Translate this page into:
Fractional Carbon Dioxide Laser versus Fractional Carbon Dioxide Laser with Autologous Intralesional Platelet-rich Plasma in the Treatment of Stable, Non-segmental Vitiligo: A Randomized Comparative Study
Address for correspondence: Dr. Bikash Ranjan Kar, Department of DVL, Institute of Medical Sciences & SUM Hospital, Siksha O Anusandhan University, Bhubaneswar 751003, Odisha, India. E-mail: karbikash@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
The treatment of vitiligo is often challenging and requires a multi-modality approach. Fractional carbon dioxide (FCO2) laser has been studied as an adjuvant therapy in cases of vitiligo. Autologous platelet-rich plasma (PRP) is rich in growth factors, which may contribute to the growth of melanocytes, and thus help in the repigmentation of vitiligo patches. We aimed to study the combination of these two modalities for the treatment of vitiligo.
Aims and Objective:
The aim of this study was to compare the efficacy and safety of FCO2 laser with PRP and FCO2 laser alone as an adjuvant therapy in stable non-segmental vitiligo (NSV) patients.
Settings and Design:
A prospective, randomized, comparative, open-label interventional study was carried out for a period of 18 months from December 2017 to June 2019, at a tertiary care hospital.
Materials and Methods:
Seventy patients with stable, NSV were assessed for eligibility; 66 patients were randomized equally into two groups. Group A received treatment with FCO2 laser with intralesional PRP, whereas Group B was treated with FCO2 laser alone. Patients in both the groups were treated with one therapy session and were followed up monthly for a period of 3 months. All the patients received topical psoralen with ultraviolet A (UVA) PUVA-sol treatment. Baseline and monthly assessments were done by VITILIGO AREA SEVERITY INDEX and standardized photographs.
Results:
VASI score reduction was significantly more in the Group A with (mean ± standard deviation [SD]) 9.5 ± 0.22, 5.8 ± 1.12, and 3.6 ± 1.81 as compared to Group B 11.9 ± 2.83, 9.9 ± 3.11, and 8.9 ± 3.46 at each subsequent follow-up visits, respectively. Side effects such as burning sensation, erythema, and crusting were seen less frequently and lasted for a short period in Group A in comparison to those in Group B.
Conclusion:
Combination of FCO2 laser and autologous intralesional PRP has a synergetic effect in treating patients with vitiligo as an adjuvant therapy with minimal adverse effects.
Keywords
Autologous platelet-rich plasma
fractional carbon dioxide laser
non-segmental vitiligo
VASI score
INTRODUCTION
Vitiligo is an acquired disorder of depigmentation characterized by a decrease in the number and selective destruction of functioning melanocytes. The etiology is hypothesized to be multifactorial comprising immunological, genetic, environmental, and autoimmune influences.[1]
Therapy in vitiligo is aimed at arresting the spread of the disease and causing repigmentation. The latter is achieved by increased mitosis, an increase in the number of melanocytes and melanosomes, and their transfer into surrounding keratinocytes. This induction of melanocytes is usually achieved by psoralen and ultraviolet A (UVA) (PUVA). Few physical and biological modalities such as fractional carbon dioxide (FCO2) laser treatment have been postulated to cause melanocyte stimulation in vitiligo.
FCO2 laser acts by the principle of fractional thermolysis, and it has been postulated to improve vitiligo by shrinkage of the vitiliginous area, migration of melanoblasts from adjoining normal skin, and post-inflammatory pigmentation.[234]
Platelet-rich plasma (PRP) is a biological cocktail of multiple growth factors.[5] The possible mechanism of PRP in vitiligo could be due to these growth factors enhancing the proliferation of keratinocytes and fibroblasts. PRP could also increase the interaction of melanocytes with keratinocytes and stabilize the melanocytes.[6]
FCO2 laser and autologous PRP have been individually studied in the treatment of vitiligo. We conducted this study to analyze the efficacy and safety of combining FCO2 laser and PRP over FCO2 laser alone as an adjuvant therapy in stable non-segmental vitiligo (NSV).
MATERIALS AND METHODS
This is a randomized, comparative, open-label, interventional study. All patients with stable NSV who presented to the department of dermatology at a tertiary care hospital between December 2017 and June 2019, were recruited for the study.
Institutional ethics committee approval was obtained before the study, and written informed consent was obtained from the patients.
Sample size calculation
The sample size was estimated by Raosoft software to be 67, for a population size of 80 with a 95% confidence interval for a period of 18 months. A total of 70 patients were enrolled considering possible dropouts. The inclusion criteria for the study were patients with NSV of either gender between the ages of 18 and 50 years with stable disease for at least a year, patients being off any topical or systemic treatment for at least last 3 months, and vitiligo patches with size between 25 and 50 cm2. Exclusion criteria for the study were patients with any history of keloid, infections such as herpes, human immunodeficiency virus, and hepatitis B virus infection, diabetes mellitus, hypertension, cardiopulmonary insufficiency, collagen vascular disease, bleeding tendency, or coagulation disorders. Pregnant or lactating women, patients with unrealistic expectations, and vitiligo on mucosal areas, scalp, palms, and soles were also excluded.
