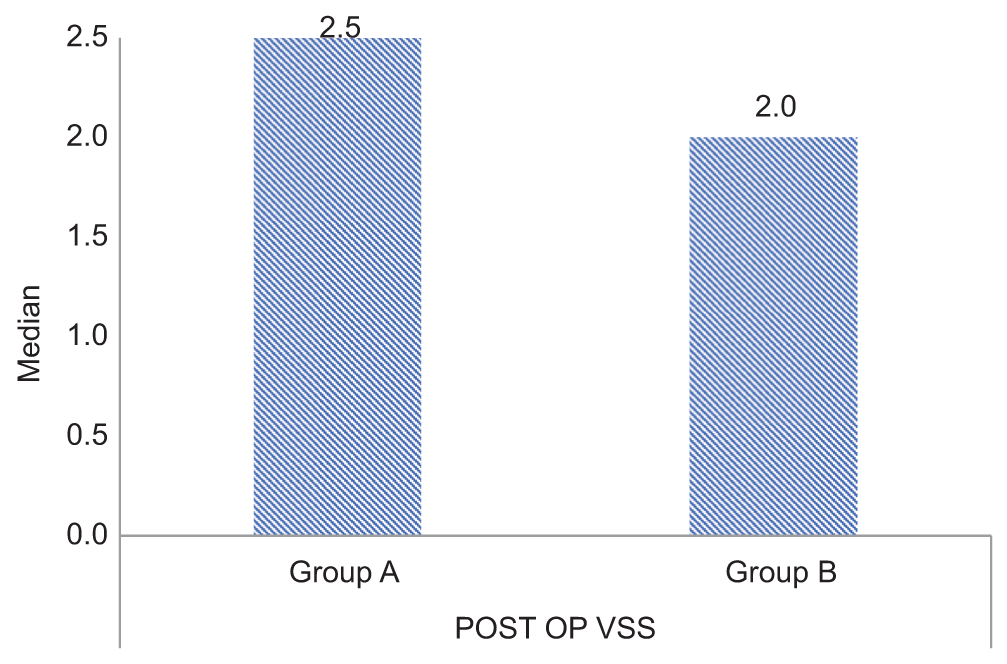
- Comparison of the mean modified vancouver scar scale between Group A and Group B (P = 0.364). POST OP VSS: Post operative vancouver scar scale.
DISCUSSION
There is an ongoing debate regarding the proper orientation of incisions in relation to the RSTL. While some surgeons advocate for “excision along RSTL” to minimize scar visibility, others believe that “excision against RSTL” will offer better wound closure with reduced tension along the edges if we consider BEST lines at such places.
The term RSTLs were coined by Borges, who suggested these lines to be used as a guide for facial surgeries. Paul defined the concept of BEST lines using a tensiometer to determine the line of wound closure after excisions on the trunk.4 When the forces acting on a wound are increased after the excision of skin lesions, as opposed to creating incisions merely for egress, the dynamics change. The stretching of skin not only changes the structural anatomy of the skin but causes ultrastructural, cellular, and chromatin stretch that results in altered genetic signals. Therefore, the term BEST lines was coined. Their study revealed that there was a statistically significant reduction in wound closure tension when BEST lines were used as compared to RSTLs.
In our study, lesions on the cheek were mostly excised along RSTL [Figure 3] (52% cases of Group B), while more lesions on the forehead were excised against RSTL [Figure 4] (32% cases of Group A). This observation goes in favor of the orientation of BEST lines over the forehead, which tends to run vertically, contrary to the horizontal placement of RSTL. In 24 out of the 39 cases of post-traumatic scars, RSTL was not followed during excision. The reason for the same is that while excising scars, we tend to follow the long axis of the scar, irrespective of its alignment with the RSTL [Figure 5]. On the other hand, 23 out of 35 cases of compound nevi were excised keeping in mind their plane along the RSTL. However, in rest of the cases of compound nevi, excision was done against the RSTL [Figure 6].

