Translate this page into:
Fractional CO2 Laser-induced Delivery of Topical Corticosteroids Hastens Resolution of Localized Plaque Sarcoidosis
Address for correspondence: Dr. Aayush Gupta, Department of Dermatology, Dr. D.Y. Patil Medical College, Hospital and Research Centre, Pune, Maharashtra, India. E-mail: aayushggupta@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Sarcoidosis, an inflammatory disorder, is characterized histopathologically by non-caseating granulomas in one or more organ systems,[1] most commonly lungs, lymph nodes, and skin. Skin lesions are the initial manifestation in almost one-third of patients with sarcoidosis.[2] Various types of cutaneous sarcoidosis exist; the most common, acute maculopapular type, has a favorable prognosis. On the contrary, plaque sarcoidosis––which develops mostly on the back, buttocks, face, and extensor extremities––is associated with chronic disease, presenting a variable response to the standard therapies.[1] Furthermore, powerful immunosuppressive treatments such as methotrexate and biologics have inherent side effects, including long-term risks of infection, hepatotoxicity, and potential malignancy.[3] Light and laser therapies are promising alternatives for therapy-resistant cases. Herein we present a case of localized plaque-type sarcoidosis treated successfully with fractional carbon dioxide laser (CO2) and topical steroids.
A 38-year-old Indian man presented with a single localized asymptomatic indurated plaque over the left knee [Figure 1A] since 3 years. It was gradually progressive, despite multiple treatments taken intermittently including topical and oral steroids. There were no systemic complaints or any history of trauma. Histopathological examination revealed mild acanthosis, elongated rete ridges, and superficial dermal epithelioid granulomas surrounded by scanty lymphocytes [Figure 1C and D]. Fite faraco- and PAS stain were negative; chest CT was normal. Except for raised serum ACE levels (67.32 U/L, normal: 8–52 U/L), other biochemical tests, including serum calcium, were normal. Diagnosed as a case of localized plaque sarcoidosis, the patient was given fractional CO2 laser therapy (18 mJ, 0.6 mm distance, overlap 4) under topical anesthesia to make microchannels, as a means of drug delivery for topical corticosteroids. Immediately after lasing, clobetasol acetate cream was applied under occlusion and the patient was advised to apply the same twice daily till the next session. A total of four sessions were done fortnightly. Follow-up after 6 months revealed mild atrophy, subtle hypopigmentation, and minimal induration over the borders of the lesion which had now stopped progressing [Figure 1B]. The satisfied patient declined to continue further therapy or a repeat biopsy.