Allocation, flow, and final analysis of patients are given in Figure 1.
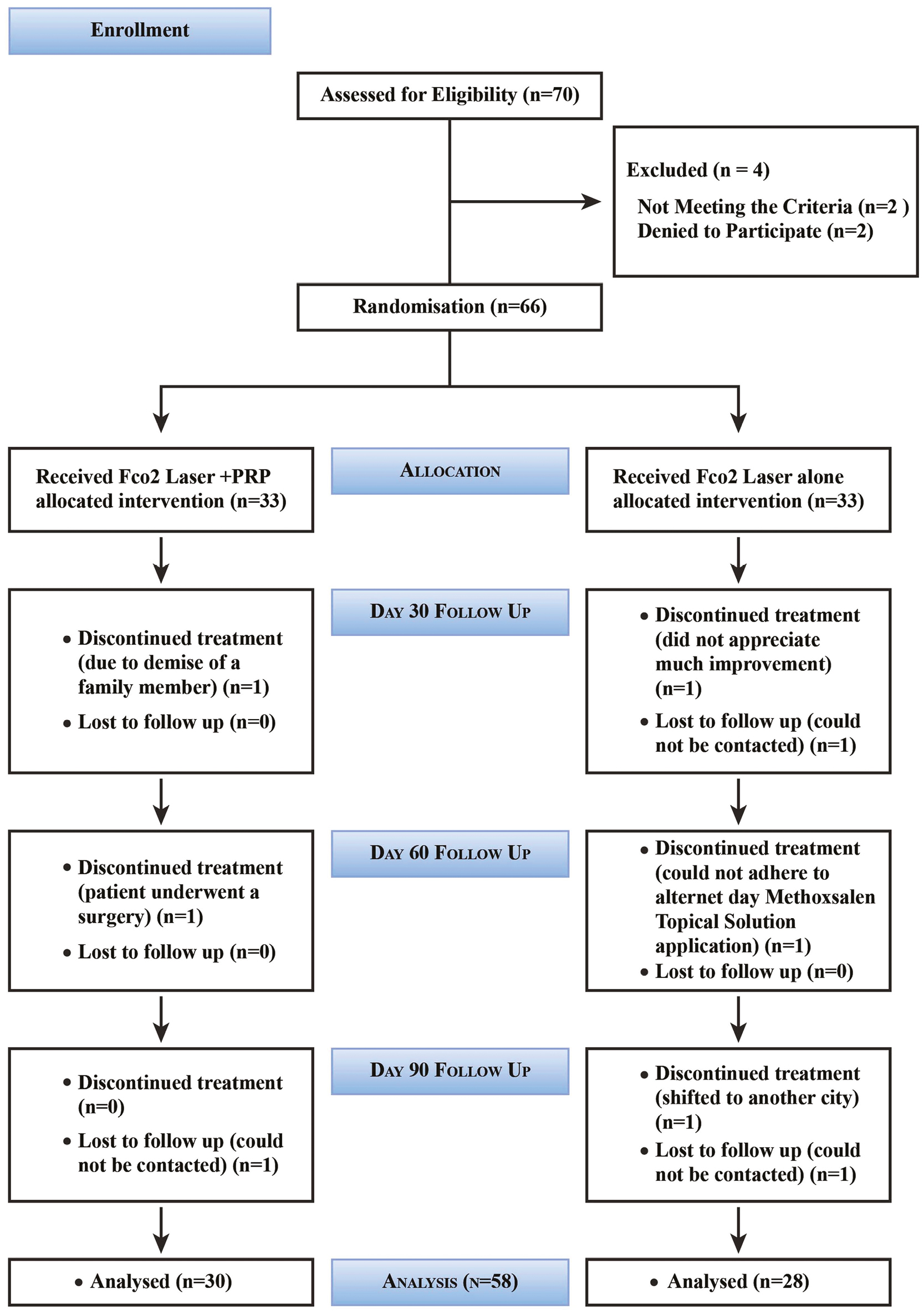
- Flow chart depicting passage of participants through four different stages of the study
Assessment tools
Vitiligo improvement was assessed according to the VASI score.
A standardized digital photograph was obtained with a Canon EOS 70D camera (Tokyo, Japan), at baseline and on each subsequent visit, and was evaluated by a blinded observer.
Safety evaluation
Assessment of adverse effects was done during and after each session based on the complaints by the patients and the observation of skin responses such as erythema, edema, crust formation, scarring, pigmentary changes, infection, or any allergic manifestations.