- Excisional biopsy along relaxed skin tension line of a plaque over the right nasolabial fold. The histopathology confirmed it to be basal cell carcinoma with tumor-free margins.
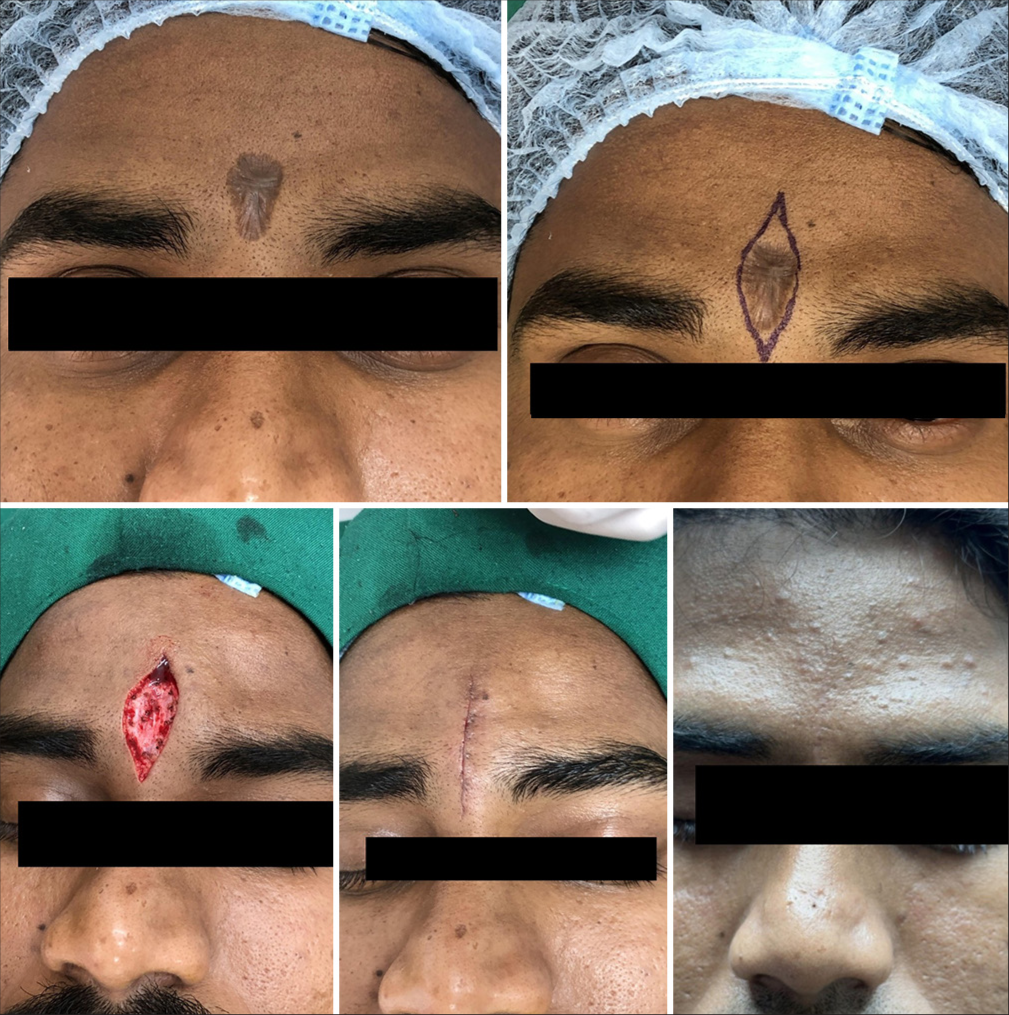
- Traumatic scar over the glabella excised vertically (against relaxed skin tension line), resulting in complete recovery after 6 months.

- Post-traumatic scar over the left cheek, which was oriented horizontally was excised along its long axis.

- Elliptical excision of compound nevus, done against the relaxed skin tension line, resulting in an inconspicuous scar.
Five cases of Group A and six cases of Group B developed minor complications post-surgery, such as secondary infection, gaping of the wound after suture removal, worsening of the existing scar, and recurrence of the lesion.
However, there was no statistically significant difference in the above side effects among the two study groups (P = 0.795). The presence of side effects positively correlated with the post-operative mean modified VSS score of more than 3 (P = 0.029), indicating that any hindrance in postoperative wound healing would lead to a relatively unsightly scar.
We could not find a statistically significant correlation between the site of lesion, pre-operative size, and diagnosis with the post-operative mean modified VSS score in each of the study groups.
After calculating the mean modified VSS after 6 months of surgery, it was found that 90% of the total cases had a score of <3, while only 10% cases had a scar count of more than 3. The mean VSS score between the two groups was not found to be statistically significant (P = 0.364). We can, therefore, decipher that the surgical outcome of the lesions excised against RSTL is similar to the ones excised along RSTL on the face. To provide additional support to the wounds created against RSTL, we emphasize the role of interrupted, nonabsorbable, and subcuticular sutures.5 Such closures decrease the chances of dog ear formation, indentation marks and wound gaping. In a study conducted by Sommerlad and Creasey,6 continuous subcuticular nylon suture, carefully inserted into the dermis and left for 3 weeks, was found histologically to be the best way to minimize scar stretching.
The findings of this study shall also give valuable insights to surgeons by helping them select the most appropriate incision for elliptical excision used to treat various conditions, especially on the face.
One of the limitations of our study was that a tensiometer was not used to compare the wound tension created along the edges after excision with both techniques. Furthermore, the site of excision was limited only to the face. A uniform suturing technique for skin closure of all the wounds could not be followed.
CONCLUSION
Based on the findings of this study, there was no statistically significant difference in surgical outcomes between excisions performed on the face in accordance with RSTL and those that did not adhere to these guidelines. Favorable outcomes in elliptical excision against RSTL can be achieved by supplementing them with subcuticular closure of the wound. Thus, alternative techniques such as flaps and grafts can be avoided in such cases. While RSTL may be a valuable consideration in surgical planning, strict adherence to it may not always be essential for achieving satisfactory results. Further research is warranted to explore the factors that may influence the impact of RSTL on surgical outcomes. These factors could include the specific anatomical region, type of incision, and the individual patient’s characteristics.
Authors’ contribution
All the authors have contributed to the concept, design, literature search, data analysis, statistical analysis, manuscript preparation, manuscript editing and review.
Ethical approval
The Institutional Review Board approval is not required as it was a retrospective, observational study analysis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- On the anatomy and physiology of the skin. I. The cleavability of the cutis. Br J Plast Surg. 1978;31:3-8.
- [CrossRef] [Google Scholar]
- Release of mechanical tension triggers apoptosis of human fibroblasts in a model of regressing granulation tissue. Exp Cell Res. 1999;248:608-19.
- [CrossRef] [Google Scholar]
- Biodynamic excisional skin tension lines for surgical excisions: Untangling the science. Ann R Coll Surg Engl. 2018;100:330-7.
- [CrossRef] [PubMed] [Google Scholar]
- Utilization of nonabsorbable (polyamide black) buried subcutaneous suture material in closure of elliptical excision in various indications for better aesthetic outcome. J Cutan Aesthet Surg. 2021;14:215-9.
- [CrossRef] [PubMed] [Google Scholar]
- The stretched scar: A clinical and histological study. Br J Plast Surg. 1978;31:34-45.
- [CrossRef] [PubMed] [Google Scholar]