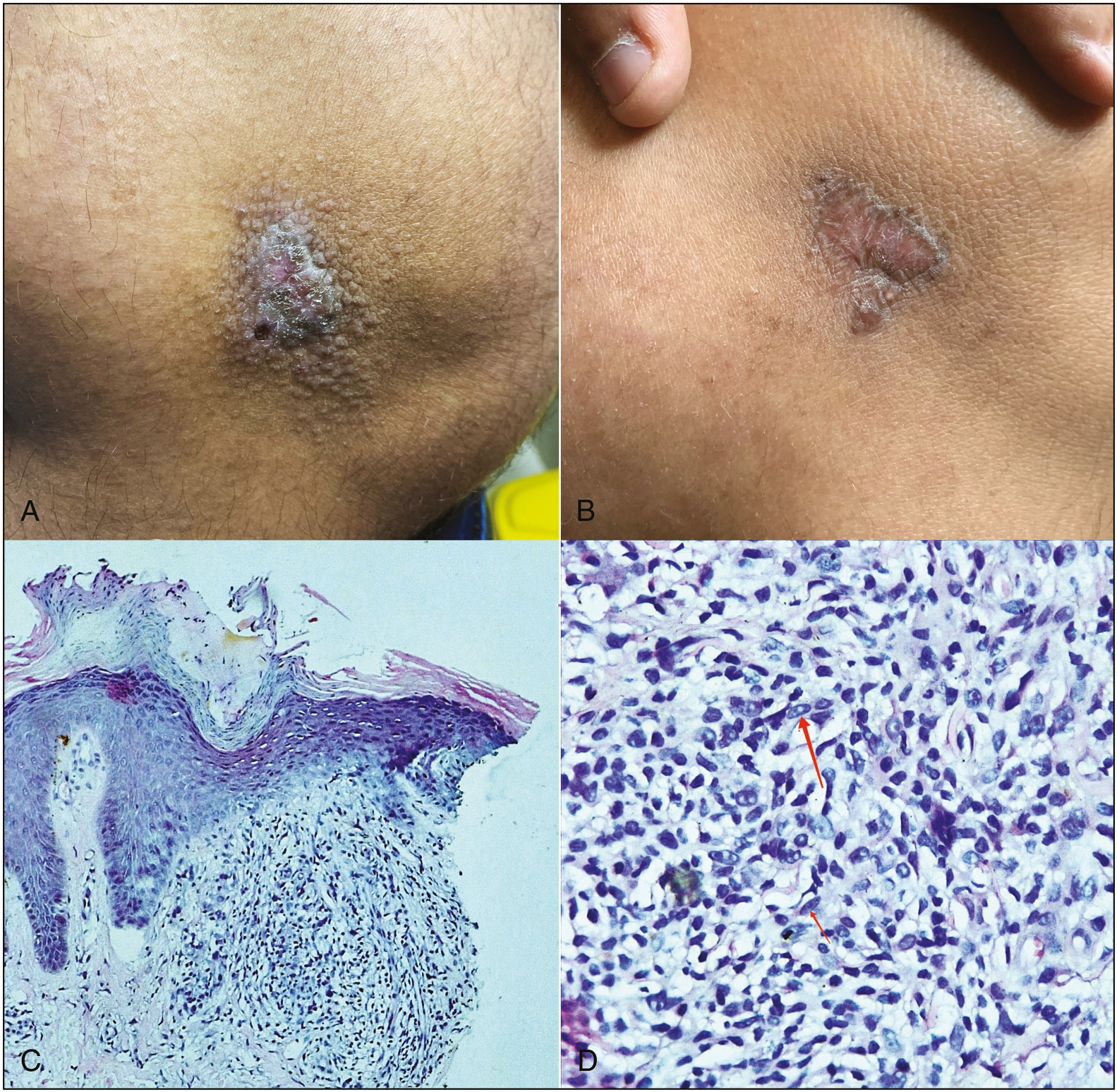
- (A) Solitary, 2 cm x 1 cm, reddish-brown plaque with minimal scaling over medial aspect of left knee surrounded by skin colored micropapules. (B) Erythematous, atrophic plaque with hyperpigmented margins after 4 weeks of treatment. (C) Mild acanthosis and elongation of rete ridges, superficial dermis shows multiple well-formed epitheloid granulomas with surrounding lymphocytes (hematoxylin and eosin, 100x). (D) Well-formed epitheloid granulomas with surrounding lymphocytes (hematoxylin and eosin, 400x)
Though many therapies have been extensively used for cutaneous sarcoidosis, few have been evaluated in randomized trials. Although topical corticosteroids are generally considered to be beneficial for skin lesions, evidence thereof is scant. Intralesional injections of triamcinolone acetonide (3–20 mg/mL) repeated every 3–4 weeks, may increase efficacy by better delivery of the drug to the reticular dermis. Use of fractional CO2 laser as a treatment modality of plaque sarcoidosis has not been previously reported. Three previous case series[345] using ablative CO2 laser resurfacing for treating grossly disfiguring lupus pernio refractory to medical therapy reported excellent post-operative responses which were maintained for many subsequent years. It is noteworthy that ablative CO2 laser procedures described in the aforementioned case series, like ours, served only to recontour rather than excise all of the abnormal tissue. Fractional CO2 serves to ablate the diseased tissue along with hastening the dermal delivery of steroids by creating microchannels and thus should be looked at as an effective treatment modality for localized cutaneous disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Not applicable.
Conflicts of interest
There are no conflicts of interest.
References
- Sarcoidosis: A comprehensive review and update for the dermatologist: Part I. Cutaneous disease. J Am Acad Dermatol. 2012;66:699.e1-18; quiz 717-8.
- [Google Scholar]
- CO2 laser vaporization for disfiguring lupus pernio. J Cosmet Laser Ther. 2002;4:87-90.
- [Google Scholar]