FCO2 laser device
A 30 W ablative FCO2 laser device (model: FIRE XEL from Bison Medical approved by the Korean FDA) was used. Topical anesthesia cream was applied 45 min before the procedure. The depigmented area was lased with the following parameters: 1 mm density, 1500 µs pulse width, 3000 microsecond repeat delay, 9 times overlap, and 202.5 mJ energy.
PRP preparation
A total of 20 mL blood was drawn from the patient’s medial cubital vein using a syringe under aseptic conditions and was then transferred to a vial containing anticoagulant citrate dextrose solution formula A (ACD-A). It was centrifuged at 1500rpm for 10 min using a REMI R-8C centrifuge (REMI R-8C centrifuge (REMI ELEKTROTECHNIK, Korea)). The supernatant was transferred to another sterile conical bottom tube without any anticoagulant. The second tubes were centrifuged at 3000rpm for 10 min. The platelet pellets collected at the bottom of the tubes were obtained. Homogenized platelet pellets were thoroughly mixed into 2 mL of plasma at the bottom of the tube. The homogenized mix was then injected via the intralesional route into the vitiliginous sites after FCO2 laser. The treatment site was covered with JELONET Paraffin gauze dressing, (Smith & Nephew, India).
Statistical analysis
Paired t test was used to compare the VASI score in the same group in both the treatment arms, and the unpaired t test was implicated to compare two different treatment arms (Group A and Group B) at the baseline, and on each subsequent follow-up visits (Day 30, 60, and 90).
A P value <0.05 was considered to be significant.
All the calculations for the study were done using Microsoft Excel (version: Microsoft Office Professional Plus 2016 for Windows).
RESULTS
The mean age of the participants in Group A and Group B was 31.43 ± 8.19 and 32.17 ± 8.63 years, respectively. The mean duration of lesion stability was 18.13 ± 7.48 and 19.71 ± 8.77 months in Group A and Group B, respectively. The gender, age, duration of lesion stability, and the distribution of the lesions were comparable between the groups at the baseline as shown in Table 1.
| Variables of the participants | Group A (FCO2 laser + PRP) (n = 30) (%) | Group B (FCO2 laser alone) (n = 28) (%) | P value |
|---|---|---|---|
| Gender | |||
| Male | 13 (43.3) | 9 (32.1) | 0.10 |
| Female | 17 (56.6) | 19 (67.8) | |
| Age (in years) | |||
| 18–30 | 15 (50) | 13 (46.4) | 0.61 |
| 30–50 | 15 (50) | 15 (53.5) | |
| Duration of lesional stability | |||
| 1–2 years | 21 (70) | 18 (64.2) | 0.38 |
| >2 years | 9 (30) | 10 (35.7) | |
| Location of the lesions | |||
| Limb | 13 (43.3) | 16 (57.1) | 0.15 |
| Trunk | 17 (56.6) | 12 (42.8) |
The value in bold is 0.10, which is more than 0.05, signifying that the difference in Gender based sub-group between both the treatment groups is not statistically significant
The mean VASI score in both the groups was comparable at the baseline (P = 0.066). The VASI score was significantly lesser in Group A versus Group B at each of the subsequent visits at the first, second, and third month, which is shown in Table 2.
| VASI baseline (mean ± SD) | VASI 1st follow-up (mean ± SD) | VASI 2nd follow-up (mean ± SD) | VASI 3rd follow-up (mean ± SD) | |
|---|---|---|---|---|
| Group A (FCO2 laser + PRP) | 12.1 ± 0.85 | 9.5 ± 0.22 | 5.8 ± 1.12 | 3.6 ± 1.81 |
| Group B (FCO2 laser alone) | 12.7 ± 2.88 | 11.9 ± 2.83 | 9.9 ± 3.11 | 8.9 ± 3.46 |
| P value | 0.066 | 0.001 | 0.0001 | 0.0001 |
A comparison of mean VASI score reduction was done between the baseline with subsequent three follow-up visits in both the groups. The difference between the mean VASI scores at each of the visits when compared with the baseline VASI score was found to be highly significant [Table 3].
| Comparison between baseline and 1st follow-up visit | Comparison between baseline and 2nd follow-up visit | Comparison between baseline and 3rd follow-up visit | |
|---|---|---|---|
| Group A (FCO2 laser + PRP) | Mean ± SD: 2.57 ± 0.82 | Mean ± SD: 6.31 ± 1.55 | Mean ± SD: 8.52 ± 1.85 |
| P value: 0.0001 | P value: 0.0001 | P value: 0.0001 | |
| Group B (FCO2 laser alone) | Mean ± SD: 0.79 ± 0.38 | Mean ± SD: 2.70 ± 0.70 | Mean ± SD: 3.75 ± 1.14 |
| P value: 0.004 | P value: 0.0001 | P value: 0.0001 |
Results of subgroup evaluation: All the patients were divided into two groups, each according to the four variables taken into consideration in the study, namely gender, age, duration of lesion stability, and location of lesions, to evaluate and compare the difference between the baseline and third follow-up mean VASI score, to assess response of the intervention in both the treatment arms.
Group A: No significant difference was observed in the VASI scores between the third visit and the baseline with respect to the gender of the study population. Patients of the age group of 18–30 years showed more decrease in the mean VASI score at the third visit than the age-group 30–50 years (P = 0.003). We found no significant difference in the change in VASI score between the patients of different durations of lesion stability, that is, more and less than 2 years in both the groups. The lesions on the trunk had a significantly higher decrease in VASI score between the baseline and final follow-up than the lesions on the limbs (P = 0.011) [Table 4].
Group B: The study did not reveal any significant difference between the VASI scores at the baseline versus third follow-up visit based on gender. Patients of the age-group of 18–30 years showed significantly more decrease in the mean VASI score than the age-group of 30–50 years at the third follow-up (P = 0.015). No significant difference was observed in the change in VASI score between the patients of different durations of lesional stability, that is, more and less than 2 years. Lesions on the trunk again showed a significant decrease in the VASI score than the lesions on the limb in this group similar to Group A [Table 5].
| FCO2 laser + PRP Group A (n = 30) | Gender | Age | Lesional stability | Location of the lesion | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M (n = 13) | F (n = 17) | P value | 18–30 years (n = 15) | 30–50 years (n = 15) | P value | <2 years (n = 21) | >2 years (n = 9) | P value | Limb (n = 13) | Trunk (n = 17) | P value | |
| VASI baseline | 13.0 ± 3.5 | 11.4 ± 3.5 | 0.21 | 11.7 ± 2.9 | 12.9 ± 3.1 | 0.23 | 12.7 ± 3.7 | 10.6 ± 2.6 | 0.10 | 10.4 ± 1.57 | 9.9 ± 1.34 | 0.20 |
| VASI 3rd follow-up | 4.2 ± 3.8 | 3.1 ± 2.4 | 0.38 | 3.01 ± 0.12 | 3.76 ± 0.7 | 0.003 | 4.05 ± 3.57 | 2.53 ± 1.37 | 0.104 | 6.5 ± 2.3 | 4.3 ± 2.01 | 0.011 |
| FCO2 laser alone Group B (n = 28) | Gender | Age | Lesional stability | Location of the lesion | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M (n = 9) | F (n = 19) | P value | 18–30 years (n = 13) | 30–50 years (n = 15) | P value | <2 years (n = 18) | >2 years (n = 10) | P value | Limb (n = 16) | Trunk (n = 12) | P value | |
| VASI baseline | 12.7 ± 2.3 | 12.6 ± 2.9 | 0.93 | 13.5 ± 2.91 | 12.2 ± 2.45 | 0.07 | 13.09 ± 2.85 | 11.9 ± 2.51 | 0.30 | 11.01 ± 0.31 | 10.81 ± 0.38 | 0.15 |
| VASI third follow-up | 8.54 ± 2.6 | 9.13 ± 3.0 | 0.60 | 8.62 ± 2.57 | 9.31 ± 3.22 | 0.015 | 9.27 ± 3.09 | 8.35 ± 2.41 | 0.39 | 7.33 ± 1.23 | 5.89 ± 1.54 | 0.013 |
Pain and burning sensation subsided within a day, and erythema and crusting subsided within a week after laser treatment without affecting the course of treatment. Infection, scarring, Koebner phenomenon, or further aggravation of vitiligo was not seen in any patient [Table 6].
| Adverse effects reported by the participants | Group A (FCO2 laser + PRP) (n = 30) (%) | Group B (FCO2 laser alone) (n = 28) (%) |
|---|---|---|
| Pain (mild to moderate) | 30 (100) | 28 (100) |
| Burning sensation | 23 (76.6) | 28 (100) |
| Erythema | 20 (66) | 25 (89.2) |
| Crusting | 11 (36.6) | 19 (67.8) |
| Scarring | Nil | Nil |
| Koebner phenomenon | Nil | Nil |
| Infection | Nil | Nil |
| Aggravation of vitiligo | Nil | Nil |
Standardized photographs of the patients at the baseline and after 90-day follow-up visit are shown in Figure 2A and B for Group A and Figure 3A and B for Group B.
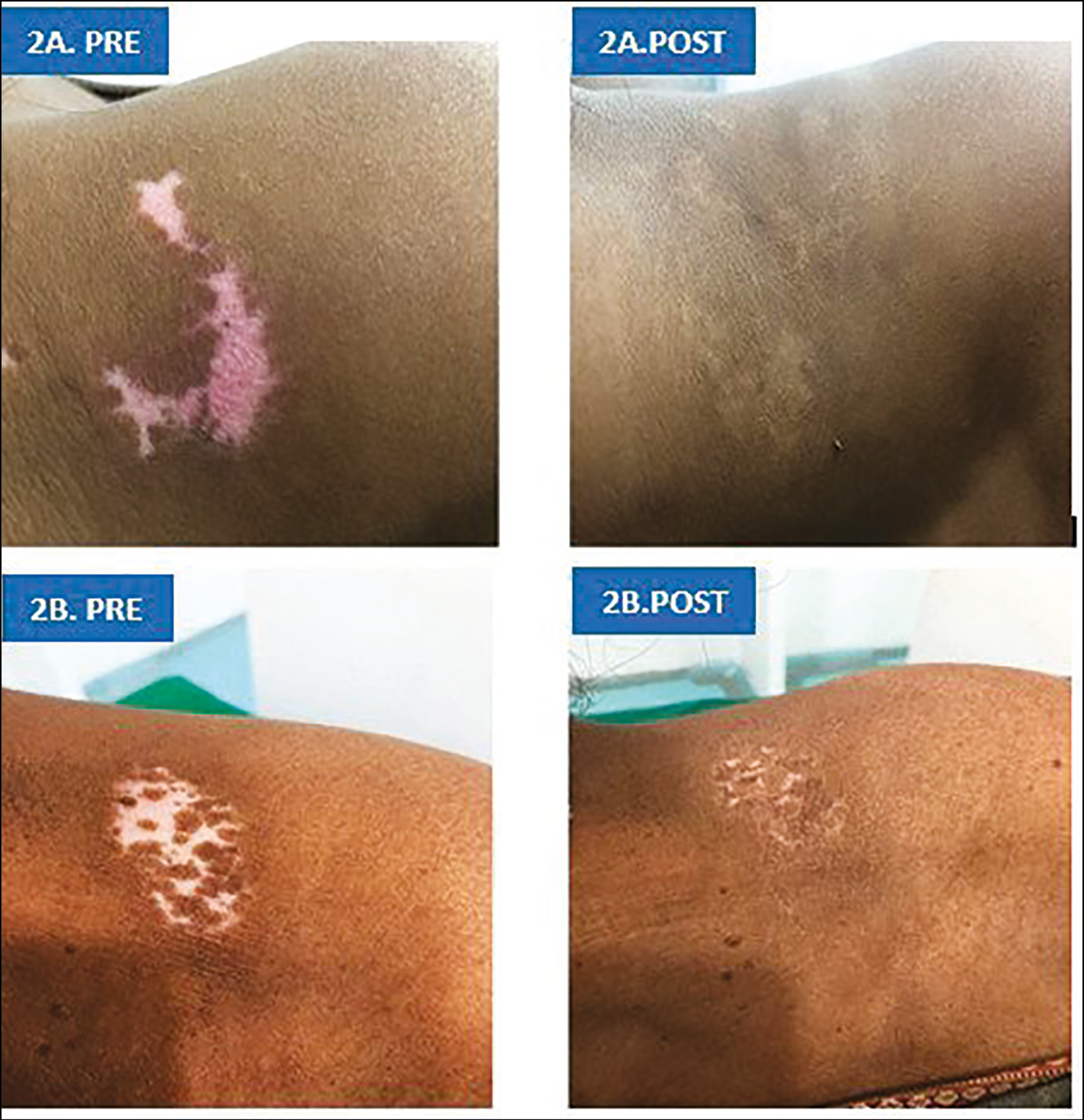
- (A) and (B): Pre (at the baseline) and post (after 90-day follow-up visit) vitiligo patch on left supraclavicular area and left shoulder in Patient 1 and 2, respectively in Group A
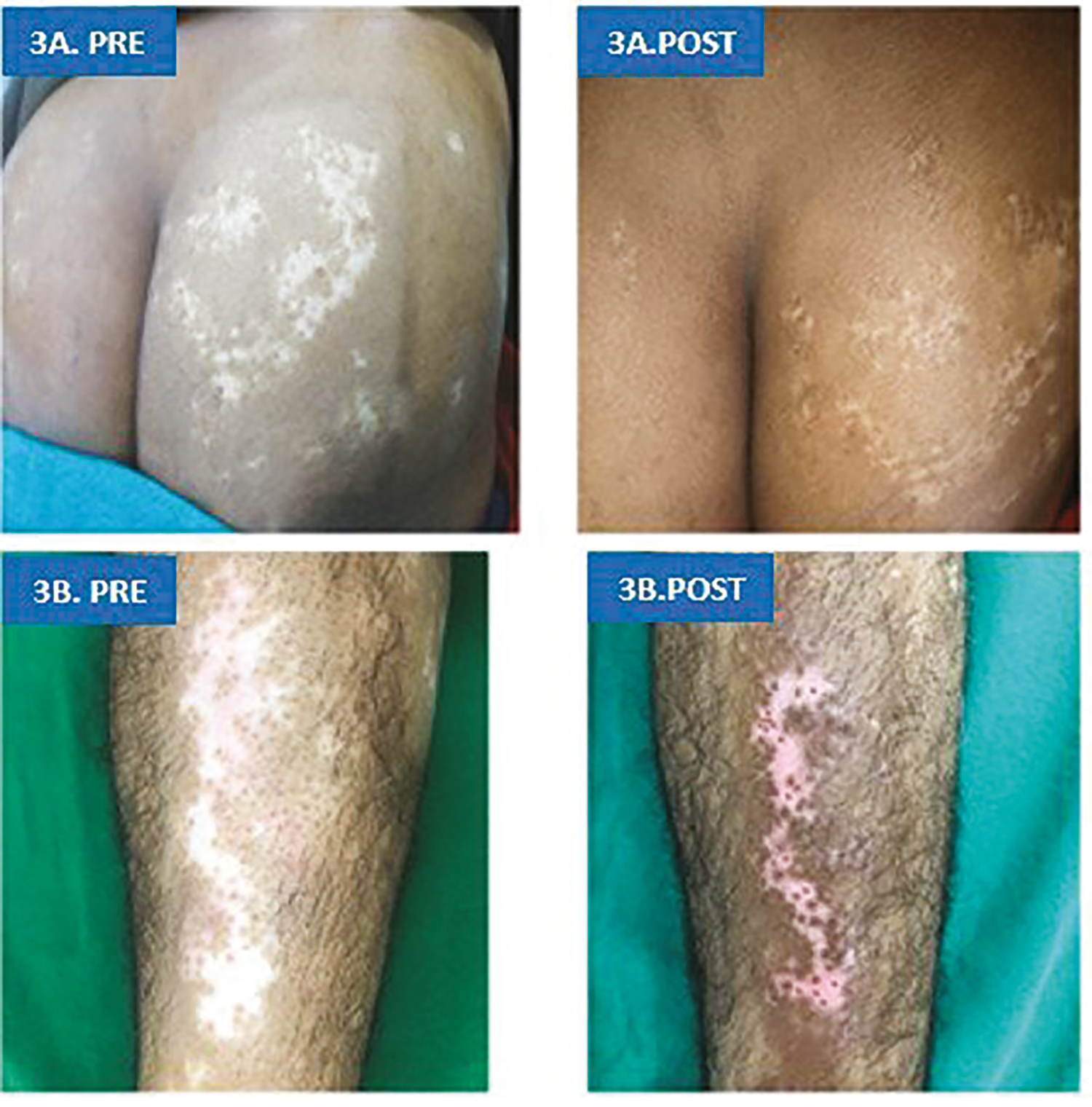
- (A) and (B): Pre (at the baseline) and post (after 90-day follow-up visit) vitiligo patch on right buttock and left shin of tibia in Patient 1 and 2, respectively in Group B
DISCUSSION
Females outnumbering males in our study are in concordance to previous studies.[4678] Increased social consequences in girls and women affected by vitiligo make them seek medical attention more than males.[9]
The mean age of patients was comparable to the study population in a study by Kadry et al.[7] and Abdelghani et al.[8] Greater reduction of mean VASI score was seen in the age-group of 18–30 years as compared with the age-group of 30–50 years in either of the groups studied by us. A possible explanation for this greater response to therapy by the patients of the younger age-group in both the treatment arms could be due to two reasons. First, there is a decline in the number and function of melanocytes with advancing age in human skin. The number of dopa-reactive melanocytes tends to decrease with age by approximately 10%–20% every decade in both sun-exposed as well as non-sun-exposed human skin.[10] Second, oxidative stress causes amassing of reactive oxygen species (ROS) intraepidermally in the vitiliginous patches, and the amount of ROS increases with age.[1112]
The duration of lesional stability did not influence the treatment outcome in any of the groups. This finding could not be compared with other studies as no conclusive data have been published in the literature to date to the best of our knowledge.
Hélou et al.[4] showed an effective response by FCO2 laser followed by sun exposure, and proposed it to be an alternative treatment modality for NSV specifically in sunny regions. Shin et al.[13] and Doghaim et al.[14] carried out treatment with FCO2 laser followed by Narrow Band- Ultraviolet B. (NB-UVB) phototherapy for recalcitrant NSV, and they concluded this combination to be an effective and safe treatment modality. Li et al.[15] and Yuan et al.[16] used FCO2 laser, topical betamethasone, and NB-UVB phototherapy for refractory NSV. Both studies found this triple combination on refractory NSV to be safe and effective. Yuan et al.[16] found an ablative CO2 laser more effective than a nonablative fractional laser. Cunha et al.[17] used FCO2 laser, topical betamethasone, and salicylic acid safely and effectively for refractory vitiligo. Chen et al.[18] reported a response to FCO2 laser combined with tacrolimus in the progressive vitiligo cases. Mohamed et al.[19] concluded the use of CO2 laser skin ablation, followed by 5FU application for acral vitiligo is a safe and tolerable technique. However, El-Zawahry et al.[20] failed to show any noteworthy superior response of combined treatment with FCO2 laser with NB-UVB phototherapy over NB-UVB phototherapy alone. Our study supports the use of FCO2 laser as an adjuvant therapeutic modality to topical PUVA-sol.
Several theories can be attributed to the possible mechanism of action of FCO2 laser in vitiligo. First, FCO2 laser causes immediate retraction of the tissues and denaturation of the collagen bundles resulting in a narrowed vitiligo lesion.[4] Second, when FCO2 laser is extended in the surrounding normal skin, it causes migration of melanoblasts from the outer root sheath of the hair follicles present there to the vitiliginous area.[4] Finally, FCO2 laser causes local tissue damage, which can lead to an epidermal inflammatory response. This causes local inflammation and thus the proliferation of melanocytes on the affected skin such as the mechanism of post-inflammatory pigmentation.[18]
PRP is a plasma fraction that contains 3–5 times higher concentration of platelets relative to the whole blood.[21] PRP contains growth factors such as Platelet Derived Growth Factor (PDGF), Transforming Growth Factor- Beta (TGF-β), Epidermal Growth Factor (EGF), Vascular Endothelial Growth Factor (VEGF), Insulin Growth Factor (IGF), Fibroblast Growth Factor (FGF) that are stored in alpha granules of the platelets along with numerous plasma proteins such as fibrin, fibronectin, and vitronectin. These growth factors help in the repair and regeneration of the tissues.[6] PRP possibly stimulates the proliferation of keratinocytes and fibroblasts with subsequent enhanced interaction with melanocytes, resulting in the stabilization of melanocytes.[6] Another advantage of treatment with PRP is the induction of escalated proliferation and migration of fibroblasts through the upregulation of cyclin E and cyclin-dependent kinase 4, which is crucial for migration and proliferation of cells.[6] PRP also limits the release of cytokines by its anti-inflammatory action.[7]
Mahajan et al.[6] found patients not responding adequately to traditional therapies can be treated with intralesional injections of PRP. Ibrahim et al.[5] concluded that a combination of intradermal PRP along with NB-UVB phototherapy can be contemplated as an effective, uncomplicated, safe, and economical treatment modality for vitiligo. The study further justified that the use of intradermal PRP could also shorten the duration of UVB exposure and hence a decrease in the cumulate dose and enhanced patient compliance.
Our study differed from previously reported studies in two ways: First, patients in both the treatment arms were allocated the therapy only once, at the baseline visit, contrary to multiple sittings, at a time gap of 15 days–1 month in other studies. Second, patients in both the treatment arms in our study were instructed for topical PUVA-sol on the treated site, 7 days after the treatment session.
Our study found more improvement of truncal lesions as compared to limb lesions of vitiligo. We also noticed greater repigmentation on the upper limbs as compared with the lower limbs. These findings are compatible with Kadry et al.[7] where the best repigmentation was observed on the lesions on the trunk and the least on the lower limbs. Abdelghani et al.[8] also observed similar findings, where truncal lesions showed the best response followed by facial, then acral lesions, and lastly the neck lesions. Hélou et al.[4] reported the least significant improvement on the articular surfaces such as knees and elbows and axilla. Trunk lesions show better response in comparison with the limb and acral areas because the areas over bony prominences and acral sites contain less density of hair follicles, the reservoir for melanocytes, and also due to the thick skin present there.[14]
The finding of this study is compatible with the finding in a study by Kadry et al.[7] where combination treatment with FCO2 laser and PRP achieved the best repigmentation, followed by PRP-only group, and least repigmentation was observed in FCO2 laser–only group. Results of the study conducted by Abdelghani et al.[8] where the combination therapy with FCO2 laser and PRP worked better than the FCO2 laser monotherapy, were also accordant with our study. They further concluded both FCO2 laser and PRP injection produced poor results when received as monotherapy. We further observed that maximum repigmentation was observed at second follow-up visit (60 days after treatment session). A hypothesis to this finding could be the peak synergistic effect of PUVA-sol, attaining saturation at the second follow-up visit. This also justifies the role of another sitting of FCO2 laser to stimulate the peripheral and perifollicular keratinocytes and melanocytes.
The secondary objective of our study was to compare the safety profiles between patients treated with FCO2 laser combined with PRP and FCO2 laser alone.
In our study, all the patients in both the treatment arms experienced mild to moderate pain after therapy session, whereas 76.6% of patients in Group A and 100% patients in Group B complained about burning sensation as seen by Mahajan et al.,[6] Kadry et al.,[7] and Doghaim et al.[14] However, pain and burning sensation subsided within a day and erythema as well as crusting within a week after laser treatment in our study, and they did not affect the course of the treatment. No patient dropped out in our study due to adverse events.
Other adverse effects observed in our study were erythema and crusting, both were greater in Group B than Group A. The presence of aforementioned side effects was also reported by Doghaim et al.[14] None of the patients in either treatment arms witnessed scarring, infection, Koebnerization, and aggravation of vitiligo similar to study by Yuan et al.[16] A hypothesis about the combination of PRP along with FCO2 laser producing fewer side effects in terms of erythema, burning sensation, and crusting than FCO2 laser alone, could be due to anti-inflammatory effects exerted by PRP.
Limitations: Long-term follow-up could not be conducted in the patients, to observe the stability of the repigmented patches.
We could not compare the two treatment arms with the third arm containing PRP alone.
CONCLUSION
A combination of FCO2 laser with autologous intralesional PRP was found to be more efficacious in terms of higher mean VASI score reduction and greater repigmentation in comparison with treatment with FCO2 laser as monotherapy. Younger age patients repigmented better compared to the older age-groups. Trunk lesions repigmented better than limb lesions, and upper limb lesions responded better than lower limb lesions.
In terms of side effects, the combination therapy fared better in the form of lesser adverse events such as erythema, burning sensation, and crusting mostly due to the anti-inflammatory and healing property of PRP.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Acknowledgement
We acknowledge Mr. P. K. Brahma for his help for his contribution in statistical evaluation of the study.
REFERENCES
- Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;345:426-38.
- [Google Scholar]
- Fractional carbon dioxide laser as an “add-on” treatment for vitiligo: a meta-analysis with systematic review. Acta Derm Venereol. 2018;98:180-4.
- [Google Scholar]
- Fractional laser for vitiligo treated by 10,600 nm ablative fractional carbon dioxide laser followed by sun exposure. Lasers Surg Med. 2014;46:443-8.
- [Google Scholar]
- The effect of platelet-rich plasma on the outcome of short-term narrowband-ultraviolet B phototherapy in the treatment of vitiligo: a pilot study. J Cosmet Dermatol. 2016;15:108-16.
- [Google Scholar]
- Effect of intralesional platelet rich plasma in chronic localized vitiligo. Int J Res Dermatol. 2018;4:550-5.
- [Google Scholar]
- Platelet-rich plasma versus combined fractional carbon dioxide laser with platelet-rich plasma in the treatment of vitiligo: a comparative study. Clin Cosmet Investig Dermatol. 2018;11:551-9.
- [Google Scholar]
- Combined treatment with fractional carbon dioxide laser, autologous platelet-rich plasma, and narrow band ultraviolet B for vitiligo in different body sites: a prospective, randomized comparative trial. J Cosmet Dermatol. 2018;17:365-72.
- [Google Scholar]
- Vitiligo: compendium of clinico-epidemiological features. Indian J Dermatol Venereol Leprol. 2007;73:149-56.
- [Google Scholar]
- Effects of aging and chronic sun exposure on melanocytes in human skin. J Invest Dermatol. 1979;73:141-3.
- [Google Scholar]
- Epidermal H(2)O(2) accumulation alters tetrahydrobiopterin (6BH4) recycling in vitiligo: identification of a general mechanism in regulation of all 6BH4-dependent processes? J Invest Dermatol. 2001;116:167-74.
- [Google Scholar]
- Combination treatment by 10,600 nm ablative fractional carbon dioxide laser and narrowband ultraviolet B in refractory nonsegmental vitiligo: a prospective, randomized half-body comparative study. Br J Dermatol. 2012;166:658-61.
- [Google Scholar]
- Combination of fractional carbon dioxide laser with narrow band ultraviolet B to induce repigmentation in stable vitiligo: a comparative study. J Cosmet Dermatol. 2019;18:142-9.
- [Google Scholar]
- Triple combination treatment with fractional CO2 laser plus topical betamethasone solution and narrowband ultraviolet B for refractory vitiligo: a prospective, randomized half-body, comparative study. Dermatol Ther. 2015;28:131-4.
- [Google Scholar]
- Fractional CO2 lasers contribute to the treatment of stable non-segmental vitiligo. Eur J Dermatol. 2016;26:592-8.
- [Google Scholar]
- New approach in the treatment of refractory vitiligo: CO2 laser combined with betamethasone and salicylic acid solution. Dermatol Ther. 2017;30:1-4.
- [Google Scholar]
- Preliminary study on the treatment of vitiligo with carbon dioxide fractional laser together with tacrolimus. Lasers Surg Med. 2018;50:829-36.
- [Google Scholar]
- Carbon dioxide laser plus topical 5-fluorouracil: a new combination therapeutic modality for acral vitiligo. J Cosmet Laser Ther. 2015;17:216-23.
- [Google Scholar]
- Effect of combination of fractional CO2 laser and narrow-band ultraviolet B versus narrow-band ultraviolet B in the treatment of non-segmental vitiligo. Lasers Med Sci. 2017;32:1953-8.
- [Google Scholar]
- Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med. 2009;37:2259-72.
- [Google Scholar]






